Acute myeloid leukemia: morphology and beyond
advertisement

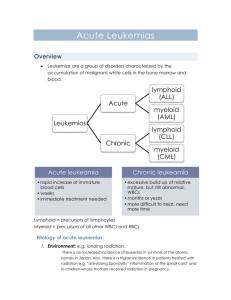
Acute myeloid leukemia: morphology and beyond Nancy Rosenthal, MD Clinical Professor of Pathology Objectives Review clinical, morphologic, immunophenotypic, and cytogenetic abnormalities that allow us to classify AML Introduce new cytogenetic and mutational abnormalities that may be leukemia defining in the future Discuss upcoming updates to the WHO classification that will be utilized starting in 2016 (?) No conflicts to disclose Diagnosing and following adult patients with acute myeloid leukaemia in the genomic age British Journal of Haematology Volume 167, Issue 2, pages 162-176, 7 AUG 2014 DOI: 10.1111/bjh.13048 http://onlinelibrary.wiley.com/doi/10.1111/bjh.13048/full#bjh13048-fig-0001 Diagnosing and following adult patients with acute myeloid leukaemia in the genomic age British Journal of Haematology Volume 167, Issue 2, pages 162-176, 7 AUG 2014 DOI: 10.1111/bjh.13048 http://onlinelibrary.wiley.com/doi/10.1111/bjh.13048/full#bjh13048-fig-0003 Is there still a role for morphology in the diagnosis of AML? May allow establishment of a diagnosis quickly Especially important in the diagnosis of acute promyelocytic leukemia so ATRA can be started Leads to the ability to review all of hematopoiesis Exclude relevant differential diagnoses Do we need to do an aspirate and bone marrow biopsy? Only in the setting of >20% blasts in the peripheral blood Depends on how the patient will be treated Does give information about cellularity, maturation patterns, stromal changes Helpful baseline for comparison purposes during evaluation of treatment efficacy Diagnosis of AML – WHO 2008 Algorithmic approach Previous therapy Therapy related myeloid neoplasm Recurrent cytogenetic abnormalities t(9;22), t(8;21), inv16, etc. AML with myelodysplasia related changes AML Not otherwise specified AML with recurrent genetic abnormalities Clues to the diagnoses can be obtained by evaluating morphology Blasts may be less than 20% Blasts (in all cases) should be counted the old fashion way, not based on flow cytometry Clues from flow cytometry t(8;21) – strong CD34, CD13+, weak CD33, CD19+, PAX5+, cytoplasmic CD79a+, weak TdT t(9;22) – CD34 -, HLADR -, CD117+ Inv16 – myeloid and monocytic markers and CD2+ For a definitive diagnosis - need cytogenetic studies and/or FISH Mutations in AML - 2008 Provisional entities NPM1 CEPBA Prognostic markers FLT3 KIT AML with recurrent cytogenetic abnormalities – new categories New mutation subgroups are being proposed AML with RUNX 1 mutation – older men, poor prognosis AML with NPM1 – good prognosis AML with CEBPADM – only changes prognosis (good) if present as a double mutant Kaplan-Meier curves for overall survival stratified by (A) CEBPA–wild-type (WT) or CEBPAmutant status, (B) CEBPA-WT, CEBPA-single, or CEBPA-double mutant status, (C) CEBPA-WT, single N-terminal (term), single C-term, or double N-term plus C-term mutant sta... Claire L. Green et al. JCO 2010;28:2739-2747 ©2010 by American Society of Clinical Oncology (A) Disease-free survival, (B) overall survival, and (C) event-free survival of patients younger than age 60 years with cytogenetically normal acute myeloid leukemia according to RUNX1 mutation status. Jason H. Mendler et al. JCO 2012;30:3109-3118 ©2012 by American Society of Clinical Oncology AML with myelodysplasia related changes Previous MDS Dyspoiesis – 50% of the cells in 2 cell lines Cytogenetic abnormalities AML with myelodysplasia-related changes Survival data. Olga K. Weinberg et al. Blood 2009;113:1906-1908 ©2009 by American Society of Hematology Characteristics of acute myeloid leukemia with myelodysplasia‐related changes: A retrospective analysis in a cohort of Chinese patients American Journal of Hematology Volume 89, Issue 9, pages 874-881, 19 JUN 2014 DOI: 10.1002/ajh.23772 http://onlinelibrary.wiley.com/doi/10.1002/ajh.23772/full#ajh23772-fig-0002 Revised criteria for AML with MRC Remove de novo cases with no MDS related cytogenetic abnormality if there is an NPM1 or CEBPAdm Revise cytogenetic abnormalities Del9q is an MDS related entity only in the absence of NPM1 mutations NPM1 commonly associated with del9q and is likely not adverse in this setting Case Flow cytometry, cytogenetics and molecular studies 14% myeloid blasts positive for CD117, CD13, CD33, CD34, CD38, HLA-DR and partial expression of CD7. 42~44,XY,add(2)(p11.2), del3, del 5, del(6)(q21),7,add(8)(q24),add(9)(p2,2), add(13)(q22),17,der(19)add(19)(p13)add(19)(q13.1),ad d(22)(p11.2) +mar[cp19]/46,XY[1] FLT3, NPM1 and CEBPA negative Acute erythroid leukemia 2008 2 subtypes recognized Acute erythroid/myeloid leukemia > 50% erythroid precursors >20% of the non-erythroid cells are blasts Acute erythroleukemia First one is controversial as the diagnosis of acute leukemia can be made with a very small number of blasts. Altered erythroid percentages can changed based on therapy, metabolic defects, use of erythropoietin Comparison of 40 patients who had MDS with erythroid hyperplasia (MDS-E), 41 patients who had AML with myelodysplasia-related changes and erythroid hyperplasia (AML-MRC), and 124 patients with acute erythroid leukemia (AEL). Robert P. Hasserjian et al. Blood 2010;115:1985-1992 ©2010 by American Society of Hematology Figure 1. Effects of the presence of erythroid predominance (EP) and diagnostic categories on overall survival. Zuo Z, Medeiros LJ, Chen Z, Liu D, Bueso-Ramos CE, et al. (2012) Acute Myeloid Leukemia (AML) with Erythroid Predominance Exhibits Clinical and Molecular Characteristics that Differ from Other Types of AML. PLoS ONE 7(7): e41485. doi:10.1371/journal.pone.0041485 http://127.0.0.1:8081/plosone/article?id=info:doi/10.1371/journal.pone.0041485 Acute erythroleukemia New update of WHO >50% erythroid precursors and 5-19% blasts would be considered RAEB (actually myelodysplasia with excess blasts) > 50% erythroid and >20% blasts would be acute myeloid leukemia (often AML with myelodysplasia related changes) Pure erythroleukemia will remain in AML Erythroleukemia will become an extremely rare disorder. Case Flow cytometry, cytogenetics and molecular studies 90% monocytic cells which express CD38, CD64, bright CD33, and partial CD36,HLA-DR, CD56, CD13 and CD14 Cytogenetics showed t(11;17) FISH showed an MLL rearrangement but no RARA break-apart probe abnormality NPM1, CEBPA and FLT3 were negative Acute monocytic/monoblastic leukemia Need a careful monocyte, promonocyte, monocyte count to make the diagnosis of AML Presence of NPM1 mutation or 11q23 rearrangement is not leukemia defining May herald rapid progression from CMML to AML is present and these patients should be watched closely Promonocytes Differentiation of types of monocytic cells can be problematic Morphological evaluation of monocytes and their precursors Haematologica 2009;94:994 Authors included Barbara Bain, Richard Brunning, etc. monoblast Round/oval Delicate/lacelike prominent nucleolus Basophilic, rare azurophilic granules Large 20-30 um promonocyte Convoluted indented Delicate/lacelike prominent nucleolus Variably basophilic Variable azurophilic granules Except for nuclear shape similar to monoblast Immature monocyte Convoluted indented More Less condensed basophilic than Rare nucleolus blast but more than monocytes monocyte Lobulated indented Condensed Gray, occ Large 20-25 No nucleolus granules, occ um vacuoles Resemble monocytes but less mature and smaller Monocyte immature monocyte promonocyte monoblast Classification 90 digital images of monocytic cells circulated among 5 experts All experts made the same identification on 25 of the cells, 4/5 made the same identification on 44 cells Percentage of good concordance (4/5 experts) was 76% For 21 cells the concordance rate was 3/5 or 2/5 6 cells had only 2/5 concordance – were sent back for a 2nd reading These cells were confirmed as immature monocytes Highest concordance was for monoblasts and lowest was for immature monocytes Proposed using their classification scheme and correlate with flow cytometric findings Use of flow cytometry to detect abnormal monocytes May lack CD13, CD33, or CD14 Express aberrant antigens such as CD56, CD19, CD7 or CD5 May be difficult to distinguish immature monocytes from promonocytes My conclusion Differentiating these cells is difficult for even those most expert in morphology Making the diagnosis of acute monocytic leukemia based on counting promonocytes is problematic in some cases Summary The diagnosis of AML is ever changing and will continue to evolve based on increased understanding of molecular mechanisms. Targeted therapy may further influence diagnostics in the future. At the moment there is still a role for morphology !!!