AML - Lafmeded.org
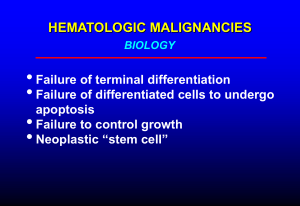
advertisement
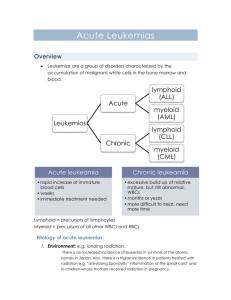
Diagnosis and Management Of Acute Leukemia in Children and Adolescents Grand Rounds September 20, 2010 St. Elizabeth Hospital, Lafayette, Indiana Bassem. I. Razzouk, MD, FAAP Medical Director, St. Vincent Children’s Center For Cancer & Blood Diseases Pediatric Cancer Incidence USA Year Population Incidence New cases < 20 yrs per 105 per year 1998 72,935,000 16.7 12,183 1999 73,120,000 16.8 12,321 2000 73,306,000 17.0 12,448 Childhood Cancer Hematopoiesis PLURIPOTENT MIXED STEM CELL PROGENITOR CELL COMMITTED PROGENITOR CELL RECOGNIZABLE BONE MARROW PRECURSOR CELL BFU-E/CFU-E CFU-Eos red cell neutrophil monocyte eosinophil CFU-Baso basophil CFU-GM myeloid progenitor cell pluripotent stem cell lymphoid progenitor cell pronormoblast myeloblast monoblast MATURE BLOOD CELL CFU-Meg megakaryocyte platelet pre-T lymphoblast T-cell pre-B lymphoblast B-cell & plasma cell Myeloid Maturation myeloblast promyelocyte myelocyte metamyelocyte band neutrophil MATURATION Adapted and modified from U Va website Principles of leukemogenesis • A multistep process • Neoplastic cell is a hematopoietic pleuripotent cell or early myeloid cell • Dysregulation of cell growth and differentiation (associated with mutations) • Proliferation of the leukemic clone with differentiation blocked at an early stage Classification of Leukemias Acute Chronic Myeloid origin Acute Myeloid Leukemia (AML) Chronic Myeloid Leukemia (CML) Lymphoid origin Acute Lymphoblastic Leukemia (ALL) Chronic Lymphocytic Leukemia (CLL) Acute Leukemia • Accumulation of blasts in the marrow Epidemiology • Childhood leukemia represents 12% of all leukemias; 60% of all acute lymphoblastic leukemias • Leukemia is the most common cancer diagnosed in children at 4.3/100.000 Epidemiology • ALL/AML = 5 • Peak incidence –ALL: 2 to 5 years –AML: 1 year, increases with age • Boys > girls –T-cell 4 times greater incidence –Infant leukemia > in girls Significance of Acute Leukemia • A hematologic urgency/emergency • Usually fatal within weeks to months without chemotherapy • With treatment, moderate to high morbidity ( acute and long term) due to disease or treatment-related complications • Notify Peds H/O promptly if acute leukemia is suspected Causes of Acute Leukemias • • • • • • Idiopathic (most) underlying hematologic disorders chemicals, drugs ionizing radiation viruses (HTLV I) hereditary/genetic conditions Predisposing Factors • Genetic Syndromes – Down syndrome: 10-20 times increased incidence (600 times in megakaryoblastic type) – Bloom syndrome – Neurofibromatosis – Schwachman syndrome – Ataxia Telangiectasia – Klinefelter syndrome Ataxia-Telangactasia Predisposing Factors • Familial aggregation – Concordance in Twins • • • • • High birth weight Ionizing radiation Non-ionizing radiation (?EMF) Alcohol consumption/cigarette smoking Breast feeding has protective effect Clinical Manifestations • Symptoms due to: – marrow failure – tissue infiltration – leukostasis – constitutional symptoms: Fever, weight loss, night sweats, anorexia – other (DIC) • Usually short duration ( 4-8 weeks) Clinical Presentation Very heterogenous –Pallor –Petechiae –Hepatosplenomegaly –Adenopathy –Fever –Bony pain Clinical Presentation Sign/Symptom Fever Bleeding Adenopathy Bony pain ALL AML 34% 61% 18% 48% 50% 14% 50% 5% Infiltration of tissues/organs • Enlargement of liver, spleen, lymph nodes • Gum hypertrophy • bone pain • other organs: CNS, skin, testis, any organ Gum Hypertrophy Chloromas • Granulocytic Sarcoma (myeloblastoma) – Localized mass of primitive myeloid cells that infiltrate extramedullary sites – Involvement of every organ system has been reported Leukostasis • Accumulation of blasts in microcirculation with impaired perfusion • lungs: hypoxemia, pulmonary infiltrates • CNS: stroke • Mostly seen with WBC >> 50 x 109/L in AML and > 100 X109/L in ALL Differential Diagnosis • Juvenile Rheumatoid Arthritis- caution to use steroids / oral methotrexate before completely ruling out leukemia • Mycobacterial infections ( TB & non-TB) • Infectious mononucleosis • Aplastic anemia • Neuroblastoma • Rhabdomyosarcoma • Hypereosinophilic syndrome Laboratory Data • • • • White blood cell count: variable Hemoglobin levels: low Platelet count: low Serum chemical values – Uric Acid and LDH: elevated – Calcium: elevated • Chest X-ray: Mediastinal Mass; Preferable to do CXR with initial diagnosis of asthma, especially if you plan to use steroids • Coagulation screening: abnormal WBC < 10.000 10,000-49,000 > 50,000 53% 30% 17% Newly Diagnosed Patients with Leukemia- Work-up • Establish a diagnosis Peripheral blood and bone marrow studies Morphology Immunopathology (cell markers) Cytogenetics Molecular Genetics • Risk assessment • Protocol enrollment- patients enrolled on clinical trials have better outcome • Consent Process Bone Marrow Aspirate/Biopsy • Necessary for diagnosis: Aspirate for ALL; Aspirate/biopsy for AML • Useful for determining type • Useful for prognosis • Acute leukemias are defined by the presence of > 20% blasts (AML) or 25 % blasts (ALL) in bone marrow (% of nucleated marrow cells) Diagnosis Morphology, cytochemistry and immunophenotype Leukemia • Acute vs. Chronic • Lymphoid vs. Myeloid ALL AML Auer rods in AML Cytochemistry Lymph Myelo Mono Megak MPO + - ANB + - ANA +, diffuse +, granular Morphology/ Cytochemistry Key Points In ALL And AML • The childhood acute leukemias are a very heterogeneous group of diseases • Accurate diagnosis is important • Selection of optimal therapy is pivotal Blood Cells Immunophenotype Immunologic Classification CD3, CD7, CD10, CD19, CD79 Lymphoid Myeloid M6/M7 CD41a, CD61, and CD42b FVIII Lymphoid Vs. M0-M7 Hemoglobin Classification - ALL Immunophenotype Frequency (%) Early pre-B 57 Pre-B 25 Transitional 1 B-cell 2 T-cell 15 Classification - AML Morphology M0 M1 M2 M3 M4 (%) Morphology (%) 2 M4 19 13 M5 21 28 M6 1 6 M7 10 19 Genetics of Childhood ALL • B-lineage ALL Translocation t(12;21) t(1;19) t(4;11) t(9;22) Fusion Incidence Cure rates TEL-AML1 25% 90% E2A-PBX1 5-6% 75% MLL-AF4 2-5% 35% BCR-ABL 3-5% <30% (70 % ) with TKI’s AML-associated chromosomal abnormalities Abnormality t(8;21) inv (16) t(15;17) t(9;11) t(11;19) t(1;22) Fusion AML1-ETO CBFβ-MYH11 PML-RAR MLL-AF9 MLL-ELL Unknown FAB Incidence M2 M4Eo M3 M4,M5 M4, M5 M7 15% 8-12% 8- 10% 7% 1% 1% PROGNOSTIC FACTORS DISEASE Heterogeneity Tx Intensity Specificity Prognostic Factors - ALL • • • • • Initial white blood cell count Age at diagnosis Immunophenotype Genetic Features Extramedullary involvement ( CNS, testis) Response to therapy ALL- Risk Groups St. Jude Estimated Low Standard High 40% 50% 10% COG Standard High Very High Prognostic Factors- AML • Favorable – Age < 1 year of age – Genetics: t(15;17), inv16, t(8;21) and t(1;22) – Down syndrome • Intermediate – Genetics: normal karyotype, other 11q23 – Residual disease after induction • High-risk – Cytogenetics: -7, -5, t(6;9), complex karyotype – AML arising from MDS – Persistent disease after induction Risk Assignment • Provisional risk assignment at diagnosis • Definitive assignment at end of induction therapy after evaluation of response to early therapy is available • The objective of rigorous risk assignment is to avoid over- or undertreatment Principles of Treatment • combination chemotherapy – first goal is complete remission – further Rx to prevent relapse • supportive medical care – transfusions, antibiotics, nutrition, metabolic /electrolyte abnormalities • psychosocial support – patient and family Therapeutic Concepts in ALL • Induce a complete remission and restore normal hematopoiesis avoiding excessive toxicity • Reduce inapparent leukemia with short-term, high-dosage cytocidal therapy early in remission when the child is well and drug sensitivity is greatest • Prevent CNS leukemia (concept of sanctuary) • Use prolonged combination chemotherapy to eradicate residual disease when there is no evidence of leukemia Basic Therapy in Childhood ALL • • • • • • Induction Treatment 4-8 wk Consolidation treatment (intensification) 2-10 wk Continuation treatment (maintenance) 2-3 y Reinduction therapy (delayed intensification) 2-7 wk CNS-directed therapy 1-2 y Cessation of therapy 2.5 y for girls, 3.5 y for boys Facts about Childhood ALL • Long-term Event Free Survival ( EFS) greater than 80% • Accomplished by – Multiagent Chemotherapy – CNS-Directed Therapy – Improved Supportive Care – Trageted therapy with tyrosine kinase inhibitors ( Gleevec and others) for Philadelphia positive ALL – Treatment of adolescents and young adults ( up to 30 years) on “Pediatric Inspired protocols” Survival of ALL According to Treatment Era at St. Jude 1 XV (2000–Present) n=254 0.9 XIII–XIV (1991–99) n=465 XI–XII (1984–91) n=546 0.8 0.7 X (1979–83) n=428 0.6 0.5 V–IX (1967–79) n=828 0.4 0.3 0.2 I–IV (1961–66) n=90 0.1 0 0 5 10 15 20 25 Years from Diagnosis 30 35 40 Pediatric AML Treatment • Standard Induction Therapy • 80%-90% achieve hematologic CR • Differentiation therapy : All trans retinoic acid ( ATRA) for specific variant ; acute promyelocytic leukemia ( APL); which needs emergency treatment since patients present with bleeding • Post-remission Therapy • Historical controls suggest High dose Ara-C consolidation improves outcome • Recent data suggest 60-70% of children with matched family donors achieved cure with Allo transplant, but data is conflicting • Maintenance Therapy • No data demonstrates efficacy Results of St. Jude AML Trials 1.0 0.9 0.8 0.7 0.6 0.5 AML97 (n=40) 0.4 AML91 (n=63) AML87 (n=41) 0.3 AML80 (n=65) 0.2 AML83 (n=45) 0.1 0 0 5 10 15 Time (years) 20 25 Supportive Care • Patient stabilization – Metabolic : hydration, alkalinization, allopurinol , and occasionally Rasbruicase ( recombinant urate oxidase) for tumor lysis syndrome – Hemorrhage (DIC)- FFP, platelets – Infection- Braod spectrum antibiotics (Cefipeme) – Leukostasis- leukapheresis in AML /early therapy • Central Venous Catheter • Blood Products ( irradiated, leukoreduced, CMV negative until CMV status is known) Hematopoietic Stem Cell transplantation • Permits “rescue” from otherwise excessively toxic treatment especially in relapsed/refractory cases • Additional advantage of graft-vs-leukemia effect in allogeneic transplants • Less used for Philadelphia positive ALL, CML, and AML with tyrosine kinase inhibitors and better outcome with chemotherapy • Trade-off for allogeneic transplantation: greater anti-leukemic effect but more toxicity Side Effects of Therapy-Acute • • • • Nausea/vomiting/mucositis/hair loss Neutropenia/Anemia/Thrombocutopenia Infections/fever Extravsation of vesicants ( Vincristine, Anthracyclines)- Central line • Weight loss/anorexia- Nutritional Support • SIADH- VCR/Cyclophosphamide • Hemorraghic cystistis- Cyclophosphamide; Hydration/MESNA Long term Side effects • Neuro-Cognitive abnormalities: High-dose and intrathechal Methotrexate, Cranial irradiation • Second cancers : Cyclo/Etoposide, radiation • Cardiomyopathy: Anthracyclines ( dose dependent) • Sterility: cyclophosphamise, Stem cell transplantation, Radiation • Endocrine abnormalities: radiation • Employment problems/Insurance • Psycho-social support: parents /siblings • Obesity: ? Females, ? Cranial radiation