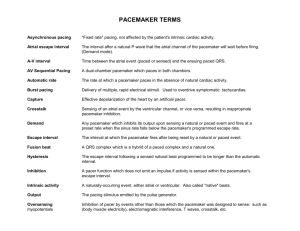
Pacemakers Handout
advertisement

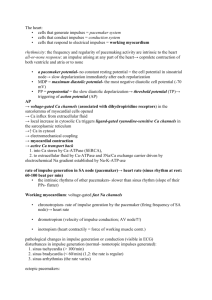
Pacemakers Permanent pacemakers are implantable devices designed to alter the cardiac rhythm during pathologic states. They are usually placed in the anterior chest wall, and have one or two wire leads which enter the subclavian vein, travel to the right side of the heart, and are implanted into the wall of the right atrium and/or right ventricle. Newer biventricular pacemakers, used in advanced heart failure, also have a lead to the left ventricle via the coronary sinus. Each lead may serve to either pace a specific chamber, sense the intrinsic electrical activity of a specific chamber, or both. Due to the wide variety of lead configurations and pacemaker modes, a system of codes has been developed to easily describe each possible combination. Each pacemaker mode is assigned either 3 or 4 codes: Position 1 2 3 4 (optional) Function Chambers Paced Chambers Sensed O A V D Response to Sensed Stimulus O T (triggered) I (inhibited) D (both triggered and inhibited) Rate Modulation? O (none) A (atrium) V (ventricle) D (both atrium and ventricle) O (non rate-responsive) R (rate-responsive) The term triggered means that an output pulse is created in response to a sensed event, whereas inhibited means that the output pulse is blocked in response to a sensed stimulus and that the pacemaker then cycles for one or more timing cycles. Pacemakers capable of rate modulation can increase their pacing rate in response to vibration, minute ventilation, temperature, oxygen saturation, or other stimuli, independent of the heart’s intrinsic activity. A fifth position is sometimes used to specify the absence or location of multisite pacing (i.e. biventricular pacing for patients with end-stage left heart failure). Most modern pacemakers are capable of mode switching in response to sustained atrial arrhythmias to prevent extreme ventricular response rates (i.e. DDD VVI in the setting of atrial flutter). Index of Common Pacemaker Configurations (Adapted from: Swanton RH. Cardiology, 5th ed. 2003.) Key to Symbols: VOO Indication Temporary mode sometimes used in pacemaker-dependent patients during surgery in order to prevent electrocautery devices from inhibiting the pacing output. Comments Many pacemakers will revert to this mode if a magnet is placed over them, to temporarily treat pacemaker-induced arrhythmias and other pacemaker-related problems. VVI Indication The combination of AV block and chronic atrial arrhythmias (particularly atrial fibrillation). Comments VVIR should be used in patients who exhibit chronotropic incompetence. AAI Indication Sick sinus syndrome in the absence of AV node disease or atrial fibrillation. Comments All patients needing AAI mode should be given rate-responsive pacemakers (AAIR), even those with chronotropic competence, due to the high likelihood that chronotropic incompetence will subsequently develop. VDD Indication AV block with intact sinus node function (particularly useful in congenital AV block). Comments This mode, most commonly engineered with a single-lead system, is also known as atrially sensed ventricular inhibited pacing (ASVIP). If atrial fibrillation occurs or excessive supraventricular bradycardia occurs, the pacemaker usually will switch to VVI mode. DDD Indications 1. The combination of AV block and SSS. 2. Patients with LV dysfunction and LV hypertrophy who need coordination of atrial and ventricular contractions to maintain adequate CO. Comments If atrial fibrillation occurs, the pacemaker usually will switch to VVI mode. Ideally, all pacemakers in DDD mode should be rateresponsive (DDDR). 2 Timing Cycles A thorough understanding of pacemaker modes requires some discussion of the timed intervals which a pacemaker senses, and which dictates its activity. Timing Cycles Definitions LR (Lower rate limit) – The longest period that a pacemaker will tolerate the absence of a QRS complex. UR (Upper rate limit) – The shortest period between a QRS complex and a subsequent P wave, for which the pacemaker’s ventricular lead will fire in response to the sensed P wave. VRP (Ventricular refractory period) – The period of time after a sensed or paced QRS complex, during which subsequent QRS complexes do not reset the timing cycle. This value is set by the pacemaker’s programmer. ARP (Atrial refractory period) – The period of time after a sensed of paced P wave, during which subsequent P waves do not reset the timing cycle. This value is also set by the programmer. AVI (Atrioventricular interval) – The period of time between the onset of a P wave and the onset of a subsequent QRS complex (either paced or intrinsically conducted) PV (P wave – ventricular interval) – The period of time between the onset of an intrinsic P wave and a subsequent ventrticular pacing impulse. VA (Ventriculoatrial interval) – Equals to the LR – AVI. PVARP (Post-ventricular atrial refractory period) – The period after the onset of a QRS complex (either sensed or paced) during which a sensed atrial impulse does not reset the timing cycle. The PVARP is a significant factor in determining the upper rate limit, thus preventing pacemaker-induced tachycardia. TARP (Total atrial refractory period) – Equal to the AVI + PVARP. VAI (Ventriculoatrial interval) – The period of time between the onset of a QRS (either paced or sensed) and the onset of a subsequent P wave. VVI If the LR time expires without sensing a ventricular impulse, the single ventricular lead fires. The LR time is reset with each QRS complex that is either sensed or paced, and which does not occur during the VRP. AAI If the LR time expires without sensing an atrial impulse, the single atrial fires. The LR time is reset with each P wave that is sensed or paced, and which does not occur during the ARP. 3 VDD A sensed P wave initiates the AV interval. If the AVI expires without a sensed QRS complex, a ventricular pacing impulse is delivered. If the LR time expires without sensing a ventricular impulse, a ventricular pacing impulse is also delivered. DDD A sensed or paced P wave initiates the AV interval. If the AVI expires without a sensed QRS complex, a ventricular pacing impulse is delivered. If the LR time expires without sensing a ventricular impulse, a ventricular pacing impulse is also delivered. If the VA interval expires, an atrial pacing impulse is delivered. Above diagrams taken from: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 7th ed., 2005. Summary of Arrhythmia-Related Indications for Pacemaker Placement Class I 1. Sinus node dysfunction with documented symptomatic bradycardia 2. Symptomatic chronotropic incompetence (failure to increase HR with exercise or increased metabolic demand) 3. 3° and advanced 2° AV block at any anatomic level, associated with any of the following: Symptomatic bradycardia Arrhythmias that require drugs resulting in symptomatic bradycardia Sinus pauses > 3 seconds Asymptomatic escape rate < 40bpm while awake Post-op AV block, not expected to resolve after surgery Neuromuscular disease with AV block, regardless of presence or absence of symptoms (there may be an unpredictable progression of AV conduction disease) 4. 2° AV block, regardless of type or site of block, with associated symptomatic bradycardia 5. Type II 2° AV block with wide QRS, regardless of symptoms or escape rate Class IIa 1. Syncope of unexplained origin when major abnormalities of sinus node function are discovered or provoked during EP studies. 2. Asymptomatic 3° AV block with an awake ventricular rate > 40bpm 3. Asymptomatic type II 2° AV block 4. Asymptomatic type I 2° AV block at intra or infra-His levels 5. 1° or 2° AV block with symptoms suggestive of pacemaker syndrome 4 Problems with Pacemakers (Rhythm strips from: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 7th ed., 2005 Failure to Capture Causes: Threshold rise (electrolytes, drugs) Lead dislodgement Lead fracture RV infarct In the above rhythm strip, the second pacing impulse fails to lead to ventricular activity for unclear reasons, and is subsequently followed by a failure to pace. Failure to Pace Causes: Oversensing Battery failure Crosstalk Internal insulation failure Conductor coil fracture In the second beat, the atrial pacing impulse is not followed by a ventricular impulse, likely due to crosstalk, in which the ventricular lead senses the atrial spike and interrupts it as intrinsic ventricular activity. Failure to pace due to oversensing of myopotentials leading to a pause in cardiac rhythm. Failure to Sense Causes: Undersensing (False Inhibition) Lead Fracture PVC Despite intrinsic ventricular activity, the pacemaker continues ventricular pacing uninterrupted, likely as a result of undersensing. 5 Lead-related complications can be distinguished intraoperatively based upon the following: Wire fracture Insulation break Lead dislodgement Lead exit block Voltage Threshold High Low High High Current Threshold Variable High High High Lead Impedence High Low Normal Normal Pacemaker-Mediated Tachycardia (also known as pacemaker-reentry tachycardia or endless-loop tachycardia) Frequently, during normal AV synchronous pacing a PVC can occur that results in retrograde ventriculoatrial conduction and a retrograde P wave. If this retrograde conduction is sensed by the atrial lead, the AVI can be initiated, leading to a paced ventricular complex, which can again result in a retrograde P wave, forming a type of reentrant circuit and a tachyarrhythmia. This potential arrhythmia is best prevented by choosing a PVARP long enough to prevent the sensing of retrograde P waves. Transvenous Pacemakers Transvenous pacemakers are only one form of temporary cardiac pacing, but are the form most likely to be encountered outside the cardiac surgery setting. (Other forms include epicardial, transesophageal, and transcutaneous pacing.) Transvenous pacers are typically placed under fluoroscopic guidance, but can be also placed via a balloon-tipped catheter via the right internal jugular or left subclavian veins. Although some SwanGanz catheters are equipped with pacing ability, they are less stable than other endocardial leads, and should be avoided in patients who are pacemaker dependent. Situations in which a temporary pacemaker (transvenous or epicardial) may be preferred over a permanent implantable pacemaker: ▪ Injury to the conduction system during CABG (frequently improves over time) ▪ Lyme disease ▪ Temporary SA node injury following heart transplantation ▪ Cardiac trauma ▪ Reverisble toxic/metabolic conditions (hyperkalemia, digoxin toxicity, beta blocker overdose) ▪ To establish the possible benefit from a permanent pacemaker in a patient with sinus bradycardia or AV block when the cause of symptoms is unclear ▪ Symptomatic bradycardia or new bifascicular block during an acute MI ▪ Patient with an indication for a permanent pacemaker, but also with an active systemic infection Transvenous pacemakers typically consist of a single ventricular lead, which both senses and paces, however temporary dual chamber AV sequential pacing all exists. Serious complication from transvenous pacemakers are generally rare, but include: Local bleeding Pneumothorax Thrombophlebitis Air embolism Infection Cardiac perforation and subsequent tamponade Induction of ventricular arrhythmias Catheter knotting Subdiaphragmatic stimulation 6 Procedures for basic single chamber pacing: 1. Determine the Pacing Mode This is determined by the position of the single lead (atrial vs. ventricular). The pacemaker can also be placed into demand (synchronous) mode or asynchronous mode, which can usually be done by adjusting the sensitivity dial. In demand mode, the pacing output is inhibited by sensed intrinsic electrical activity, whereas in asynchronous mode, the pacing output is constant regardless of intrinsic activity. (Asynchronous mode is best suited for patients whose intrinsic HR is constantly below the paced rate.) 2. Determine the Sensing Potential Turn the rate dial to at least 10bpm below the patient’s intrinsic HR. Then set the output to the minimal setting (to prevent competitive pacing). Next, turn the sensitivity dial to the most sensitive setting. Slowly decrease the sensitivity until the pace indicator begins to flash. (At minimum output, there should be no actual pacing of the cardiac rhythm.) Increase the sensitivity until the sense indicator begins to flash again. The millivolt value at which this occurs is the sensing threshold. The sensitivity dial should then be set at twice this sensitivity (to ensure a margin of safety). For example, if the threshold is 6mV, the sensitivity dial should be set at 3mV. Lastly, reset the rate and output dials to their original values. 3. Determine the Stimulation Threshold Turn the rate dial to 10bpm above the patient’s intrinsic HR. Verify 1:1 capture on the ECG. Gradually decrease the pacing output until 1:1 capture is lost. Then slowly increase the output until 1:1 capture is regained. This value is the stimulation threshold. The output dial should then be set at twice the threshold value. 4. Select the Appropriate Pacing Rate This value will depend upon the specific clinical situation. A typical transvenous pacemaker (Medtronic 5348 pictured) Some transcutaneous pacemakers are equipped with the ability to deliver rapid atrial pacing for termination of some atrial arrhythmias, however, this should be done under the supervision of an experienced cardiologist only. 7