Acute Intracranial Probs
advertisement

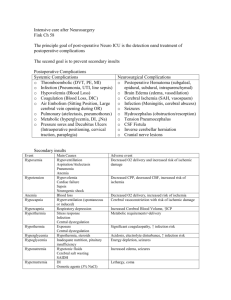
Acute Intracranial Problems Megan McClintock, MS, RN 11/4/11 Head Injury Head Injury Skull Fractures Basilar Frontal Temporal Parietal Posterior fossa Head Trauma Diffuse Injuries Concussion Diffuse axonal injury (DAI) Focal Injuries Lacerations Contusions Hematomas Cranial nerve injuries Complications Epidural hematoma Bleeding between the dura and the skull Arterial or venous Initial LOC, brief lucid interval, decrease in LOC Headache, nausea, vomiting Subdural hematoma Bleeding between the dura mater and the arachnoid layer Usually venous Acute, subacute, or chronic Symptoms similar to a stroke, TIA, or dementia Intracerebral hematoma Usually occurs in frontal or temporal lobes Diagnostic Studies CT MRI (for smaller lesions) Cervical spine xrays Most important to diagnose timely and get them to surgery (if needed) and keep ICP from increasing Craniectomy Craniotomy with surgical evacuation Hemicraniectomy Goals Maintain cerebral blood flow Remain normothermic Control pain Prevent infection Attain maximum cognitive, motor, sensory function Interventions Prevention Monitor for changes in neuro status Encourage family members to stay Lubricating eye gtts, tape eyes shut Do not allow fever or shivering Watch for otorrhea/rhinorhea HOB up Collection pad (no packed dressings) No NG tubes No sneezing or blowing nose No nasotracheal suction Brain Tumors Can occur anywhere Can be primary or secondary Brain Tumors Symptoms depend on location Dx studies – CT, MRI, no LP, biopsy Tx – surgical removal, VP shunt, radiation therapy, chemotherapy Cranial Surgery Burr hole Craniotomy Craniectomy Cranioplasty Stereotactic Shunt Interventions Hair is shaved in the OR Usually need ICU after surgery Prevention of increased ICP Frequent neuro assessments for first 48 hrs Closely monitor F&E status Prevention of pain and nausea HOB at 30 degrees (except for posterior fossa, burr hole) Do not position patient on operative side with craniectomy Brain Abscess Accumulation of pus within the brain tissue Sx – headache, fever, n/v, focal symptoms, s/s of ICP Tx – antimicrobial therapy, may need surgical drainage or removal (if encapsulated) If untreated, mortality is almost 100% Bacterial Meningitis Usually Streptococcus pneumoniae, Neisseria meningitidis, used to be Haemophilus influenzae Less common in summer MEDICAL EMERGENCY!!!! Sx – fever, headache, n/v, nuchal rigidity, photophobia, decreased LOC, ICP, skin rash Cx – neuro deficits, chronic headache, Waterhouse-Friderichsen syndrome Treatment Dx – blood culture, CT, LP (high protein, low glucose, purulent) Tx – immediate antibiotic therapy (after culture), may give decadron Interventions Prevention with immunizations Vigorous treatment of ear and resp infections Seizure precautions Codeine for pain Dark room, cool cloth, quiet, decreased stimuli Avoid restraints Family at bedside Control fever Respiratory isolation!!!! Viral Meningitis Also called aseptic meningitis Caused by a variety of viruses , sometimes through personal contact or by insects, most people have the viruses but don’t develop meningitis Usually mild and self-limiting Give antibiotics until you confirm that it is viral Only treat symptoms Encephalitis Acute inflammation of the brain Can be fatal Usually caused by a virus See as a complication of AIDS Sx – fever, headache, n/v, then CNS abnormalities Tx – may need ICU, antivirals, 1. Intracranial pressure monitoring is instituted for a patient with a head injury. The patient’s arterial blood pressure is 92/50 mm Hg, and intracranial pressure is 18 mm Hg. Using these values to calculate the patient’s cerebral perfusion pressure (CPP), the nurse determines that 1. the CPP is adequate for normal cerebral blood flow. 2. to prevent cerebral hypoxemia, the patient’s blood pressure should be increased. 3. the CPP is so low that ischemia and neuronal death are imminent. 4. lowering the patient’s blood pressure will reduce the intracranial pressure, increasing cerebral blood flow. 3. Management of the patient with bacterial meningitis includes 1. administering antibiotics immediately following collection of specimens for culture. 2. waiting for results of a CSF culture to identify an organism before initiating treatment. 3. providing symptomatic and supportive treatment because drug therapy is not effective in treatment. 4. obtaining skull x-rays and CT scans to determine the extent of the disease before treatment is started.