central nervous system infections
advertisement
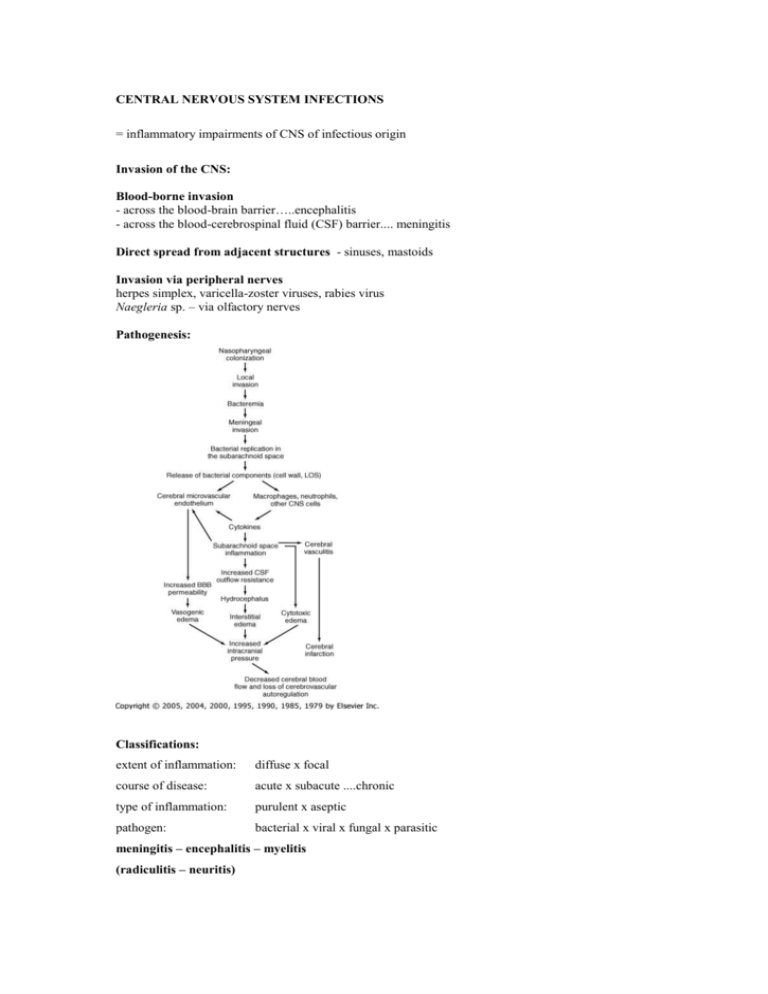
CENTRAL NERVOUS SYSTEM INFECTIONS = inflammatory impairments of CNS of infectious origin Invasion of the CNS: Blood-borne invasion - across the blood-brain barrier…..encephalitis - across the blood-cerebrospinal fluid (CSF) barrier.... meningitis Direct spread from adjacent structures - sinuses, mastoids Invasion via peripheral nerves herpes simplex, varicella-zoster viruses, rabies virus Naegleria sp. – via olfactory nerves Pathogenesis: Classifications: extent of inflammation: diffuse x focal course of disease: acute x subacute ....chronic type of inflammation: purulent x aseptic pathogen: bacterial x viral x fungal x parasitic meningitis – encephalitis – myelitis (radiculitis – neuritis) Clinical symptoms: meningeal syndrom - triad of symptoms: 1) constant and severe headache, aggravated by movement 2) nauzea, vomiting 3) positive meningeal signs: neck stiffness, Brudzinski I spine sign, Kernig I, Amos Lassegue, Kernig II fever signs of cerebral dysfunction – declining level of consciousness (somnolence, sopor, coma), confusion, seizures, palsies, tremor, ataxia, hypersensitivity (photophobia) signs of increased intracranial pressure and brain stem impairment – coma, hypertension, bradycardia, n III palsy petechiae (purpura) in meningococcal disease Clinical diferencies: purulent meningitis aseptic meningitis symptoms duration: 1 – 2 days several days, two-phase illness history: otitis, sinusitis, head trauma, recent tick-bite shunt, immunodeficiency consciousness impaired: common and severe, comma less frequent,mild, somnolence meningeal signs: highly positive mild to moderate, but tremor, ataxia, nystagmus brain edema moderate to severe mild to moderate progress rapid slow Cerebrospinal fluid changes during CNS infections cells per mm3 protein g/L glucose mmol/L 0,1 – 0,4 2,2 – 4,2 Purulent meningitis 0–5 lymphocytes thousands mainly neutrophils Aseptic meningitis (meningoencephalitis) hundreds < 1000 (2000) mainly lymphocytes Fungal meningitis tens-hundreds mainly mononuclears Normal ↑↑↑ 1 ↓↓ pathogen bacteria amoebae ↑ 0,4 – 1 ↔ viruses spirochetae ↑↑ ↓ fungi (Cryptococcus) PURULENT MENINGITIS Etiology: bacteria: predisposing age: Streptococcus pneumoniae - any age except for neonates Haemophilus influenzae type b - 3m – 5y Neisseria meningitidis - 1 – 4y, 15 – 19y, any age Predisposing factors for specific pathogens: neonatal age – Streptococcus agalactiae (group B), E.coli, other Enterobacteriacae (Klebsiella), Listeria monocytogenes, Enterococcus sp. otitis media, mastoiditis, sinusitis – S.pneumoniae, H. influenzae penetrating head trauma or neurosurgery – S.aureus, S.epidermidis, gram-negative bacilli closed head trauma (skull-base fr.) - S.pneumoniae CSF shunt – S.epidermidis, S.aureus, gram-negative b. (Pseudomonas) immunocompromised host – Listeria monocytogenes, fungi (Cryptococcus) Mycobacterium tuberculosis endocarditis, spondylodiscitis – S.aureus Rare: Mycobacterium tuberculosis fungi: Cryptococcus neoformans parasites: free-living amoebae – Naegleria fowleri, Acanthamoeba , Balamutia mandrilaris Toxoplasma gondii Pathogenetic classification: 1. primary meningitis – no preceding focus of purulent inflammation, organisms spread via blood (N.m., H.i.) or along neural fibres (naegleriae) from mucosal surface, a viral infection may precede 2. secondary meningitis – bacteria spread from pre-existing focus (S.p., S.a., gramnegatives) Diagnosis history, clinical signs, neurological examination CSF test: cytology, biochemical tests etiology: CSF - Gram stain (microscopy), culture, PCR, latex agglutination blood – culture, PCR, latex agglutination inflammation markers: ESR, leukocytosis + left-shift, CRP if papilloedema, focal neurological signs, focus in sinus or mastoid - CT, MRI Treatment: Antibiotics - bactericidal, well penetrating HLB: ceftriaxon, cefotaxim benzylpenicillin (penicillin G) chloramphenicol Corticosteroids – antiinflammatory and antiedema effects: dexamethason 0,15mg/kg q 6h or 0,4mg/kg q12h, for 2 or 4 days, confirmed benefit in haemophilus and pneumococcus meningitis Treatment of brain edema: - corticosteroids - hyperosmolar agents (mannitol) - strict bed rest, head elevation 30 degrees, sedation Supportive care: adequate oxygenation, adequate blood pressure (crystaloids, colloids, catecholamines) to keep sufficient cerebral perfusion pressure and brain O 2 supply (if severe intracranial hypertension, ICPmonitoring recommended ) Symptomatic therapy: sedatives, anticonvulsants, analgesics, antiemetics, antipyretics Focus sanation – mastoidectomy, sinus surgery Complications: subdural effusion thrombophlebitis of cerebral vessels and venous sinuses brain abscess symptoms: focal neurological signs, fever, impaired consciousness, persisting/worsening CSF inflammation Sequelae: hear imparment - partial or total deafness cranial nerve paresis encephalopathy – sleep and memory disturbancies, concentration and learning disabilities Our strategy: Clinics: meningeal syndrom + fever = suspected meningitis Aseptic or purulent meningitis? History: recent tick-bite, recurrent otitis media, head trauma, immunosupression, physical overload… Symptoms duration: hours = primary purulent meningitis days = aseptic meningitis/meningoencephalitis secondary purulent meningitis If history, clinical signs (and elevated inflammatory markers) evoke suspicion of purulent meningitis, it is necessary to confirm or exclude this dg., as the treatment has to start within 30 minutes after admission!!! Emergent: fundoscopy lumbar puncture + CSF tests: leukocytes, protein, glucose, lactate Gram-stain immediately, if available latexagglutination culture + PCR blood culture Treatment: 1. Dexamethason i.v. 16mg first dose, continue 8mg q6h, next dosage depends on the course 2. Antibiotic – start empirically, consider the most likely pathogens: ceftriaxon 100mg/kg/24h up to 6g in 1-2doses, cefotaxim 200mg/kg/24h up to 12-16g in 4doses, chloramphenicol 12g/24h in 3doses, meningococcus – benzylpenicillin 20milU/24h in 4doses (neonate – different clinics, different pathogens, different treatment!!) 3. Manitol 20% 100-150ml q6h for 10-15min (not immediately after ATB) + necessary supportive care and symptomatic treatment BRAIN ABSCESS Diagnosis: if abscess suspected, LP is contraindicated (CSF test rarely helpful) CT – ring-enhancing lesion with surrounding edema blood culture, other sites cultures Treatment: small abscess – conservative, large – surgery CEF III + MET or CMP, guided by microbiological results anticonvulsants, mannitol, (corticosteroids decrease edema, but may delay resolution) surgery – aspiration or open drainage MENINGITIS IN NEONATES Etiology: group B streptococci, E.coli, other aerobic gram-negative bacilli (Klebsiella), Listeria monocytogenes, Enterococcus sp. Clinical signs – nonspecific: poor feeding lethargy or irritability, strange cry (high-pitched voice) hypothermia rather than fever hypotonus vomiting convulsions bulging fontanelle neck stiffness, opisthotonus Treatment: cefotaxim 200mg/kg/24h + ampicillin 400mg/kg/24h alternative: ampicillin + gentamicin 5mg/kg/24h Sequelae: hydrocephalus mental and motoric retardation deafness, blindness convulsions (epilepsy) Neisseria meningitidis INFECTION 13 serogroups, A,B,C,Y, W135 – 95% of cases Clinical forms: 1. superficial infection: pharyngitis, conjunctivitis 2. invasive disease: meningitis, sepsis, mixed form Meningococcal invasive disease: History: physical overload, sudden onset, nonspecific flu-like symptoms – fever, malaise, in meningitis inreasing headache, vomiting and altered consciousness, in sepsis general dyscomfort, myalgia, diarhea, in both rash - early maculopapular, later haemorhagic – petechiae, ecchymoses Clinics: sepsis – fever, haemorhagic rash, septic shock (tachycardia, hypotension, tachypnea, cold acra, cyanosis, oliguria), altered mental status (restlessness, confusion) meningitis – fever, meningeal syndrom,decreased consciousness mixed form – more or less like sepsis plus signs of meningitis Diagnosis: blood tests: blood count + differential leuko acid-base balance, G, Na ,K ,Cl , urea, creatinine, lactate, protein, albumin, bilirubin, AST, ALT, CRP coagulation – aPTT, PT (Quick), AT III, DD, fibrinogen blood culture, PCR CSF tests (if LP indicated): WBC, biochemical – P, G, L, Cl – microscopy, culture, (latexagglutination), PCR Treatment: 1. treatment of sepsis and septic shock 2. treament of meningitis ATB: cefotaxim, ceftriaxon benzylpenicillin chloramphenicol Complications: aseptic arthritis serositis – pericarditis (perimyocarditis), pleuritis neurological sequelae – deafness, other cranial nerve lesions peripheral gangrene (purpura fulminans), loss of digits, extremities fulminating sepsis with septic shock and MODS (multiple organ system failure = DIC, ARDS, cardiac and circulatory failure, ARF, GIT, liver, encefalopathy) autopsy dg.: Waterhouse-Friedrichsen syndrome – haemorhagic necrosis of adrenal glands Prevention: vaccination - indicated for persons at particular risk: military recruits, local epidemic, asplenic patients, complement deficiences esp. C5-C9, travellers to the African meningitis belt and pilgrims visiting Mecca - polysacharide group A,C,Y,W135 vaccines - conjugate C vaccines – capsular polysacharide conjugated with immunogenic proteins such as diphtheria or tetanus toxoids chemoprophylaxis - household and kissing-contacts in 10 days preceding disease: oral penicilin or cef I, macrolide, rifampicin, ciprofloxacin ASEPTIC MENINGITIS, MENINGOENCEPHALITIS Etiology: viruses: enteroviruses: Coxsackie, ECHO arboviruses: alphaviruses, flaviviruses - tick-borne Central European encephalitis, Russian SpringSummer encephalitis, louping-ill in Scotland, Eastern and Western equine, St.Louis encephalitis, Japanese B encephalitis respiratory viruses: parainfluenza, influenza, adenoviruses, RSV herpesviruses: HSV 1,2, VZV, CMV, EBV, HHV6 viruses occuring very rarely due to vaccination: polio, mumps, measles, rubella, rabies virus lymphocytic choriomeningitis virus bacteria: spirochetae: Borrelia (Lyme borreliosis), Leptospira: all species, Treponema pallidum (lues) Mycoplasma pneumoniae rickettsiae: Coxiella burneti (Q-fever) Diagnosis: history, clinical symptoms CSF test: cytology, biochem tests etiology: serology - TBE, LB, leptospirosis, respiratory viruses PCR - HSV DNA in CSF, LB DNA in blood, CSF virus isolation – CSF, nasopharynx, stool (enteroviruses) other screening tests (blood count, CRP, ions, kidney and liver tests) Treatment: symptomatic therapy: bed rest antipyretics, analgesics, antiemetics treatment of brain edema supportive care causative therapy: HSV encephalitis, Lyme borreliosis Herpes Simplex Virus Encephalitis Etiology: HSV 1, 2 Pathology: focal necrotizing inflammation of brain tissue, often haemorrhagic, uni/bilateral, temporal and frontal lobes Clinics: the onset abrupt or insidious symptoms: fever, headache focal signs – speech disturbancies (aphasia, dysphasia), paresthesia, convulsions, behaviour abnormalities, personality changes progressive loss of consciousness…coma Diagnosis: emergent CT or MRI !!! normal CT scan does not exclude dg!!! EEG CSF test – aseptic inflammation, erythrocytes PCR - HSV DNA in CSF (brain biopsy for histology and viral culture) serology – not sufficiently sensitive, late dg. Treatment: acyclovir 10 mg/kg q 8h i.v. 21-28days symptomatic supportive care Fungal meningitis Cryptococcus neoformans An ubiquitous agent, infection by inhalation. Disseminated infection in patients with lymphoma, AIDS or on steroid therapy. Clinics: insidious development of symptoms headache, irritability, memory and behavior disturbances focal neurological signs fever and meningeal signs may be missing Laboratory: CSF – lymphocytes, protein, glucose CSF stained with India ink for cryptococcus capsule cryptococcus antigen in CSF and blood culture - CSF, blood, sputum, urine Treatment: amphotericin B + 5-fluorocytosin 6-10 weeks AIDS pts – prophylaxis with amfo B o.w. + fluconazol daily Amoebic meningoencephalitis Free-living amoebae – Naegleria fowleri By 1997 totally 180 cases, 7 survived. Distributed worldwide, most often in swimming-pool water. Clinics and CSF signs similar to purulent meningitis Laboratory: microscopical detection of amoebae in fresh CSF culture Treatment: Amphotericin B + Rifampicin + Miconazol i.v.+i.th. Granulomatous encephalitis - Acanthamoeba, Balamutia mandrilaris Polyradiculoneuritis – Guillan-Barré syndrome Acute demyelinating disease. Etiology not clear, immunopathological response to infection, some evidence for: Campylobacter jejuni, Mycoplasma pn., Borrelia burg., CMV, EBV, HIV, rare complication of chickenpox, measles, influenza A vaccine. Clinics: 1-2 weeks after upper resp. tract or diarheal illness symmetrical sensory and motor loss beginning on distal parts of the limbs (“glove and stocking”) ranging from weakness to plegia, slowly ascends to trunk and respiratory muscles, bulbar palsy Dif.dg.: poliomyelitis, diphtheric polyneuritis, transversal myelitis Dg.: CSF - proteocytological dissociation – protein, normal leukocyte count and glucose Treatment: plasmapheresis or high-dose intravenous immunoglobulins supportive care long-term rehabilitation