Objectives
advertisement

I have nothing to disclose
&
No conflicts of Interest
What Do I Do With
That Pacemaker Spike
Michelle M. Loomis, APRN-BC
Objectives
• Review indications for pacemaker placement
• Understand 2 primary functions of a
pacemaker
• Review the NBG code for pacemaker mode
• Identify normal parameters of pacemaker
function
• Recognize normal function vs abnormal
• Trouble shoot when pacemaker spike does not
seem normal
INDICATIONS FOR
PERMANENT PACEMAKER
1
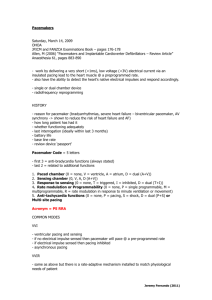
Indications for Pacemaker
•
•
•
•
•
•
•
•
•
•
•
SA/AV block
Symptomatic bradycardia
Need for medications that may cause bradycardia
Chronic Bi-fasicular and Tri-fasicular block
Post MI
Sinus Node Dysfunction (SND)
Certain arrhythmias
Atrial fib with RVR
Carotid Hypersensitivity (CSH)
Neurocardiogenic/Vagal Syncope
Valve surgery
Undersensing (overpacing):
Failure to sense
-Pacer lead fails to detect an intrinsic rhythm
-Paces unnecessarily
-Patient may feel “extra beats”
-If an unneeded pacer spike falls in the latter
portion of T wave, dangerous
tachyarrhythmias or V fib may occur
(R on T)
*****TX: Increase sensitivity of pacer
6
Pacing and Sensing
• Pacing-pacemaker lead does not see intrinsic
electrical signal within a certain time interval
– Dual chamber (AV delay)
– Single chamber (lower rate)
– Depolarization of atria and/or ventricles in response to
a pacing stimulus
• Sensing-pacemaker lead sees intrinsic rhythm and
therefore does not pace
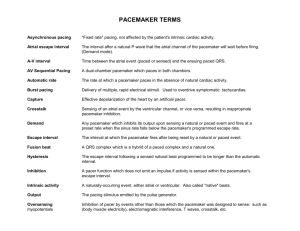
NBG Code
I
Chamber
Paced
II
Chamber
Sensed
III
Response
to Sensing
IV
Programmable
Functions/Rate
Modulation
V: Ventricle
V: Ventricle
T: Triggered P: Simple
programmable
A: Atrium
A: Atrium
I: Inhibited
M: Multiprogrammable
D: Dual (A+V) D: Dual (A+V) D: Dual (T+I) C: Communicating
O: None
O: None
S: Single
S: Single
(A or V)
O: None
V
Antitachy
Function(s)
P: Pace
S: Shock
D: Dual (P+S)
R: Rate modulating O: None
O: None
(A or V)
2
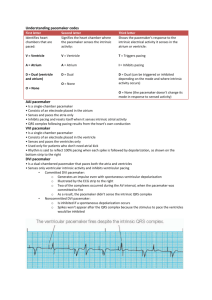
Standard Pacemaker Features
• Lower rate
• Upper rate
• Synchronous
– contains 2 circuits, one forms an impulse and one acts as a sensor
• Asynchronous
– Just paces at one rate--FIXED RATE—
– Independent of intrinsic cardiac activity
Standard Features (cont..)
• AV interval (AV delay)
– Dual chamber
– RV vs LV pacing
– PR interval
• R wave sensitivity
• Rate Response
When activated by an R wave, sensing circuit either triggers or
inhibits the pacing circuit
Called “Triggered” or “Inhibited” pacing
• Mode Switch
– Sensors (activity and breathing)
– Atrial arrhythmias
Upper Activity (Sensor) Rate
• In rate responsive modes, the Upper Activity Rate
provides the limit for sensorsensor-indicated pacing
Lower Rate Limit
Upper Activity Rate Limit
PAV
DDDR 60 / 120
A-A = 500 ms
AP
VP
V-A
PAV
AP
V-A
VP
3
Upper Tracking Rate
• The maximum rate the ventricle can be paced in
response to sensed atrial events
Lower Rate Interval
{
Upper Tracking Rate Limit
SAV
AS
VA
VP
SAV
AS
VA
VP
DDDR 60 / 100 (upper tracking rate)
Sinus rate: 100 bpm
Normal vs Abnormal Function
• Mode of the Pacemaker
• Features of the device
• Is there capture in the chambers that are affected?
• IT IS NOT THE PACEMAKER
SPIKE BUT WHAT IT MEANS
• Abnormal Function
– Sensing problems
• Artifact
– Look in 2 leads
– Interference from something
4
Reasons for No
Pacemaker Spikes
• Dead Battery
– Will see patient’s intrinsic rhythm
• Failure to pace
• Failure to capture
• Over sensing
5
Sensing
• The ability of the pacemaker to see intrinsic
rhythm and if not appropriately respond by
pacing
• Undersensing
• Oversensing
Undersensing
• Pacemaker does not “see” the intrinsic beat, and
therefore does not respond appropriately.
Scheduled pace delivered
Intrinsic beat
not sensed
6
Oversensing
Pacemaker
working
Pacemaker
senses T wave
as QRS and
doesn’t fire
VVI / 60
properly
7
Fusion Beats
• The combination of an intrinsic beat and a
paced beat
• The morphology varies, a fusion beat does
not really look like a paced beat or a
intrinsic beat
• Fusion beats contribute to the conduction of
the chambers being paced.
Fusion Beats
• The combination of an intrinsic beat and a
paced beat
• The morphology varies
• The fusion beat doesn’t really look like a
paced beat or an intrinsic beat
• Spike in QRS or near T-wave but not at end
of T-wave
Managed Ventricular Pacing
(MVP)
• Atrial-based pacing mode that significantly
reduces unnecessary right ventricular pacing by
primarily operating in an AAI(R) pacing mode
while providing the safety of a dual chamber
backup mode if necessary.
• Promotes Intrinsic Conduction Without
Compromising Safety
8
MVP® Basic Operation
Ventricular Back-Up
Ventricular pacing only as needed in the presence of transient loss of conduction.
Loss of
conduction
Back-up
V-pace
Pacemaker Mediated Tachycardia:
• Retrograde conduction of impulses from the
ventricle is sensed by the pacer as atrial
tachycardia and a continuous circuit is formed.
MVP® Basic Operation
AAI(R) to DDD(R) Switch
Ventricular support if loss of A-V conduction is persistent.
Switch to DDD(R) occurs after
back-up VP; programmed PAV/SAV are used
during this mode of operation
Pacemaker-Mediated Tachycardia
(PMT)
• A rapid paced rhythm that can occur with
atrial tracking pacemakers
• Occur in patients with dual chamber pacemakers.
• Initiated by a PVC with retrograde that tracks fast
atrial rates
9
ANTI-TACHYCARDIAC PACING
• PRACTICE TIME
10
How To Look at
Pacemaker Spikes
Strip #1
DDD 60/150 AV=200ms PVARP=225ms
• Mode of PPM
• Is there capture after each spike
• Are there spikes anywhere in the p-wave,
QRS or T-wave
• Are the pacemaker spikes really close
together
Loss of ventricular
capture.
Patient’s intrinsic QRS finally
comes through on its own.
Strip #3
Strip #2
•DDD 60/130 AV=120ms PVARP=320ms
Why isn’t there a ventricular pace shortly after these
P waves? Atrial undersensing?
Ventricle did not pace. How come?
Mode is DDIR
We don’t track P waves in DDIR mode. This is normal function.
Must have seen something that wasn’t
actually there…..”Ventricular Oversensing”
11
12
13
14
When to Call
•
•
•
•
Loss of capture
Patient unstable
Pacemaker spike in the middle of the t-wave
PMT
• Patient’s admitted who have a pacemaker
do not need to have a standard pacemaker
check
Summary
• Pacemaker spikes can be normal and abnormal
• This can be very tricky to figure out sometimes
• Know how device is programmed
– Sign over patient’s bed
– Let CMT know
• Know capture of each chamber being paced
• Always look in 2 leads
• When posting strips, mark the lead
15