GENERAL PRINCIPLES
advertisement

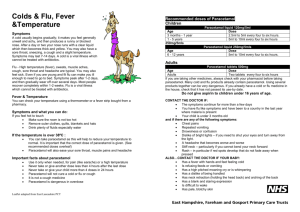
GENERAL PRINCIPLES N.B. This document is intended for use primarily in the peri-operative setting. 1. Prevention is better than cure: it is important to maintain analgesia with regular dosing, rather than waiting for severe pain and trying to treat this. 2. The dosages in this guide assume that children are healthy (ASA 1 or 2). It excludes: Neonates Children aged < 6 months Children with hepatic or renal impairment Children with significant CNS disease Children with significant respiratory depression 3. It is best to provide a balanced approach to analgesia e.g. intra-operative local anaesthetic +/- simple analgesic +/- opioid. Simple Analgesics– PLEASE ALWAYS PRESCRIBE THIS FOR EVERY CHILD BEFORE THEY LEAVE THEATRE e.g. paracetamol, NSAIDs Non-narcotic, non-addictive, non-sedative Suitable for mild to moderate pain Generally oral or rectal administration Reduce post-operative opioid requirements Opioid Analgesics e.g. morphine May be administered orally, subcutaneously or I.V. (intermittent bolus or PCA) N.B. IM administration should be avoided where possible as this is distressing for the child Main side-effects include: Respiratory depression Drowsiness Nausea and vomiting Delayed gastric emptying N.B. Addiction does not occur in short-term analgesic setting 1 SIMPLE ANALGESICS PARACETAMOL Paracetamol may be used alone after minor procedures, or given concurrently with an opioid after more major procedures. It also has an antipyretic action. It can be given rectally, but absorption is slow and bioavailability is poor by this route. It is a very safe drug (caution in liver disease) and may be used in neonates. Acute overdose is often due to error in dose calculation. Over-dose may cause liver damage, sometimes undetectable for several days. TOXICITY is usually due to chronic use => limit use to 5days; limit to 3 days if liver disease, viral illness, or age < 3 months. Formulations: Tablets - 500mg (also soluble) Suspension – 120mg /5mls, 250mg /5mls Suppositories - 60mg, 120mg, 240mg, 500mg (refrigerated) *Intravenous (Perfalgan) – 500mg or 1g vials (10mg/ml) DOSE Loading Dose : oral 20 mg/kg : pr 40 mg/kg : loading dose not recommended for i.v. administration Maintenance : (any route) 15 mg / kg 4-6 hourly Maximum 90 mg/kg in 24h (maximum 60mg/kg/day i.v.) Review dosage after 72h. Neonates : Restrict loading dose to 20mg / kg Increase dosing interval 8-12h Maximum dose 60 mg/kg in 24h. Review dosage after 48h. *Notes on intravenous paracetamol: Not recommended in children and infants <10 kg i.v. paracetamol dose to be infused over a period of 15 minutes 2 NSAIDS: Analgesic Anti-inflammatory Side-effects include gastric irritation, renal failure, exacerbation of asthma and occasionally post-operative bleeding. AVOID in Severe asthma (i.e. child who has required hospitalisation for asthma, or who is taking oral steroids) Renal failure Infants <1 year (renal immaturity) Coagulopathy or bleeding disorder (GI ulcer) Aspirin is contra-indicated in children <12y due to rare but serious complication of Reye’s Syndrome DICLOFENAC Formulations: Suppositories – 12.5mg, 25mg, 50mg, 100mg Dispersible tablets – 50mg EC tablets – 25mg, 50mg DOSE 1 – 3 mg per kg per dose (Oral: 1mg/kg 8hourly) Maximum 3mg / kg in 24 hours (maximum 150mg / day) KETOROLAC (IV) 0.5 – 1.0 mg/kg (max 15mg), followed by bolus injections of 0.5 mg/kg 6 hourly The maximum daily dosage is 90mg, and the maximum duration of treatment is 48 hours. IBUPROFEN This may be preferable to diclofenac for oral administration as it is available as a suspension Formulations: (oral only): Suspension – 100mg / 5ml Tablets - 200mg, 400mg DOSE 10 mg / kg 8hourly or 5 mg / kg 6 hourly PIROXICAM - FELDENE MELT (20mg tablets) licenced for 16year olds but licenced for juvenile arthritis at 6years once daily administration 0.4 mg / kg 3 OPOID ANALGESICS effective in moderate to severe pain. Opioid requirements are decreased by the concomitant use of simple analgesics (though opioid side-effects may still be evident) Main side-effects include: Respiratory depression Nausea and vomiting Delayed gastric emptying, constipation Drowsiness Avoid use in head injury or raised intracranial pressure (may cause respiratory depression, pupillary constriction) 1. Oral Formulations DIHYDROCODEINE (DF118) Not to be used for children under one year or those with (potential) respiratory depression. Formulations: Elixir – 10mg / 5ml Tablets – 30mg DOSE 1 - 4 years = 0.5 mg / kg 6 hourly 4+ years = 0.5 - 1 mg / kg 6 hourly (max dose = 30mg) ORAMORPH Oral solution of morphine sulphate. May be used in severe pain in children provided oral intake is adequate (e.g. not suitable immediately post-op appendicectomy / trauma etc until oral intake re-established). DOSE 0.3 mg / kg 4hourly monitor Spo2 if 2nd dose required CODEINE PHOSPHATE Recently there has been concern that Codeine could cause respiratory depression in children who are rapid metabolisers. We now avoid using codeine in children who will not be observed in hospital. Oramorph at a dose of 0.1 – 0.2mg/kg is a suitable alternative to oral codeine in the post-operative period. 4 PARENTERAL ANALGESICS MORPHINE Morphine is an opioid analgesic used to control severe pain in children. It should be avoided in neonates if possible and used with caution in children under 6 months (consider apnoea monitor, esp. in ex-prem) Morphine can be given by IV bolus or PCA. Subcutaneous administration is no longer recommended. All children receiving systemic opioids should be monitored closely. IV bolus: 0.1 – 0.2 mg / kg 2 hourly ( 0.05 mg / kg as bolus if IV morphine infusion running) PCA: N.B. Dedicated cannula or anti-reflux valve required Suitable for cooperative children 6y+ Child, parents and nursing staff should all understand principles! Dilution : child’s body weight (kg) in mg diluted in 50ml normal saline (20 micrograms / kg / ml) PCA bolus = 0.5 –1ml (10 – 20 mcg / kg); lockout 5 minutes Consider background 0.2 ml/h (4 mcg/kg/h); background infusion should only be used in a high-dependency area. IV Infusion: this should only be used in a high-dependency area and should be avoided if at all possible. N.B. Dedicated cannula or anti-reflux valve required Infusion rate : 0.5 – 2 ml/h (= 10 – 40 micrograms / kg / h) IM injections may be distressing to children and should be avoided where possible. IM dosage: Up to 1 year : 0.2 mg / kg 4hourly Over 1 year : 0.2 – 0.4 mg / kg 4hourly 5 TRAMADOL HYDROCHLORIDE Tramadol is not licensed for children under the age of 12 years. DOSAGE 12 – 18 years = 50 – 100 mg q 4h oral or i.v. OPIOID ANTAGONIST = NALOXONE Dose = 2-10 mcg/kg bolus. Repeat every 60sec as required. Infusion = 10mcg/kg/h. If no i.v. access, IM dose = 100mcg/kg 6 Nausea and Vomiting Minimise opioid use (e.g. LA use, NSAID, paracetamol) Anti-emetics are not prescribed routinely in children due to an increased risk of extrapyramidal side-effects (e.g. oculogyric crisis) Newer anti-emetics e.g. ondansetron and dexamethasone may have an improved safety profile Children > 12y can use adult anti-emetic regimens Anti-emetics should be administered systemically rather than orally whenever possible Combination therapy intra-operatively is more effective than single agent use Post-operative anti-emetics should be given for treatment of persistent postoperative nausea and vomiting which is severe enough to prevent the ingestion of oral analgesics or fluids. Anti-emetics 1. ONDANSETRON 0.1 mg / kg by slow IV injection (maximum 4mg) 8 hourly prn 2. DEXAMETHASONE 0.15 – 0.25 mg/kg by slow IV injection (maximum 8mg) intra-op. 3. PROCHLORPERAZINE Formulations: Suppositories – 5mg, 25mg (Syrup – 5mg / 5ml) DOSAGE 0.25 mg/kg pr (to the nearest 5mg) ( oral dose 0.25 mg/kg) 4. METOCLOPRAMIDE To be administered by slow IV injection: <1y (10kg) 1mg 12h 1 – 3y (10 – 14kg) 1mg 8h 3 – 5y (15 – 19 kg) 2mg 8h 5 – 9y (20 – 29kg) 2.5mg 8h 9 – 14y (30kg+) 5mg 8h 14y+ (60kg+) 10mg 8h 7 REFERENCES 1. Postoperative Analgesia Protocols: Royal Hospital for Sick Chidren, Edinburgh (Dr. E. Doyle) 2. Paediatric Acute Pain Protocols: Royal Hospital for Sick Children, Yorkhill, Glasgow (Dr. N. Morton, S/N S. Aitkenhead) 3. Howell, TK. Paracetamol use in Children. Care of the Critically Ill 1999; 15: 208-213 4. Howell, TK. What we should know about paracetamol. Paediatric Anaesthesia 1999; 9: 367 5. Korpela R, Olkkola KT. Paracetamol – misused good old drug? Acta Anaesthesiologica Scandinavica 1999; 43: 245-247 6. Birmingham PK et al. Twenty-four-Hour Pharmacokinetics of Rectal Acetaminophen in Children. Anesthesiology 1997; 87: 244-252 7. Howell, TK. Post-operative Pain Relief: Doing Simple Things Better. (lecture and report) Seventh Annual Paediatric Anaesthesia Update, Manchester, Jan 2000 8. Ward B, Alexander-Williams JM. Paracetamol revisited. Acute Pain 1999; 2: 139-149 9. Morton NS. Prevention and control of pain in children. British Journal of Anaesthesia 1999; 83: 118-129 10.Pain in children. Acute Pain Management: scientific evidence. P93-108 (source: http://www.health.gov.au/nhmrc/publicat/pdf/cp57.pdf) 8 APPENDIX Suggested Analgesic Regimens for some Common Procedures These suggestions are for guidance only. It is up to the individual clinician to decide upon the most appropriate regimen for each patient. A balanced analgesic regimen is ideal e.g. intra-operative opioid plus supplementation with pr NSAID plus local anaesthetic technique if appropriate. If NSAIDs are contra-indicated, consider the use of i.v. paracetamol intraoperatively. Caudal analgesia: the usual dose is 0.8 – 1ml/kg of 0.25% bupivacaine (maximum dose 20ml). The use of additives; It is up to the individual to decide whether or not to add an adjunct to the caudal in order to increase duration of action e.g. Clonidine 2 microgrammes/kg We DO NOT recommend Ketamine due to concerns about neurotoxicity Step-Down Analgesia This may be required after procedures where the child has been prescribed parenteral opioids post-operatively e.g. PCA morphine. Always prescribe a simple analgesic in addition to the opioid e.g. paracetamol or NSAID Never prescribed oral opioid (e.g. dihydrocodeine) at the same time as parenteral opioid Oral opioid (e.g. dihydrocodeine) may require to be prescribed when PCA is removed. 9 Intra-op: Post-op: To Take Away (TTA): Intra-op: Post-op: Intra-op: Post-op: Intra-op: Post-op: Tonsillectomy Fentanyl (~2/3 - 1 mcg/kg) + morphine (~0.05 mg/kg) + IV paracetamol + NSAID (oral ibuprofen premed or pr voltarol) Paracetamol + ibuprofen + oramorph 0.1 - 0.2 mg/kg prn + ondansetron prn Paracetamol + ibuprofen + difflam spray + dihydrocodeine We are planning on also giving them a few doses of oramorph TTA (o.1 - 0.15 mg/kg). Pharmacy arrangements need to be finalised Circumcision Caudal or penile block Lignocaine gel or EMLA cream TTA Paracetamol plus ibuprofen TTA Inguinal hernia Caudal or ilio-inguinal block or LA infiltration Paracetamol plus ibuprofen TTA Appendicectomy, Laparotomy IV morphine Plus LA infiltration, TAP Block or wound catheter Plus pr diclofenac or IV Ketorolac PCA morphine (>6y with good understanding) Plus paracetamol (oral or i.v.) Intra-op: Post-op: Orthopedics e.g. MUA, ORIF Diclofenac +/- Fentanyl where appropriate Plus LA infiltration where appropriate Paracetamol plus ibuprofen +/- dihydrocodeine / oramorph if appropriate 10