Cerebral Dysfunction - Georgetown University
advertisement
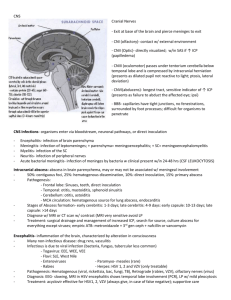
Cerebral Dysfunction Lauren Walker, RN, BSN Georgetown University Overview Topics • • • • • Increased Intracranial Pressure Level of Consciousness Cerebral Abnormalities Nervous System Tumors Infections Pediatric Cerebral Dysfunction General Information • Children under the age of 2 require special evaluation for neurologic function – Observation of fine and motor reflexes – Pregnancy and delivery history • General Assessment – Family History – Health History – Physical Evaluation Abnormal neurologic physical evaluations of infants • • • • Size and shape of head Sensory responses Spontaneous activity Symmetry in extremity movement • Frequent movement of extremities • Skin and hair texture • Distinctive facial features • • • • • High-pitched, piercing cry Abnormal eye movements Inability to suck or swallow Lip smacking Asymmetric facial movements • Yawning • Muscular activity and coordination • Level of development Increased Intracranial Pressure • Brain is enclosed in the solid bony cranium • Cranium’s total volume: – Brain: 80% – Cerebrospinal fluid (CSF): 10% – Blood: 10% • Volume must remain approximately the same at all times • Brain is terrible at compensation! • Normal ICP 5-10 ICP Video Clinical s/s of Increased ICP Infants • • • • • • • • • Tense and/or bulging fontanel Separated cranial sutures Irritable High-pitched cry Increased occipital circumference Distended scalp veins Changes in feeding Crying when disturbed Setting-sun sign • • • • • Children Headache Nausea Vomiting Diplopia, blurred vision Seizures Box 28-1, Chapter 28 Wong Clinical s/s of Increased ICP Personality and behavioral signs • • • • • • • • Irritability, restlessness Indifference, drowsiness Decline in school performance Diminished physical activity and motor performance Increased sleeping Memory loss Inability to follow simple commands Lethargy and drowsiness Late signs • Bradycardia • Lowered level of consciousness • Decreased motor response to commands • Decreased sensory response to painful stimuli • Alterations in pupil size and reactivity to light • Flexion and extension posturing • Cheyne-stokes respirations • Papilledema • Coma Box 28-1, Chapter 28 Wong Level of Consciousness Earliest indicator of improvement or deterioration • Determined by observations • Physical Assessment – Motor activity, reflexes, vital signs • • 15 points- highest score, unaltered LOC 3 points- lowest score, deep coma http://www.eguidelines.co.uk/eguidelin esmain/gip/media/images/barclay_glas gow_comascore2.gif Nursing Management of ICP • • • • • • Positioning Alternating mattresses Avoid causing pain Cluster care Minimize environmental noise Closely monitor nutrition and hydration Nursing Management of Increased ICP • Indications for inserting a monitor: – GCS of 8 or below – Deterioration – Judgment from clinical appearance and response • Monitors: – – – – Intraventricular catheter Subarachnoid bolt Epidural sensor Anterior fontanel pressure monitor Medications for Altered ICP • What is the cause? – Corticosteroids: inflammation – Antibiotics: infectious process – Diuretics: edema – Antiepileptic: seizure activity – Sedation: combativeness – Barbiturates: deep coma Cerebral Malformations • Newborn cranial sutures are separated by membranous seams Sutures: Soft areas: -Sagittal -Anterior fontanel -Coronal -Lambdoidal -Posterior fontanel Eight weeks: Posterior fontanel closed Six Months: union of suture lines Eighteen Months: Anterior fontanel closed After 12 years: sutures unable to be separated by increased ICP Hydrocephalus “water on the brain” • Imbalance in the production and absorption of CSF in the ventricular system • Causes: – Impaired absorption of CSF fluid – Obstruction of flow through ventricle • Brain structures become compressed • Most cases are from developmental defects Diagnosing Hydrocephalus • Time of onset and preexisting lesions – Infants: Head circumferences and neuro signs • CT • MRI Clinical Manifestations of Hydrocephalus Infancy (early) Infancy (later) Infancy (general) Childhood Abnormal rapid head growth Frontal enlargement Irritable Headache on awakening Bulging fontanels Depressed eyes Lethargy Papilledema Dilated scalp veins Sun-setting sign Cries when picked strabismus up or rocked Separated sutures Pupils sluggish Infantile reflexes persist Irritable Macewen sign Change in LOC Lethargy Thinning of skull bones Lower extremity spasticity Confusion/ incoherence Difficult suck and feeding vomiting Box 28-13, chapter 28, Wong Management of Hydrocephalus • Direct removal of obstruction • Placement of shunt – Ventriculoperitoneal shunt (VP shunt) – Associated with infection and malfunction High success rate with surgically treatment Shunting Shunting Video Family Support • • • • • • Coping is difficult with patents Feel guilty, anxious Uncertain outcome Continue to educate family Include family in patient care Possibility of long term rehabilitation Nervous System Tumors • CNS tumors account for 20% of all childhood cancers • 3.3 cases per 100,000 occur in kids under 15 years old • Difficult to treat • No dramatic advancements or improvements seen vs other childhood cancers Brain Tumors • Most common solid tumors in children • Infratentorial (60%) – Primairly in brain stem or cerebellum – Usually see increased ICP (medulloblastoma, cerebellar astrocytoma, brainstem glioma) • Supratentorial – Mainly cerebrum (astrocytoma, hypothalamic tumors, optic pathway tumors) Brain Tumor Diagnostics • s/s are related to: – Location – Size of tumor – Child’s age • Most common signs: Headache, vomiting • s/s are vague and can be overlooked • Detected by: – MRI – CT scan • Official diagnosis with biopsy from surgery Treatment of Brain Tumors • Treatment of choice = total removal of tumor without neurologic damage – Surgery, radiotherapy, chemotherapy • Prognosis: – Depends on size, tumor type, extent of disease Nursing Management of Brain Tumors • Establish a baseline assessment • Vital signs – Look for sudden variations • • • • • Frequent neurologic assessments Headache? Vomiting? Seizures? Child’s behavior positioning Postoperatively check muscle strength when awake Intracranial Infections • Nervous system is limited in ways to respond to an infection • Inflammatory process in brain affects: – Meninges (meningitis) – Brain (encephalitis) • Meningitis has many origins Bacterial Meningitis • Definition: acute inflammation of the meninges and CSF • 10-15% of cases are fatal • Caused by many bacterial agents – H. Influenzae type b, S. pneumoniae, Neisseria Meningitidis • Vascular dissemination or direct implantation • Infective Process Clinical Manifestations of Bacterial Meningitis Children and Adolescents (Classic picture) • • • • • • • • Abrupt onset, rash Fever, chills, headache Alteration in senses Seizures* Irritability/agitation Nuchal rigidity Positive Kernig & Brudzinski signs • • • • • • • Infants and Young Children Fever Poor feeding Vomiting Irritable Frequent seizures Bulging fontanel Difficult to evaluate in this age group Box 28-5, Chapter 28 Wong Clinical Manifestations of Bacterial Meningitis Neonates: Specific Signs • Very hard to diagnose • Well at birth- behaves poorly a few days later • Refuses feeds • Poor sucking • Vomiting/diarrhea • Poor tone • Lack of movement • Weak cry • Supple neck Neonates: Nonspecific Signs • Hypothermia/fever • Jaundice • Irritable • Drowsiness • Seizures • Respiratory irregulations • cyanosis Box 28-5, Chapter 28 Wong Diagnostic and Therapeutic Management of Bacterial Meningitis • • • • • Lumbar Puncture Elevated WBC count Decreased Glucose level Considered a medical emergency! Initial management: – Isolation, iv antibiotics, fluids, monitored, treatment of complications Management of Bacterial Meningitis • • • • • • Hydration Quiet, decreased stimulation Side lying position Correct electrolyte imbalance Measure for s/s increased ICP Monitor for complications • Prevention: – Vaccines for children starting at 2 months Nonbacterial (aseptic) Meningitis • • • • • Caused by many viruses! Abrupt or gradual onset Symptoms develop 1-2days after onset s/s vague Diagnosis is based on pt assessment and CSF findings • Systematic treatment • Nursing care similar to bacterial meningitis Encephalitis • Definition: inflammatory process of the CNS which is caused by a variety of organisms – Virus invades CNS or postinfection after a viral disease – Cause in typically unknown Clinical Findings of Encephalitis • Initial findings are nonspecific • Evolve to demonstrate neuro s/s – Seizures, abnormal CSF – Mild s/s for a few days, rapid recovery, to fulminating encephalitis with CNS involvement Onset Malaise Fever Headache/Dizziness Lethargy Neck Stiffness Nausea/Vomiting Tremors Speech Difficulties Altered Mental Status Severe Cases High Fever Stupor Seizures Disorientation Spasticity Coma Paralysis Diagnosis and Management of Encephalitis • Based on clinical findings • CT in late stages • Some viruses are found in CSF • Hospitalized for observation with supportive treatment • Prognosis depends on age, organism, neurologic damage • http://www.youtube.com/watch?v=8tf5VewEf Gs http://www.youtube.com/watch?v=Qmym2iFV Nw8&feature=related