3 MB 25th Aug 2014 Pacemaker Presentation
advertisement

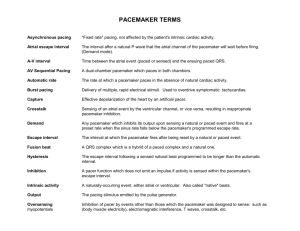
The Electrical Management of Cardiac Rhythm Disorders Bradycardia Device Course Pacemaker Components Leads ● Epicardial ● Endocardial Goals of Cardiac Pacing ● The electrical management of bradyarrhythmias requires ○ Ability to deliver enough energy to consistently depolarize the heart (capture) ○ Ability to correctly sense intrinsic cardiac activity ● These functions are affected by many factors ○ Settings of output parameters (pulse amplitude, pulse width) ○ Sensitivity parameter settings ○ Impedance ○ Electrical concepts Capture ● The capture threshold is defined as the minimum amount of electrical energy required to consistently depolarize the myocardium ● When a pacemaker output causes a depolarization, that is also called “capture” ● The capture threshold is also called the pacing threshold or the stimulation threshold ● The capture threshold is not constant ○ It can change over time (disease, medications, age) ○ It can even change over the course of the day! What Affects the Capture Threshold? • Activity level • Posture • Time of day • Comorbidity • Heart failure • Meals • Drugs • Disease progression Capture Threshold Values Atrial Ventricular Acute Threshold < 1.5 V < 1.0 V Chronic Threshold < 2.5 V < 2.5 V Threshold values at implant should be low; expect chronic thresholds to increase These are suggested values and may not be possible for all patients Sensing ● Sensing refers to how well the pacemaker is able to “listen to” or perceive intrinsic cardiac events ● Important things to consider when talking about sensing ○ Surface ECG ○ Intracardiac electrogram (EGM) ○ Sensing threshold ○ Sense amplifier ○ Sensitivity setting and sensitivity safety margin ○ Unipolar/bipolar configurations ○ Electromagnet interference Surface ECG/Intracardiac EGM ● Surface ECG: graphic depiction of heart’s electrical signals recorded from electrodes on the body’s surface ● Intracardiac EGM: graphic depiction of the heart’s electrical signals recorded by electrodes from inside the heart (pacing lead) Sensitivity Safety Margin ● Sensing thresholds are not constant and vary with many factors ● The sensitivity safety margin allows reliable sensing even with fluctuations in the sensing threshold ● Using this formula, the safety margin should be at least 2 at implant Safety margin = Sensing Threshold Sensitivity Setting Electromagnetic Interference (EMI) ● EMI is defined as electrical signals of nonphysiologic origin ● May interfere with pacemaker (temporarily or permanently) ● Common sources of EMI ○ Cardioversion/defibrillation ○ Electrocautery ○ MRIs ○ Extracorporeal shock wave lithotripsy (ESWL) ○ Therapeutic radiation ○ Radiofrequency ablation What About Cardioversion/Defibrillation? ● May permanently damage the pulse generator ● Can temporarily inhibit or reprogram the pacemaker ○ Backup or noise reversion mode ● Myocardial thermal damage secondary to shock which may result in ventricular fibrillation, myocardial infarction, or both ● Guidelines ○ Evaluate potential device interactions ○ Place paddles 4 to 6 inches away from implanted pacemaker ○ Orient paddles in anterior/posterior position, if possible What About Electrocautery? ● May reprogram or permanently damage the pacemaker ● May inhibit the pacemaker ● May cause the device to go into backup or noise reversion mode ● Myocardial thermal damage secondary to the transmission of the electrical energy may result in VF, MI, or both ● Guidelines ○ Contraindicated What About MRI? ● The magnet in the MRI device can cause asynchronous pacing (pacing without sensing) ● Guidelines ○ Generally contraindicated ● Magna-Safe Study What About Lithotripsy? ● The vibrations in extracorporeal shock wave lithotripsy can damage the pacemaker (especially pacemakers with sensors, i.e. rate-adaptive units) ● Guidelines ○ Program to VVI or VOO mode ○ Keep focal point of lithotripter at least 6 inches away from the implanted pacemaker ○ Monitor the heart throughout the procedure What About Therapeutic Radiation? ● Damage depends on dose ● Damage is cumulative; monitor device throughout course of radiation therapy ● Transistors may fail ● Pacemakers may fail but mode of failure cannot be predicted ● Guidelines ○ Therapeutic ionizing radiation is contraindicated ○ If therapeutic radiation is used, pacemaker should be shielded or moved to a less vulnerable location What About Radiofrequency Ablation? ● RF ablation can temporarily or permanently reprogram the pulse generator ● Guidelines ○ Interrogate the pacemaker following the procedure to verify proper function ○ If necessary, reprogram Myopotentials ● Myopotentials are muscle noises that are sensed by the pacemaker ● Can inhibit pacing ○ The pacemaker senses the myopotential and inhibits the output, thinking the heart has beat on its own! ● Can interfere with sensing ● Can cause inappropriate pacing ○ The pacemaker senses myopotential noise and inappropriately “thinks” it is atrial activity; it then tries to pace the ventricle to keep up or track that atrial activity More EMI Sources ● Arc welding ● Automobile alternators ● Cell phones ○ Phone antenna should not overlap area of implanted pacemaker ○ Talk on other side from implanted device ○ Do not carry an activated cell phone near the implanted pacemaker ○ May cause inappropriate inhibition, asynchronous pacing, backup mode, inappropriate rate adaptation, and mode switching ○ Cellular Tested only from St. Jude Medical EMI in the Medical Environment ● Electrocoagulation from electrocautery ● Defibrillation ● Electroconvulsive therapy ● Diathermy ● MRI ● Stimulators (e.g. transcutaneous nerve) ● Dental equipment ● Diagnostic ultrasound ● Low-frequency acupuncture ● Lithotripsy EMI in the Industrial Environment ● ● ● ● ● ● Arc welding Power lines Transformers Radio and TV transmitters Static charge Large metal frames in magnetic fields ● Induction furnaces and heaters ● Electrical switches EMI in the Public Environment ● CB radio ● Radiofrequency transmissions ● Telecommunications antennas ● Airport metal detectors ● Anti-theft detectors in stores ○ These may not be marked! ● Digital cell phones Effects of EMI ● Pacemaker protection ○ Hardware backup circuits (to protect against loss of memory or software errors) ○ Shields ● Effects ○ EMI inhibition: pulse-to-pulse interval extends to the point that the pacemaker does not pace as often as it should. ○ Noise reversion: change in mode (typically to asynchronous pacing at the programmed rate) which may require reprogramming. ○ EMI tracking: acceleration of pacing as the pacemaker tries to track electromagnetic signals (“thinking” they are atrial signals) Pacemaker Overview NASPE / BPEG (NBG) Pacemaker Code NAPSE/BPEG Generic (NBG) Code Position I II III IV Category Chamber(s) Paced Chamber(s) Sensed Response to Sensing Rate modulation O-None O-None O-None O-None O-None A-Atrium A-Atrium T-Triggered R-Rate modulation A-Atrium V-Ventricle V-Ventricle I-Inhibited V-Ventricle D-Dual (A+V) D-Dual (A+V) D-Dual (T+I) D-Dual (A+V) Letters Used Manufacturer’s Designation Only S- Single (A or V) S- Single (A or V) V Multisite Pacing Magnet Use ● Pacemakers ○ Pace Asynchronously (VOO or DOO) at the given battery rate (Temporarily) ○ Device will revert back to exactly the same parameters it was programmed to once the magnet is removed ● ICD ○ Will disable ICD Shock Therapy (Temporarily) ○ Does not affect pacing ○ Device will revert back to exactly the same parameters it was programmed to once the magnet is removed. ● Magnet must be placed over the device in order for temporary changes to occur. ● ● ● ● ● ● ● ● A Systematic Approach to Diagnosing Rhythm Strips Measure Base Rate Measure AV/PV Interval Verify Atrial capture Verify Atrial sensing Verify Ventricular capture Verify Ventricular sensing Verify Underlying rhythm Document Dual Chamber ECG Analysis What is the Analysis? ECG # 1 Base Rate 60 ppm MTR 120 ppm AVD 200 ms PVARP 250 ms Dual Chamber ECG Analysis Base Rate What is the analysis? ECG # 2 60 ppm MTR 120 ppm AVD 200 ms PVARP 250 ms Dual Chamber ECG Analysis ● What is the analysis Base Rate MTR AV PV PVARP ECG # 3 60 ppm 120 ppm 200 ms 200 ms 250 ms Dual Chamber ECG Analysis ● What is the analysis? Base Rate MTR AV PV PVARP ECG # 4 60 ppm 120 ppm 200 ms 200 ms 250 ms ECG Tracing Results!!! ● #1- Normal ECG –Dual chamber pacing and Atrial pacing w/ Ventricular (intrinsic) sensing. ● #2- Loss of atrial capture. ● #3- Normal ECG ● #4-No ventricular sensing and loss of ventricular capture. ECG #5 Answer ● Slide #5 ○ Normal Sinus Rhythm ○ Can not determine any pacemaker function • Pacers are usually set to pace above 50 or 60 bpm • Single Chamber ICD- Pace above 40bpm ○ Pacemakers only work when? • Native heart rate goes below the base rate • An intrinsic beat does not occur before the set Paced and Sensed AV Delays. • Set at an Asynchronous Mode (VOO or DOO) Thank you for your time!!!