2011 CNS Bacterial Infection - Emory University Department of
advertisement
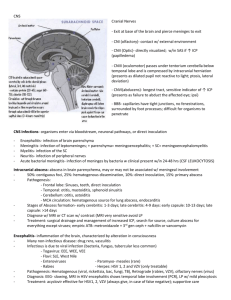
CNS Bacterial Infections Pediatric Critical Care Medicine Emory University Children’s Healthcare of Atlanta Introduction • Infections of the CNS are among the most devastating infectious diseases – Cause death and disability worldwide • Often present as medical emergencies – Early, appropriate care is critical to reducing morbidity and mortality CNS Development CNS Development • 2 wks: Neural plate forms from ectoderm – Neural tube completed by day 26-28 • 3-4 wks: Hemispheres form – Pons/medulla develop at 3-7.5 wks • 8-18 wks: Neuronal proliferation – Up to 200,000 new neurons per minute • > 25 wks: Arborization, synaptogenesis, apoptosis, neural connectivity • 30 wks - adolescence: Continuing myelination CNS Development • The mature human brain will have 10 billion neurons – Most are formed during the period of rapid proliferation (8-18 wks) – Very little neurogenesis after birth • 70% of developing neurons will die by apoptosis during development – Bcl-2, Apaf1, cystein-protease caspase • Pathways are upregulated during development – Newborn brain more prone to injury-related PCD Blood-Brain Barrier Blood-Brain Barrier • There is debate over whether the infant BBB is ‘leaky’ – Tight junctions in mature BBB form a true zona occludens – Agree that permeability of macromolecules in the same as in adults • BBB has both ‘static and dynamic’ properties – Astrocyte feet have lots of control • Impermeable to ions, proteins, osmolar agents – Osmotic (not oncotic) gradients are critical to water movement through aquaporin channels Pathogenesis • Pathogens must first gain access to CNS to cause disease – Subarachnoid space (meningitis) – CNS parenchyma (encephalitis, myelitis, abscess) • Most are spread through the bloodstream • May also occur through direct spread » Adjacent structures (otitis, sinusitis, dental abscess) » Shunt infections » Skull fractures Clinical Syndromes Syndrome Signs and Symptoms Pathogen Acute Meningitis Acute onset of fever, HA, vomiting, meningismus, AMS Progression over hours to days Bacteria, viruses Subacute or Chronic Meningitis Gradual onset, lower fever, progression over weeks Tuberculous, fungal Acute Encephalitis Diffuse: AMS and seizures Focal: tropism of virus for specific CNS location (HSV) Viruses Encephalopathy w/ Systemic Infection Symptoms vary, often AMS. Chorea? Shigella, typhoid, malaria, Rickettsia, endocarditis Postinfectious Various, depending on lesion ADEM, transverse myelitis, optic neuritis, MS Viruses, vaccines Diagnosis Thorough history and physical exam are very important! Note chronicity of symptoms, comorbid conditions, preceding illnesses, VP shunt Travel, surgery, trauma, sick contacts, insect bites, animal contact, sexual activity Lab evaluation: CBC, CMP, CPR, UA, blood culture CSF: opening pressure, cultures, cytology Fungal, AFB, mycobacterial cx if appropriate CSF gram stain, PCR, antigen testing, serology Other studies: Imaging, EEG, biopsy, I&D CSF Findings Characteristics Viral Bacterial Tubercular WBC/mm3 Normal (<5) or raised (10-100) Raised 100 – >1000 Raised 100 – 1000 Cell type Lymphocytes Neutrophils Lymphocytes Glucose (CSF: serum) Normal (<0.6) or Decreased <0.4 decreased (<0.4) (or much lower) Decreased <0.4 Protein Normal (<50) or up to 100 Raised 100-500 Raised 100 – >500 General Management • Neurologic evaluation – – – – Meningeal signs Severity of coma Neuro exam (focal deficits, cranial nerves, bulbar tone) Increased ICP • Other sites of infection or injury – Otitis, sinusitis, PNA – Rashes or skin lesions – Trauma General Management • Consider intubation if GCS <8 or bulbar hypotonia – Take care to minimize ICP spikes – Consider thiopental, propofol, ketamine (becoming more accepted for high ICP), lidocaine – Modified RSI, avoid overventilation • Get antibiotics going early and at high doses! • Cardiovascular support as needed General Management • Consider ICP monitoring for moderate to severe ICP elevation – Level of consciousness correlates well with decreased cerebral perfusion – M&M are inversely related to CPP • Control seizures with benzodiazepenes – About 50% of patients with seizures progress to status – Status is hard to treat and has poor outcome General Management • Electrolyte and fluid derangements are common – At risk for diabetes insipidus – Do not fluid restrict empirically – Prospective RCT by Singhi et al found no outcome improvement with fluid restriction vs. maintenance • Correct hyponatremia slowly over 36-48 hrs – 3% if necessary for seizures • Also at risk for hypokalemia – GI losses, hemodilution, osmotherapy, diuretics, sepsis BACTERIAL MENINGITIS Etiology, Pathophysiology, Diagnosis, Treatment, Outcome Bacterial Meningitis: Etiology *There are 3 main bacterial meningeal pathogens: 1. Haemophilus influenzae 2. Neisseria meningitidis 3. Streptococcus pneumoniae *Incidence varies by region and age. Haemophilus influenzae • Small GN, pleomorphic, coccobacilli • H. flu type B causes almost ALL invasive disease • Nontypeable Hib can rarely cause meningitis. • Incidence of Hib decreased by 97% after vaccine Neisseria meningitidis - GN diplococci - Serotypes A,B,C,Y, and W135 cause most invasive disease. - Virulence depends on: 1. Capsular polysaccharide 2. LPS(endotoxin) 3. Pili 4. IgA protease 5. ompS gene Streptococcus pneumoniae * Small, non-motile GPC in pairs or chains. * 8 serotypes cause 90% of invasive disease. 1, 4, 6, 9, 14, 18, 19 & 23 * Virulence depends on capsular polysaccharides * Associated with CSF leak (skull fractures), asplenia, HIV, cochlear implants Other Pathogens: GN bacilli • Neonatal GN sepsis/meningitis is most commonly due to E.coli – K1 capsular polysaccharide antigen is a marker of neurovirulence • Outside of neonates, GN meningitis is often nosocomial – Associated with GI infections, head trauma, NS procedures, immune deficiency – Klebsiella, Salmonella, Enterobacter, and Pseudomonas Klebsiella Ventriculitis/Abscess Other Pathogens: GBS • Still a common cause of invasive neonatal disease • Six main serotypes: Type III causes most neonatal meningitis • Incidence is down in developed countries due to screening and treatment of pregnant women GBS Meningitis with Infarcts Other Pathogens: Listeria • Listeria monocytogenes is a Gram positive rod and still an important cause of neonatal sepsis • Can also be seen in older children with cellular immune deficiencies • Associated with maternal consumption of unpasteurized cheese or contaminated meats Other Pathogens: Anaerobes * Anaerobic meningitis occurs in only in certain conditions Rupture of brain abscess Chronic otitis, mastoiditis, sinusitis Head trauma, NS procedures Congenital dural defects GI infections, suppurative pharyngitis CSF shunts Immune suppression * Includes Bacteroides fragilis, Fusobacterium spp., Clostridum spp Pathogenesis Pathophysiology * With acute CNS infection there is loss of autoregulation: Early increase in CBF, followed later by a decrease At risk for global cerebral hypoperfusion * Focal hypoperfusion can result from vasculitis leading to ischemia Can occlude large vessels: carotid, MCA, ACA * Cerebral edema can be vasogenic, cytotoxic, or interstitial Interstitial edema is the main cause of obstructive hydrocephalous in meningitis Cerebral Edema Clinical Presentation • Depends on the age of the patient and the offending organism – Generally more abrupt onset than viral • Infants have a variable presentation – Fever, poor feeding, lethargy, irritability, high-pitched cry, full fontanelle • Older children may have acute onset of fever, HA, vomiting, photophobia, and altered mental status – +/- Kernig or Brudzinski sign Clinical Presentation *Seizures may be the presenting feature in nearly 1 in 6 children Have a low index of suspicion with seizures + fever *Papilledema is uncommon at presentation *Focal signs can be found in 14% of cases Sudural epyema, cortical infarction, cerebritis *Rashes are not uncommon Petechial or purpuric rash highly suggests meningococcemia Diagnosis * Definitive diagnosis is by analysis and culture of the CSF LP should be done at earliest opportunity Do not delay antibiotics – may alter culture and gram stain but chemistry or cells * WAIT on the LP if: Evidence of raised ICP (pupil changes, cushing’s, kussmaul pattern, deep coma), focal neuro exam, resp/CV instability, coagulopathy Get a head CT if there is focality or question about diagnosis Diagnosis • CSF findings include high opening pressure, pleocytosis, low glucose, and high protein – Cloudy CSF with high opening pressure is diagnostic – Glucose ratio of 0.4 is 80% sensitive and 98% specific • CSF WBC (predicted) = CSF RBC x (blood WBC/blood RBC) – Observed CSF WBC/ predicted <0.01 and WBC/RBC ratio of <0.01 are 100% reliable in ruling out bacterial meningitis Diagnosis • Gram stains are quick, cheap, and accurate – 90% strep, 86% H. flu, 75% neisseria, 30% Listeria • CSF culture will be positive in the majority of untreated cases • Empiric diagnosis can be made if: – CSF WBC > 300, with >60% poly’s – Glucose < 50% of serum – Absolute glucose < 30 Diagnosis: Viral vs. Bacterial * Latex agglutination Helpful in partially treated meningitis Specific but not that sensitive Strep pneumo – 96% specific, 70 -100 % sensitive * PCRs are available for neisseria and pneumococcus Both are sensitive and specific DNA load correlates with mortality for neisseria Very expensive * CRP may be helpful but only if very high or very low * Peripheral WBC, CSF lactate, limulus amebocyte lysate, procalcitonin, and various cytokines are up in the air Complications • • • • • • • • • Raised ICP Seizures Subdural empyema Infarcts Cerebritis Brain abscess Hydrocephalous, ventriculitis Cranial nerve involvement Sensorineural hearing loss Treatment: By Age Age Common pathogens Antimicrobial Therapy < 1 month GBS, E. coli, Listeria, Klebsiella Amp + cefotaxime or an aminoglycoside 1-23 months S.pneumoniae, N. meningitidis, Vanc + 3rd gen GBS, H.flu, E.coli cephalosporin 2-50 years N. meningitidis, S. pneumoniae Vanc + 3rd gen cephalosporin > 50 years S. pneumoniae, N. meningitidis, Listeria, GN bacilli Vanc + amp + 3rd gen ceph Treatment: Head Trauma Type of Trauma Pathogens Antimicrobial Therapy Basilar skull fracture S.pneumo, H.flu, group A strep Vanc + 3rd gen ceph Penetrating trauma S.aureus, coag-neg staph, GN bacilli (Pseudomonas) Vanc + cefepime, ceftaz, or meropenem Post-neurosurgery GN bacilli, S. aureus, coag-neg staph Vanc + cefepime, ceftaz, or meropenem CSF shunt Coag-neg staph, GN bacilli, propionibacterium acnes Vanc + cefepime, ceftaz, or meropenem Duration of Therapy Organism Length of Treatment Neisseria meningitidis 7 days Strep pneumoniae 10-14 days GBS, Listeria, GN’s 3 weeks minimum Other Considerations • In developing countries, ampicillin and chloramphenicol are sometimes used due to the high cost of cephalosporins – Increasing resistance of H.flu to ampicillin, but it is via B-lactamase production – Remember that strep and meningococcus resistance is by alteration of penicillin binding proteins • Meropenem and newer fluoroquinolones are as effective as cephalosporins, but still are not 1st line – Meropenem is good for ESBLs Other Considerations • With treatment CSF culture and Gram stain will become negative in 24-48 hours – Glucose will normalize in 72 hours – Cells and protein take days • Fever may persist for 7-10 days (H.flu), but beyond this consider other factors – Thrombophlebitis, spread of infection, empyema, drug fever – A recurrence of fever may also indicate a complication or a secondary nosocomial infection Do we need a repeat LP? • Repeat LP’s are not routinely necessary if the patient gets better and is afebrile – EXCEPT for neonatal GN meningitis • Consider repeat LP in these situations: – No clinical improvement after 3-4 days of abx – NEW focal neuro signs, AMS, or increased ICP – Initial culture had resistant/weird bugs and no improvement after 24-48 hrs of appropriate therapy Should we give steroids? * Inflammatory cascade in bacterial meningitis leads to tissue damage and can worsen neurologic sequelae Antibiotics make this worse * Steroids can decrease inflammation, ICP, cerebral edema, and CSF outflow obstruction * Dexamethasone given to patients with H.flu or pneumococcal meningitis has shown benefit * The AAP recommends its use in H.flu meningitis 0.4 mg/kg q12h x 2 days * Adult guys give it when strep pneumo is suspected Consider adding rifampin? * The benefits of steroids have NOT been established in neonatal meningitis Prognosis • Mortality continues to be as high as 15-20% • Coma, raised ICP, seizures, and shock are significant predictors of morbidity and mortality • Neurologic sequelae are common – Hydrocephalous, spasticity, vision/hearing loss, cognitive defects, developmental delay Prevention • Isolation is necessary for H.flu and Neisseria for the first 24 hours of treament • Rifampin prophylaxis is indicated for household contacts of H.flu if any of them is unvaccinated and <4yrs old • Rifampin is also recommended for household and daycare contacts of Neisseria – Single oral dose of cipro or azithro is ok for adults Prevention • H.flu vaccine is awesome and has virtually eliminated H.flu meningitis in developed countries • Heptavalent pneumococcus vaccine is good too – Don’t forget kids with asplenia, nephrotic syndome, sickle cell, and cochlear implants need 23-valent • Quadrivalent meningococcal vaccine (A, C, Y, W135) is recommended for high risk kids > 2 yrs and college students/military TITLE • INFORMATION 47