Determining BRAIN DEATH in Adult
advertisement

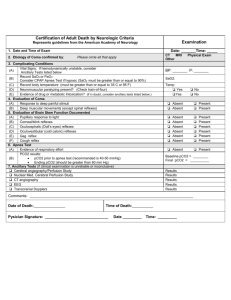
DEPARTMENT OF NEUROLOGY OSMANIA MEDICAL COLLEGE American Academy of Neurology Guideline Update 2010 Coma, from the Greek ‘‘deep sleep or trance,’’ is a state of unresponsiveness in which the patient lies with eyes closed and cannot be aroused to respond appropriately to stimuli even with vigorous stimulation. • Three medical considerations emphasize the importance of the concept of brain death: (1) Transplant programs require the donation of healthy peripheral organs for success. The early diagnosis of brain death before the systemic circulation fails allows the salvage of such organs. However, ethical and legal considerations demand that if one is to declare the brain dead, the criteria must be clear and unassailable (2) Even if there were no transplant programs, the ability of modern medicine to keep a body functioning for extended periods often leads to prolonged, expensive, and futile procedures accompanied by great emotional strain on family and medical staff. (3) Critical care facilities; are limited and expensive and inevitably place a drain on other medical resources. Their best use demands that one identify and select patients who are most likely to benefit from intensive techniques, so that these units are not overloaded with individuals who can never recover cerebral function. The THREE clinical findings necessary to confirm irreversible cessation of all functions of the entire brain, including the brain stem: 1. coma (with a known cause) 2. absence of brainstem reflexes, and 3. apnea. The Clinical Evaluation The Neurologic Assessment Ancillary Test Documentation A. Establish irreversible and proximate cause of coma. Exclude the presence of a CNS-depressant drug effect There should be no recent administration or continued presence of neuromuscular blocking agents There should be no severe electrolyte, acid-base, or endocrine disturbance B. Achieve normal core temperature. Raise the body temperature and maintain a normal or nearnormal temperature-36°C C. Achieve normal systolic blood pressure. Neurologic examination is usually reliable with a systolic blood pressure 100 mm Hg. D. Perform 1 neurologic examination If a certain period of time has passed since the onset of the brain insult to exclude the possibility of recovery, 1 neurologic examination should be sufficient to pronounce brain death. The Clinical Evaluation The Neurologic Assessment A. Coma Patients must lack all evidence of responsiveness. Eye opening or eye movement to noxious stimuli is absent. Noxious stimuli should not produce a motor response other than spinally mediated reflexes. B. Absence of Brain Stem Reflex Absence of pupillary response to a bright light is documented in both eyes. Absence of ocular movements using oculocephalic testing and oculovestibular reflex testing. Absence of corneal reflex. Absence of facial muscle movement to a noxious stimulus. Absence of the pharyngeal and tracheal reflexes. C. Apnea Absence of a breathing drive. Breathing drive is tested with CO2 Challenge. Prerequisites: 1) normotension 2) normothermia, 3) euvolemia 4) eucapnia (PaCO2 35–45 mm Hg) 5) absence of hypoxia 6) no prior evidence of CO2 retention Adjust vasopressors to a systolic blood pressure 100 mm Hg. Preoxygenate for at least 10 minutes with 100% oxygen to a PaO2 200 mm Hg. Reduce ventilation frequency to 10 breaths per minute to eucapnia. Reduce positive end-expiratory pressure (PEEP) to 5 cm H2O If pulse oximetry oxygen saturation remains 95%, obtain a baseline blood gas Disconnect the patient from the ventilator. Preserve oxygenation(e.g., place an insufflation catheter through the endotracheal tube and close to the level of the carina and deliver 100% O2 at 6L/min). Look closely for respiratory movements for 8–10 minutes. Abort if systolic blood pressure decreases to 90 mm Hg. Abort if oxygen saturation measured by pulse oximetry is 85% for 30 seconds. If no respiratory drive is observed, repeat blood gas after 8 minutes. If respiratory movements are absent and arterial PCO2 is 60 mm Hg (or 20 mm Hg increase in arterial PCO2 over a baseline normal arterial PCO2), the apnea test result is POSITIVE. If the test is inconclusive but the patient is hemodynamically stable during the procedure, it may be repeated for a longer period of time (10–15 minutes) after the patient is again adequately preoxygenated. The Clinical Evaluation The Neurologic Assessment Ancillary Test In clinical practice, EEG, cerebral angiography, nuclear scan, TCD, CTA, and MRI/MRA are currently used ancillary tests in adults. Ancillary tests can be used when uncertainty exists about the reliability of parts of the neurologic examination or when the apnea test cannot be performed. “In adults, ancillary tests are not needed for the clinical diagnosis of brain death and cannot replace a neurologic examination.” The Clinical Evaluation The Neurologic Assessment Ancillary Test Documentation Time of death is the time the arterial PCO2 reached the target value (60). In patients with an aborted apnea test, the time of death is when the ancillary test has been officially interpreted. Neuronal Swelling Neuronal Injury ICP>MAP is incompatible with life Decreased Intracranial Blood Flow Increased Intracranial Pressure Persistent Vegetative State Locked-in Syndrome Minimally Responsive State Normal Sleep-Wake Cycles No Response to Environmental Stimuli Diffuse Brain Injury with Preservation of Brain Stem Function Static Encephalopathy Diffuse or Multi-Focal Brain Injury Preserved Brain Stem Function Variable Interaction with Environmental Stimuli Ventral Pontine Infarct Complete Paralysis Preserved Consciousness Preserved Eye Movement Clinical Prerequisites: Known Irreversible Cause Exclusion of Potentially Reversible Conditions ▪ Drug Intoxication or Poisoning ▪ Electrolyte or Acid-Base Imbalance ▪ Endocrine Disturbances Core Body temperature > 32° C Coma Absent Brain Stem Reflexes Apnea No Response to Noxious Stimuli ▪ Nail Bed Pressure ▪ Sternal Rub ▪ Supra-Orbital Ridge Pressure Pupillary Reflex Eye Movements Facial Sensation and Motor Response Pharyngeal (Gag) Reflex Tracheal (Cough) Reflex Pupils dilated with no constriction to bright light Occulo-Cephalic Response “Doll’s Eyes Maneuver” Oculo-Vestibular Response “Cold Caloric Testing” Corneal Reflex Jaw Reflex Grimace to Supraorbital or Temporo-Mandibular Pressure Prerequisites ▪ Core Body Temperature > 32° C ▪ Systolic Blood Pressure ≥ 100 mm Hg ▪ Normal Electrolytes ▪ Normal PCO2 1. Pre-Oxygenation ▪ 100% Oxygen via Tracheal Cannula ▪ PO2 = 200 mm Hg 2. Monitor PCO2 and PO2 with pulse oximetry 3. Disconnect Ventilator 4. Observe for Respiratory Movement until PCO2 = 60 mm Hg 5. Discontinue Testing if BP < 90, PO2 saturation decreases, or cardiac dysrhythmia observed Facial Trauma Pupillary Abnormalities CNS Sedatives or Neuromuscular Blockers Hepatic Failure Pulmonary Disease Sweating, Blushing Deep Tendon Reflexes Spontaneous Spinal Reflexes- Triple Flexion Babinski Sign Recommended when the proximate cause of coma is not known or when confounding clinical conditions limit the clinical examination EE G Normal Electrocerebral Silence Cerebral Angiography Normal No Intracranial Flow Technetium-99 Isotope Brain Scan MR- Angiography Transcranial Ultrasonography Somatosensory Evoked Potentials Somatosensory-evoked potentials. Bilateral absence of N20-P22 response with median nerve stimulation. THANK YOU Are there patients who fulfil the clinical criteria of brain death who recover brain function? There is insufficient evidence to determine the minimally acceptable observation period to ensure that neurologic functions have ceased irreversibly. What is an adequate observation period to ensure that cessation of neurologic function is permanent? There is insufficient evidence to determine the minimally acceptable observation period to ensure that neurologic functions have ceased irreversibly. Are complex motor movements that falsely suggest retained brain function sometimes observed in brain death? For some patients diagnosed as brain dead, complex, non– brain-mediated spontaneous movements can falsely suggest retained brain function. Additionally, ventilator autocycling may falsely suggest patient-initiated breathing. What is the comparative safety of techniques for determining apnea? Apneic oxygenation diffusion to determine apnea is safe, but there is insufficient evidence to determine the comparative safety of techniques used for apnea testing. Are there new ancillary tests that accurately identify patients with brain death? Because of a high risk of bias and inadequate statistical precision, there is insufficient evidence to determine if any new ancillary tests accurately identify brain death. This update sought to use evidence-based methods to answer 5 QUESTIONS historically related to variations in brain death determination4 to PROMOTE UNIFORMITY IN DIAGNOSIS. 1959 Coma de’passe’ Mollaret and Goulon 1968 Irreversible Coma/Brain Death Harvard Medical School Ad Hoc Committee 1981 Uniform Determination of Death Act - President’s Commission for the Study of Ethical Problems in Medicine 1995 American Academy of Neurology Guidelines for the determination of Brain Death 2005 NYS Guidelines for Determining Brain Death “An individual who has sustained either irreversible cessation of circulatory and respiratory functions, or irreversible cessation of all functions of the entire brain, including the brainstem. “ Uniform Determination of Death Act (UDDA) A determination of death must be made with accepted medical standards The American Academy of Neurology (AAN) published a 1995 practice parameter to delineate the medical standards for the determination of brain death.