Pacemaker/ICD
advertisement
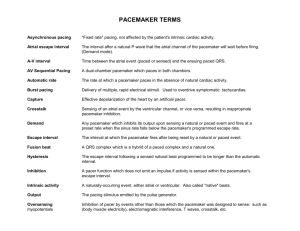
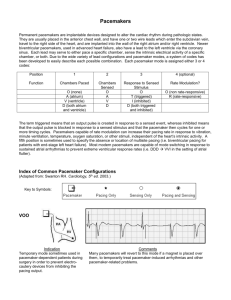
Pacemakers and Implantable Cardioverter Defibrillators Dr. Sivaraman Yegya-Raman Temporary and Permanent Cardiac Pacing • Introduction • Temporary pacing : Indications, Technique • Permanent Pacing : Nomenclature Indications Pacing for Hemodynamic Improvement Pacemaker Implantation, Complications • Implantable Cardioverter Defibrillator Temporary Cardiac Pacing • Transvenous • Transcutaneous • Epicardial • Transesophageal Indications for Temporary Pacing Acute myocardial infarction with: CHB, Mobitz type 2 AV block, medically refractory symptomatic bradycardia, alternating BBB, new bifascicular block, new BBB with anterior MI In absence of acute MI : SSS, CHB, Mobitz type 2 AV block Treatment of tachyarrhythmias : VT Temporary Transvenous Pacing Electrograms Permanent Pacing The Pacemaker System • Patient Lead Pacemaker • Programmer Lead Pacemaker Pacemaker Implantation • Transvenous : • Generator implanted anterior to pectoral muscle • Atrial/Ventricular leads via subclavian or cephalic vein • Sensing and pacing threshold • Chest X-ray for pneumothorax, lead position Castle LW, Cook S: Pacemaker radiography. In Ellenbogen KA, Kay GN, Wilkoff BL [eds]: Clinical Cardiac Pacing. Philadelphia, WB Saunders, 1995, p 538. Acute Complications of Pacemaker Implantation • Venous access Pneumothorax, hemothorax Air embolism Perforation of central vein Inadvertent arterial entry • Lead placement Brady – tachyarrhythmia Perforation of heart, vein Damage to heart valve • Generator Pocket hematoma Improper or inadequate connection of lead Delayed Complications of Pacemaker Therapy • Lead-related Thrombosis/embolization SVC obstruction Lead dislodgement Infection Lead failure Perforation, pericarditis • Generator-related Pain Erosion, infection Migration Damage from radiation, electric shock • Patient-related Twiddler syndrome Codes Describing Pacemaker Modes Position 1 Function Chambers Paced Chambers Sensed Response to Sensing Rate Multisite Modulation pacing Specific Designations O=none A=Atrium V=Ventricle D=DualAtrium and Ventricle O=none A=Atrium V=Ventricle D=DualAtrium and Ventricle O=none T=Triggered I=Inhibited D=DualTriggered and Inhibited O=none R=Rate modulation 2 3 4 5 O=none A=Atrium V=Ventricle D=DualAtrium and Ventricle NASPE/BPEG 2002 DDD Indications for Pacing for AV Block Degree Pacemaker necessary Third Symptomatic congenital complete heart block Aquired symptomatic complete heart block Atrial fibrillation with complete heart block Acquired asymptomatic complete heart block Second Symptomatic type I Symptomatic type II First Pacemaker probably necessary Pacemaker not necessary Asymptomatic Asymptomatic type type II I at supra-His (AV nodal) block Asymptomatic type I at intra-His or infra-His levels Asymptomatic or symptomatic Indications for Pacing for Sinus Node Dysfunction Pacemaker Pacemaker probably necessary Pacemaker not necessary Symptomatic bradycardia Symptomatic patients with sinus node dysfunction with documented rates of <40 bpm without a clear-cut association between significant symptoms and the bradycardia Asymptomatic sinus node dysfunction Symptomatic sinus bradycardia due to longterm drug therapy of a type and dose for which there is no accepted alternative Case #1 72 year old male with chronic atrial fibrillation of greater than 10 years’ duration is admitted following a syncopal episode. A 2D echo shows LVEF 60%. Telemetry reveals atrial fibrillation with slow ventricular response and pauses of 5 to 6 seconds associated with lightheadedness. How would you proceed? Case #1 72 year old male with chronic atrial fibrillation of greater than 10 years’ duration is admitted following a syncopal episode. A 2D echo shows markedly dilated left atrium and LVEF 60%. Telemetry reveals atrial fibrillation with slow ventricular response and pauses of 5 to 6 seconds associated with near syncope. How would you proceed? Answer: Implant a ventricular rate responsive pacemaker Pacemaker Follow-up • GOAL OF FOLLOW-UP – Verify appropriate pacemaker operation – Optimize pacemaker functions – Document findings, changes and final settings in order to provide appropriate patient management “Pacemaker Syndrome” • Fatigue, dizziness, hypotension • Caused by pacing the ventricle asynchronously, resulting in AV dissociation or VA conduction • Mechanism: atrial contraction against a closed AV valve and release of atrial natriuretic peptide • Worsened by increasing the ventricular pacing rate, relieved by lowering the pacing rate or upgrading to dual chamber system • Therapy with fludrocortisone/volume expansion NOT helpful Sources of Electromagnetic Interference • Medical – MRI – Lithotripsy – Electrocautery/cryosurger y – External defibrillators – Therapeutic radiation • Nonmedical – Arc welding equipment – Automobile engines – Radar Transmitters Biventricular Pacing Normal Conduction Is Important Sinus node AV node • Normal conduction allows for prompt and synchronous activation of the atria and ventricles • Results in a brief P wave, PR interval and a narrow QRS Cardiomyopathy, LBBB, Heart Failure Sinus node AV node Conduction block • Delayed lateral wall contraction • Disorganized ventricular contraction • Decreased pumping efficiency Heart Failure Bifocal Ventricular Pacing • Intraventricular Activation • Organized ventricular activation sequence • Coordinated septal and free-wall contraction • Improved pumping efficiency Sinus node AV node Conduction block Stimulation therapy Bi-Ventricular Pacing Right atrial lead Coronary sinus lead Right ventricular lead N Engl J Med 2003 SVC coil RA lead LV lead RV coil RA lead LV lead RV lead Bi-V Pace Implantable Cardioverter Defibrillator (ICD) ICD Implantation • Secondary prevention: Prevention of SCD in patients with prior VF or sustained VT. • Primary prevention: Prevention of SCD in individuals without a h/o VF or sustained VT. Indications For ICD • VF/sustained unstable VT not in the setting of a completely reversible cause. • LVEF ≤ 35%, CHF NYHA class II, III. • Ischemic dilated cardiomyopathy, LVEF ≤ 40%, NSVT and inducible sustained VT. • Syncope, LV dysfunction, inducible sustained VT. • High risk patients with: hypertrophic cardiomyopathy, LQT syndrome, RV dysplasia, Brugada syndrome Ellenbogen K A, 2007 ACC/AHA/HRS 2008 Guidelines: Systolic Heart Failure Cardiac Resynchronization Therapy (CRT) Recommendations • LVEF ≤ 35% • QRS ≥ 120 msec • NYHA functional Class III or ambulatory Class IV • Optimal medical therapy “Typical Case” 58 year old male, CAD, prior MI, EF 28%, CHF, NYHA class II, Medications: Furosemide 40 mg, Enalapril 20 BID, Aldactone 25 qd, Carvedilol 25 BID, no syncope or VT, ECG: Sinus rhythm, old anteroseptal MI, QRS 92 msec Based on available trial data, you would suggest: A. Treating medically without device implantation B. Implanting an ICD C. Implanting an ICD with biventricular pacing capabilities (3 leads) Typical Case Q: 60 year old female presents with a 1 year h/o non ischemic dilated cardiomyopathy, CHF NYHA class III despite maximum medical therapy, LVEF 20% and LBBB with QRS 170 msec. What device is indicated? A: Bi-Ventricular ICD 1° Prevention: Clinical Device Algorithm If Non –Ischemic Dilated Cardiomyopathy: & EF ≤ 35% ACE inhibitors, Beta Blockers ICD If LVEF ≤ 35%, CHF Class III-IV, QRS ≥ 120 ms BiV ICD Magnet Application on Pacemaker/ICD • Pacemaker: – Disables sensing – Changes to VOO or DOO mode – Useful if cautery is being used in PPM dependent pt. • ICD: – Disables Tachycardia sensing – Useful at bedside if pt. has ventricular lead fracture or Afib with rapid ventricular response causing ICD shocks – Prevents ICD shock during cautery application at surgery Future Directions • Leadless pacing • Biological pacemakers • Subcutaneous ICD