Flexibility is the key to managing cancer pain
advertisement

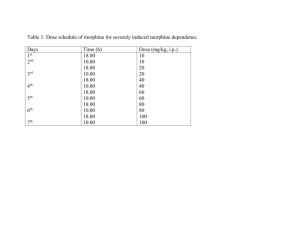
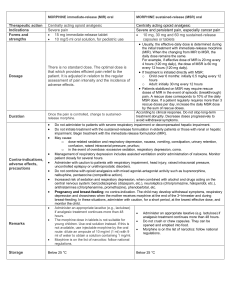
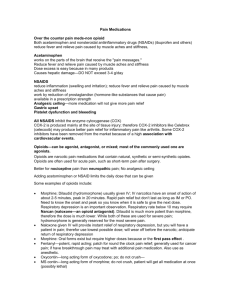
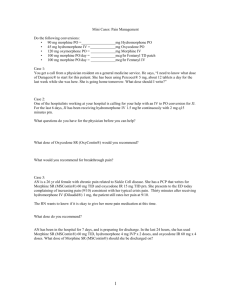
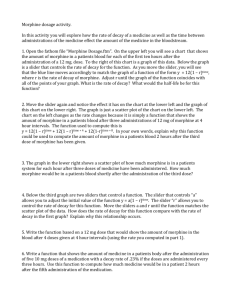
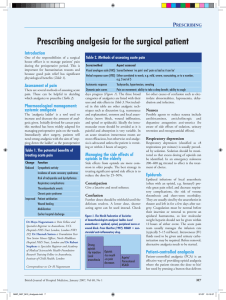
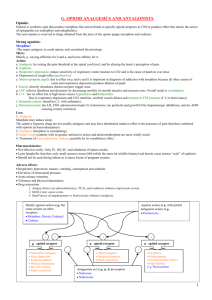
Cancer Pain Management DR. PRADEEP JAIN Sr. Consultant Department of Anaesthesiology, Pain & Perioperative Medicine Sir Ganga Ram Hospital New Delhi - 110 060 Global Crusade Against Pain Chronic Pain is a Disease State Global Crusade Against Pain Chronic Pain is a Disease State NURSING PHARMACY physician Pain Management A Team Approach SPIRITUAL GUIDANCE SOCIAL WORKER CASE MANAGER PHYSICAL REHAB DIETICIAN Pain Management Children with cancer do not need to suffer unrelieved pain Effective pain management and palliative care are major priorities of the WHO cancer programme, together with primary prevention early detection & treatment of curable cancers Analgesic therapies are essential in controlling pain and should be combined with appropriate psychosocial, physical & supportive approaches Pain in Cancer In the developed world, the major sources of pain in children’s are due to diagnostic and therapeutic procedures. In the developing world, most pain is disease related Why to Relieve Pain CHILDREN Irritable, anxious & restless in response to pain Develop mistrust & fear of hospitals, medical staff and treatment procedures Experience night terrors, flashbacks, sleep disturbance and eating problem Children with uncontrolled pain may feel victimized, depressed, isolated ,lonely and their capacity to cope with cancer treatment may be impaired Why to Relieve Pain PATIENTS AND CLOSE RELATIVES Distrustful towards the medical system Experience depression & guilt about being unable to prevent the pain HEALTH CARE WORKERS It numbs their compassion, creates guilt Encourages denial that children are suffering Management Strategies Assess the child Conduct physical examination Determine primary cause of pain Evaluates secondary causes (environmental and internal ) Develop treatment plan Analgesic drugs and non analgesic therapies Implement Plan Assess regularly and revise plan as necessary Pain Assessment • QUESTT Q – Question the child U – Use pain rating scales E – Evaluate child’s behavior S – Secure parent’s involvement T – Take cause of pain into account T – Take earliest action Pain Assessment PRE VERBAL - Physiological changes - Behavioral response –facial expression, body movement and type of cry PRE-SCHOOLERS The various self-reporting scales are: –The Oucher Scale –Happy-Sad Face Scale –Eland’s Colour Scale –Poker Chip Tool –Ladder Scale –Linear Analogue Scale SCHOOL AGED CHILDRENS VAS and modified Mcgill Pain Questionnaire Neonatal Pain Assessment Scale Krecheal SW, Bildner J CRIES: a new neonatal postoperative pain management score. Initial testing of validity and reliability. Pediatric Anesthesia 1995;5:53-61 Pain Assessment Scales The Wong Baker Scale 0 10 No Pain Max. Pain VAS Approach to pain management Flexibility is the key to managing cancer pain Placebo should not be used in management of cancer pain Drug treatment is the main stay in cancer pain management Effective (70 - 80%) Inexpensive Non Opioid Drugs • Mild to moderate pain • Adjunct to balanced pain management • Pharmacokinetics similar in infants aged over 6 months to adults • Very little efficacy & safety data for infants available • Paracetamol - tablet, syrup, suppositories dose 10-15mg/kg orally 6 hr • Ibuprofen - tablet, syrup dose 10-20mg/kg orally 6 hr • Diclofenac - orally 1mg/kg 8-12 hr • Ketarolac - i/v 0.2-0.5 mg/kg Morphine Name derives from the Greek, Morpheus, the God of dreams, while opium is the Greek word for juice. Oldest analgesic known to man Land mark in the development of pain control Dried exudate of the opium poppy ‘’ papaver somini ferum”. Guidelines for Analgesic Drug Therapy “By the ladder” “By the clock” “By the appropriate route” “By the child” “By the ladder” Morphine in Cancer Pain Management “By the clock” at fixed interval of time dose titrated against the patients pain - gradually increasing until the patient is comfortable next dose before the effect of previous dose worn off prn means pain relief negligible making patients earn their analgesia is as unacceptable as making diabetic earn their insulin Morphine in Cancer Pain Management “By Mouth” Treatment of choice Tablets every 4 hourly Slow release tablets MST - 12 hourly MXL - 24 hourly A simple aqueous solution of the sulfate or hydrochloride salt every 4 hours Morphine in Cancer Pain Management “By The Child ” No standard doses. No fixed upper dose limit (analgesic celing effect) The “right” dose is the dose that relieves the pain Range 5mg to >1000 mg Morphine Drug of choice Oral, S/C, I/V, rectally, epidural and Intrathecal Oral dose Intermittent I/V 50-100 g /kg Continuous I/V or S/C 15-30 g /kg/h Controlled release oral preparation < 6 months of age dose decrease to 1/3 0.15 –0.3mg/kg every 4 hour Fentanyl More potent then morphine Hepato-renal compromise < histamine release Muscular rigidity Only opioid with transdermal preparation Oral Trans mucosal preparation Sufentanyl nasal spray, Aerosol preparation Pediatric Cancer Pain Management Adjuvant drugs May be necessary for one of the three reasons: To treat the adverse effects of analgesic: To enhance pain relief To treat concomitant psychological disturbances: Intrathecal Drug Delivery Morphine most commonly used Epidural or Intrathecal administration Epidural percutaneous catheter Tunneled subcutaneous catheter Procedure Related Pain General Principles Prophylaxis should involve both pharmacological and non pharmacological approaches The specific approaches used should be tailored to the individual Children must be adequately prepared for all invasive and diagnostic procedures To be done in specially designated treatment rooms Algorithms for Pain Management During Procedures PAINLESS PROCEDURE (CT, MRI) Individualized preparation chloral hydrate 1 hour before procedure Pentobarbital MILD PAINFUL PROCEDURE (I/V CANNULATION) Parental presence Local anaesthetics – Topical anaesthetics – Buffered lidocaine Behavioural techniques e.g. bubble-blowing, distraction Algorithms for Pain Management During Procedures MODERATELY PAINFUL PROCEDURE (L.P.) Benzodiazepines SEVERE PAINFUL PROCEDURES (B.M ASPIRATION, BIOPSY) No venous access – oral midazolam with morphine, I/M Ketamine Venous access – midazolam with fantanyl, morphine,Ketamine, propofol and N2O GA Oral Transmucosal Fentanyl Sedation 100,200,300 ug Dose:10-15ug/kg Onset 20 mins Nausea/vomiting common EMLA Application 1. 1. Applying: Don’t rub the cream 2. Covering: Allow a thick layer 3. Timing: Let it be undistributed 4. Removing: 60 min after application 2. 3. 4. Nitrous Oxide Analgesia Provide good analgesia, sedation and amnesia without resulting in loss of consciousness known as relative analgesia Bone marrow aspiration, lumbar, puncture, venous cannulation and wound dressings Administration – Demand system (entonox ) – Constant flowdevices (quantiflex apparatus/ anaesthesia machine) Programmable Electronic Devices • Interfaced with microprocessor • Flexibility in programming • Comprehensive display & memory of events • Security features prevent tempering • Event log • Multiple application Disposable Fixed Programme Devices • Light weight - Maximum portability • Non Electronic - No programming • Hydrostatic positive pressure Elastomeric energy • Flow restrictor - Flow rates are preset • Simplicity • Minimal patient & nursing training PEDIATRIC PO PAIN RELIEF PCA Morphine loding dose 50 g/ Kg Infusion rate 15 g/ Kg/ hr PCEA Bupivicaine Bolus 0.5 ml/ Kg ( 0.25% ) Infusion rate - ( 0.125% ) 0.1 - 0.5 ml/ Kg / hr Fentanyl 2 g/ ml + 0.125% Bupivicaine - 0.1 - 0.5 ml/ Kg / hr Morphine 20 - 50 g/ Kg Non Drug Pain Therapy Supportive Support and empower the child and family Cognitive Influence thought Behavioural Changes behaviour Physical Affects sensory system Integral Part of Cancer Pain Treatment Cancer Pain Freedom from pain should be seen as a right of every cancer patient and access to pain therapy as a measure of respect of this right Conclusion Nothing would have a greater impact on the quality of life of children with cancer than the dissemination and implementation of the current principles of palliative care, including pain relief & symptom control SGRH Thank You….