CRYPTOCOCCAL INFECTIONS
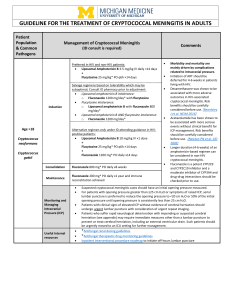
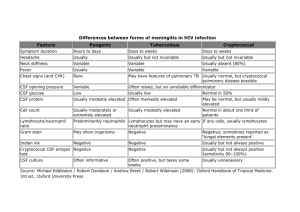
advertisement

CRYPTOCOCCAL INFECTIONS IN PATIENTS WITH AIDS Stephen J. Gluckman, M.D. Botswana-UPENN Partnership Microbiology • Encapsulated yeast • 4 serotypes – A (C. neoformans v grubii) – B and C ( C. gatti) – D (C. neoformans v neoformans) • All types can cause human disease • Life cycle – Asexual: yeast that reproduce by budding • Human infections – Sexual: only seen in the laboratory Ecology and Epidemiology • World wide – C. neoformans associated with bird droppings – C. gatti not associated with birds, associated with eucalyptus trees • Generally an infection of immunocompromised but can cause clinical disease in healthy persons – Decreased Cell-mediated immunity • AIDS – CD 4 usually < 100 • Prolonged corticosteroids • Organ transplant Ecology and Epidemiology • 15-30% of AIDS patients in Sub-Saharan Africa* • Much less common in children • No person to person transmission *Powderly, WG Clin Infect Dis 1993 Clinical Presentations • Pulmonary – Asymptomatic nodule – Symptomatic: not distinguishable from other causes • History, PE, routine laboratory testing does not produce features peculiarly suggestive of cryptococcal infection – Diagnosis • Staining of biopsy specimen • Culture of sputum and/or blood • Serum cryptococcal antigen (CRAG) – All patients with pulmonary disease need a CSF examination to r/o sub clinical meningitis Silver Stain Clinical Presentations • Cutaneous – Disseminated disease – Looks similar to molluscum contageosum – Diagnosis: • Unroofing a lesion and making a smear and culture • Serum CRAG – All patients with cutaneous disease need a CSF examination to r/o sub clinical meningitis Clinical Presentations • Cryptococcal Meningitis – Typical • Subacute onset of fever and headache • Photophobia and/or meningeal signs in only 25% – Less typical • • • • • Seizures Confusion Progressive dementia Visual or hearing impairment FUO – Diagnosis • CSF • Serum CRAG: > 99% sensitive in AIDS patients Cryptococcal Meningitis • In 2003 there were 193 (+) CSF cultures for cryptococcus from PMH * – Leucocytes • No leucocytes in 31% • Only 1-10 leucocytes in 23% • 7% had > 250 leucocytes – 30% of these had predominately PMN’s – 95% (+) India Ink – 1% (-) cryptococcal antigen • Literature – Sensitivity: 93-100% – Specificity: 93-98 % *Bisson et al India Ink Prognosis for Cryptococcal Meningitis • Prior to 1950 it was uniformly fatal • Amphotericin B introduced and mortality fell to the 3040% range • In 1970’s 5-FC was released – Not for monotherapy – Decreased relapse rate when used with Amphotericin B • Mortality with current regimens: 10% • Predictors of death – Altered mental status – CSF CRAG > 1024 – CSF cell count < 20 • Changes in serum CRAG titer do not correlate with clinical outcome. So no need to follow Summary of Diagnostic Options • Culture – White mucoid colonies within 48hours – Blood cultures often (+) in immunosuppressed patients • 2/3rds with meningitis • Tissue – Silver or mucicarmine stain • India Ink for CSF • Cryptococcal antigen – Serum and CSF are 99% sensitive in AIDS patients – Serum is less sensitive in normal hosts Cryptococcal Meningitis Treatment • Antifungal agents – Induction – Consolidation – Maintenance • Pressure management Treatment* *Modified IDSA Guidelines – Immunosuppressed (pulmonary, cutaneous, or meningitis) • Induction – Amphotericin B 0.7-1 mg/kg/day plus 5-flucytosine 100mg/kg/day x 2 weeks then • Consolidation – Fluconazole 400 mg/day x 6-10 weeks then • Suppression – Fluconazole 200 mg/day x ? Cryptococcal Meningitis Treatment One More Thing • Anti-fungal: induction, consolidation, maintenance • Pressure management – Elevated pressure • 75% > 200 • 25% > 350 – Repeated lumbar punctures • Increased pressure: daily until normal x several days • Normal pressure: recheck at 2 weeks prior to switching to fluconazole – Lumbar drain – VP shunt: if still elevated at 1 month – No role for • acetazolamide, mannitol – Steroids: ? Treatment • Other options – Fluconazole induction • Increased mortality • Not IDSA first choice – 5 FC monotherapy • Not an option because of resistance – 5-FC plus Fluconazole • Increased long term toxicity but an option – Caspofungin • No efficacy – Voriconazole • Good in vitro activity but little clinical experience Summary • Cryptococcal infections are common in patients with AIDS • In patients with AIDS cryptococcal infections are seen in patients with the lowest CD 4 (+) cell counts • Prolonged therapy and secondary prophylaxis is necessary • For meningitis both anti-fungal therapy and aggressive pressure management are required