Pacemakers and AICD's
advertisement

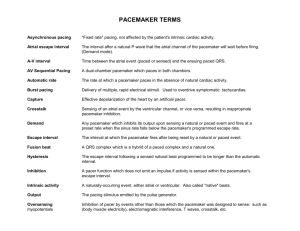
Pacemakers and AICD’s Emergency Medicine Ryan Ngiam Historical Perspective 1905 – Einthoven Published first two human AV block using string galvanometer 1958 – Senning and Elmqvist Asynchronous (VVI) pacemaker implanted by thoracostomy and functioned for 3 hours Arne Larsson First pacemaker patient Used 23 pulse generators and 5 electrode systems Died 2001 at age 86 of cancer Historical Perspective 1960 – First atrial triggered pacemaker 1964 – First on demand pacemaker (DVI) 1977 – First atrial and ventricular demand pacing (DDD) 1980 – Griffin published first successful pacemaker intervention for supraventricular tachycardias Historical Perspective 1981 – Rate responsive pacing by QT interval, respiration, and movement 1994 – Cardiac resynchronization pacing 1998 – Automatic capture detection Now Approximately 3 million with pacemakers Approximately 1 million with ICD device Pacemaker Basics Provides electrical stimuli to cause cardiac contraction when intrinsic cardiac activity is inappropriately slow or absent Sense intrinsic cardiac electric potentials ICD Basics Designed to treat a cardiac tachydysrythmia Performs cardioversion/defibrillation Ventricular rate exceeds programmed cut-off rate ATP (antitachycardia pacing) Overdrive pacing in an attempt to terminate ventricular tachycardias Some have pacemaker function (combo devices) Pacemaker and ICD Basics Pulse Generators Placed subcutaneously or submuscularly Connected to leads Battery Most commonly lithium-iodide type Life span 5 to 8 years Output voltage decreases gradually Makes sudden battery failure unlikely Pacemaker and ICD Basics Asynchronous Fixed rate Impulse produced at a set rate No relation to patients intrinsic cardiac activity Susceptible to Torsades if impulse coincides with t wave Pacemaker and ICD Basics Synchronous Demand mode Sensing circuit searches for intrinsic depolarization potential If absent, a pacing response is generated Can mimic intrinsic electrical activity pattern of the heart Pacemaker Nomenclature I II III IV V Chamber Paced Chamber Sensed Response to Sensing Rate Modulation, Programmability Antitachycardia Features A=Atrium A=Atrium T=Triggered P=Simple P=Pacing V=Ventricle V=Ventricle I=Inhibited M=Multiprogrammable S=Shock D=Dual D=Dual D=Dual R=Rate Adaptive D=Dual O=None O=None O=None C=Communicating O=None Pacemaker Nomenclature 1st letter – chamber paced 2nd letter – chamber sensed 3rd letter – Response to chamber sensed Examples VVI Paces ventricle Senses ventricle Inhibited by a sensed ventricular event Pacing Nomenclature Examples AAT Paces atria Senses atria Triggers generator to fire if atria sensed DDD Paces atria and ventricle Senses atria and ventricle Atrial triggered and ventricular inhibited EKG – 2 spikes DDD Atrial Spike Ventricular Spike Pacemaker Lead System Endocardial leads placed via central access Placed in right ventricle and/or atria Fixed to the endocardium via screws or tines Experimental pacing systems 2 atrial leads (minimize afib) Biventricular pacing Magnet Inhibition Closes an internal reed switch Causes sensing to be inhibited Temporarily turns pacemaker into “asynchronous” mode (set rate) Does NOT turn pacemaker off Rate can confer info regarding battery life Distinct rates for BOL, ERI, EOL Pacemaker Indications Absolute indications Sick sinus syndrome Symptomatic sinus bradycardia Tachy-brady syndrome Afib with slow ventricular response 3rd degree heart block Chronotropic incompetence Inability to increase heart rate to match exercise Prolonged QT syndrome Pacemaker Indications 3rd Degree heart block Pacemaker Indications Relative indications Cardiomyopathy Dilated Hypertrophic Severe refractory neurocardiogenic syncope Paroxysmal atrial fibrillation ICD Indications Generally Used in cases where there was a previous cardiac arrest Or, patients with undetermined origin or continued VT or VF despite medical interventions Pacemaker Complications EKG abnormalities due to Failure to output Failure to capture Sensing abnormalities Operative failures Pacemaker Failure to Output Definition No pacing spike present despite indication to pace Etiology Battery failure, lead fracture, break in lead insulation, oversensing, poor lead connection, “cross-talk” Atrial output is sensed by ventricular lead Pacemaker Failure to Capture Definition Pacing spike is not followed by either an atrial or ventricular complex Etiology Lead fracture or dislodgement, break in lead insulation, elevated pacing threshold, MI at lead tip, drugs, metabolic abnormalities, cardiac perforation, poor lead connection Pacemaker Sensing Abnormalities Oversensing Senses noncardiac electrical activity and is inhibited from correctly pacing Etiology Muscular activity (diaphragm or pecs), EMI, cell phone held within 10cm of pulse generator Undersensing Incorrectly misses intrinsic depolarization and paces Etiology Poor lead positioning, lead dislodgement, magnet application, low battery states, MI Pacemaker Operative Failures Due to pacemaker placement Pneumothorax Pericarditis Perforated atrium or ventricle Dislodgement of leads Infection or erosion of pacemaker pocket Infective endocarditis (rare) Venous thrombosis Pacemaker Complications Pacemaker syndrome Patient feels worse after pacemaker placement Presents with progressive worsening of CHF symptoms Due to loss of atrioventricular synchrony, pathway now reversed and ventricular origin of beat Impact on ALS protocols Not many Can defibrillate Sternal paddles should be placed a safe distance (10 cm) from pulse generator In case of MI May require temporary transcutaneous pacing ICD Complications Similar to pacemaker complications Operative failures Same as pacemakers Sensing and pacing failures Inappropriate cardioversion Ineffective cardioversion/defibrillation Device deactivation ICD Sensing failures Similar to pacmakers Oversensing Undersensing Appropriate failure to treat Programmed cut off at 180 bpm If V Tach occurs at 160 bpms, appropriately fails to cardiovert ICD Inappropriate Cardioversion Most frequent complications Provokes pain and anxiety in pts Consider when Pt is in afib With ventricular response > programmed cut off Received multiple shocks in rapid succession Etiology Afib, T-wave oversensing, lead fracture, insulation breakage, MRI, EMI ICD Inappropriate Cardioversion Treatment Magnet over ICD inhibits further shocks Does NOT inhibit bradycardiac pacing Note Some older devices produce beep with each QRS If left on for >30 seconds, ICD disabled and continous beep To reactivate, lift off magnet and then replace for > 30 seconds, beep will return with each QRS ICD Failure to Deliver Cardioversion Etiology Failure to sense, lead fracture, EMI, inadvertent ICD deactivation Management External defibrillation and cardioversion Do not withhold therapy for fear of damaging ICD If pt’s internal defibrillator activates during chest compressions, you may feel a mild shock (no reports of deaths related to this) Antidysrhymthic medications ICD Ineffective Cardioversion Etiology Inadequate energy output Rise in the defibrillation threshold MI at the lead site Lead fracture Insulation breakage Pre-programmed set of therapies per dysrythmia Manufacturer specific Once number of attempts reached, will not deliver further shocks until new episode is declared Electromagnetic Interference Can interfere with function of pacemaker or ICD Device misinterprets the EMI causing Rate alteration Sensing abnormalities Asynchronous pacing Noise reversion Reprogramming Electromagnetic Interference Examples Metal detectors Cell phones High voltage power lines Some home appliances (microwave) Electromagnetic Interference Intensity of electromagnetic field decreases inversely with the square of the distance from the source Newer pacemakers and ICDs are being built with increased internal shielding Case 1 CC: Chills, rigors HPI: 65 yom c/o fevers, chills, rigors x 1 day. Positive n/v and anorexia. Pt states he had recent pacemaker insertion 4 days ago for an arrhythmia. PMH: HTN Arrythmia Hypercholesterolemia PSHx: As stated above Case 1 Physical exam Temp 101.2, HR 110, BP 90/55 EKG Diagnosis? Case 1 Pocket Infection Pacemaker insertion is a surgical procedure 1% risk for bacteremia 2% risk for pocket infection Usually occurs within 7 days of pacemaker insertion May have tenderness and redness over pacemaker site Case 2 CC: SOB HPI: 65 yom states he had onset of shortness of breath and left sided pleuritic chest pain. Pt states he awoke with pain and difficulty breathing. Had pacemaker placed yesterday. PMHx: HTN, Diabetes, Hypercholesterolemia, Arrythmia, CAD PSHx: Pacemaker, left knee surgery, b/l cataract Case 2 Physical Exam BP 146/85, HR 80s, RR 30s, O2 Sat 88% Lungs Decreased breath sounds on left EKG Diagnosis? Case 2 Pneumothorax Occurs during cannulation of central veins Incidence Cardiologist dependent Treatment Small or asymptomatic – observation Large or symptomatic – Chest tube Case 3 CC: Cardiac arrest HPI: 59 yom found on couch. Wife states they were watching TV when patient let out a moan and then became unconscious. She states, he has a bad heart and had “something” put in a few years ago. PMHx: unknown Meds: bottles in bathroom Case 3 Physical Exam Airway patent, no visible chest rise, no pulses Generally: cool, clammy, diaphoretic EKG: Diagnosis? Case 3 Cardiac Arrest with ICD (V-fib) 2% annual incidence with ICD Etiology ICD delivered predetermined shocks for identified event and patient failed to respond ICD failed to recognize event and failed to shock appropriately Failure to sense, lead fracture, EMI, inadvertent ICD deactivation Case 3 Cardiac Arrest with ICD Treat using ACLS protocols Secure airway CPR Defibrillate/shock as warranted Keep sternal pad 10 cm away from pulse generator Meds Questions References Emedicine http://www.emedicine.com/emerg/topic805.htm Minish, Travis. Pacemaker Emergencies. http://www.cgi.ualberta.ca/emergency/rounds/files/pacers3.ppt The Implantable Pacemaker, a short historical overview. http://igitur-archive.library.uu.nl/dissertations/2006-0426-200006/c1.pdf Healthy Hearts http://www.healthyhearts.com/pacemaker.htm Medtronic http://www.medtronic.com/patients/heart.html Shelton State University http://www.sheltonstate.edu/userfiles/File/faculty/s%20warren/NUR%20202%20E KG%20Dysrrhythmias-Sinus,%20Atrial,%20Junctional,%20Vent%20.pdf Google Images http://images.google.com