Diseases of the Eye CC

Diseases of the Eye
Casey Conway
Jeannie Stall , R.V.T. & ???
Credits : Clip Art graphics/Google images
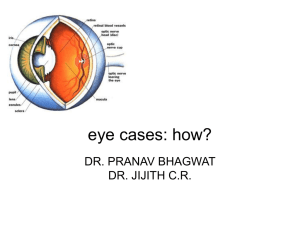
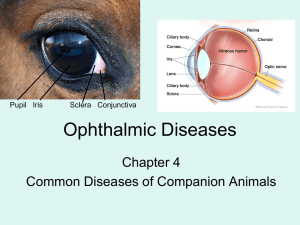
The Eye
• CDCA has great picture of a cross section.(hint)
• Most highly developed of all senses
• Most pets can live quality lives with a vision loss
• Proper diagnosis, quick treatment – Essential!
• 3 main categories of eye diseases:
▫ Accessory structures
▫ The globe
▫ The retina and the neural pathways
Anatomy Credits: ukvetsonline
Diseases of the Accessory
Structures
• Eyelids, conjunctiva, tear ducts, third eyelid, lacrimal glands
• Red eyes, blepharospasm (squinting), ocular discharge
• Common causes: Trauma & infection
• Conjunctivitis/Epiphora(overflow of tears)/
KCS (Keratoconjunctivitis sicca)/Cherry Eye
Conjunctivitis
• Inflammation of the conjunctiva
• Rarely a primary dz process
• Canine: can be non-infectious or infectious
Feline : is primarily infectious
▫ FHV – seen w/ Upper Resp. Tract symptoms
▫ Calicivirus
▫ Chlamydia psittaci
▫ Mycoplasmas
Conjunctivitis cont’d
• Clinical signs
▫ Chemosis (swelling)
▫ Hyperemia (redness)
▫ Ocular discharge
▫ +/- signs of URT dz
• Dx
▫ PE (thorough exam of conjunctiva/foreign body)
▫ Schirmer Tear Test, conj. scraping (cytology, c & s)
• Tx:
▫ Resolve underlying systemic dz.
▫ Topical antibiotic ointments/drops
▫ Nonsteroidal oint/drops may be needed
▫ Keep eyes clean and clear
• Prevent eye issues – riding out car window!
Epiphora
• Overflow of tears
▫ Overproduction (pain or irritation)
▫ Faulty drainage: (lacrimal duct blocked by swelling or trauma)
• Clinical Signs
▫ Watering of the eye
▫ Wet facial hair
▫ Secondary bacterial infection of facial skin
▫ Discoloration of the facial hair
Epiphora cont’d…….
• Dx:
▫ Eye exam
▫ Fluorescein dye
▫ Dacryocystorhinography ( Radiography of nasolacrimal duct )
• Tx:
Resolve primary cause of pain & irritation /
Flush lacrimal ducts / Surgery / Topical abx/ Trim hairs
Eyelid Diseases
• At the base of each eyelash is a sebaceous gland
Hordeolum: Meibomian gland abscess, usually caused by a staph. infection
Chalazion: When inflammation involves meibomian glands & granulation occurs
• Eyelid neoplasms : Older animals/ most are benign (cat usually malignant),
Squamous cell carcinoma most common tumor
Blepharitis:
Swelling of the eyelids
• Causes:
▫ Allergens
▫ Nutritional Deficiencies
▫ Viral
▫ Dermatitis from any cause
• Clinical signs
▫ Generalized swelling of lid
▫ Periocular pruritis (itchy eyes)
▫ Periocular alopecia ( hairloss)
▫ Rubbing of the eyes
Blepharitis Cont.
• Dx:
▫ Eye exam
▫ Skin scrape
▫ Fungal culture
▫ Bacterial cultures
• Tx: warm compresses
▫ Express hordeolum (staph infection)
▫ Surg. r emoval of chalazion (granulation tissue)
▫ Topical abx or systemic abx
▫ Corticosteroids ( Prednisolone)
▫ Antifungals ( Conofite or Tresaderm)
Blepharitis
Entropion
• Eyelids roll in against the cornea
• Common in dogs, not in cats
• 3 main forms:
▫ Congenital: breeds have large orbits with deep-set eyes, inadequate lid support, lid droops over the lower orbital rim and inverts – Collies, Great Danes, Irish
Setters, Dobes, Goldens, Rotts, Weim (primary lid deformities, poor ocular muscle development)
▫ Acquired nonspastic: surgical or traumatic – scarring of the lid with contraction – lid turns inward
▫ Acquired spastic – most common in cats – secondary to painful corneal lesions, conj. inflam. or both
Entropion
Entropion
• Clinical Signs
▫ Rolling inward of the lid margin(s)
▫ Epiphora (tear overflow)
▫ Chemosis ( conjunctiva swelling )
▫ Swelling
▫ Conjunctivitis
▫ Blepharospasm(eyelid muscle spasm)
▫ Pain
▫ +/- corneal ulceration
▫ Photophobia
Entropion Con’t……
• Dx:
▫ Observe lids interaction with globe
▫ Eye exam while awake
• Tx: Surgical correction
Ectropion:
Eyelids that roll outward, exposing the cornea
• Excessive lid droops outward
• Natural breed characteristic for:
Basset hounds, bloodhounds, cocker span, clumber span,
Eng. bulldogs, St. Bernards – usually asymptomatic
• All breeds: Secondary to muscular dz in senile dogs/
Dogs w/ surgical overcorrection of entropion
• Clinical signs
▫ Lid eversion
▫ Conjunctivitis
▫ Epiphora
▫ Keratitis
▫ Purulent exudate
Ectropion Cont.
• Dx:
▫ Observe lids
▫ Interaction with globe
▫ Eye exam while awake
• Tx: Surgical correction advised if clinical signs present
“Cherry Eye” or
Hypertrophy of Nictitans Gland
• Third eyelid:
▫ Protective structure/Spreads pre-corneal tear film
Covers eye to protect from injury/ Produces ~50% of lacrimal fluid
• Prolapse of 3 rd eyelid/gland: “passive forward displacement when eye withdrawn into orbit”
Hypertrophy of gland ONLY occurs in K9’s
• Etiology: Unknown cause
• Breeds: Basset, beagle, Boston, cocker
Cherry Eye
• Usually seen in young dogs (< 2 yrs. old)
-usually neoplasia if seen in old K9’s & cats
• Medial canthus is filled with red, swollen, third eyelid, resembles a small cherry
• Clinical signs
▫ Reddened enlargement of tissue in the medial canthus of the eye
▫ Mild irritation
▫ Usually no pain
▫ Epiphora ( tears)
▫ +/- conj. irritation
Cherry Eye continued…..
• Dx:
▫ Clinical signs
▫ Predisposed breed
▫ Rule out tumor (usually older dogs & cats)
• Tx:
▫ Surgical replacement of the gland, Tuck sutured
▫ Avoid excision – predisposes to KCS
– only excise in cases of neoplasia
• W/O sx., corneal damage can occur & may affect vision
Cherry Eye
Glaucoma:
• In healthy eye:
Aqueous fluid production =‘s aq. fluid amt. leaving eye, so IOP(intraocular pressure) remains fairly constant
• More aqueous fluid produced than leaves = glaucoma
• Normal k9/fel IOP range: 12-22 mm Hg w/ Tono-pen
• Most K9’s have decreased outflow, not increased prod.
• Primary – inherited defect (cocker, basset, chow)
• Secondary –drainage angle obstruction secondary to another dz.– ie: Neoplasia, uveitis, lens luxation, hemorrhage
Glaucoma cont’d
• Acute – elevated IOP (> 60 mm Hg ) can produce blindness within hours
Clin. signs: Ocular pain, vascular congestion, diffuse corneal edema, dilated pupil, sluggish or unresp to light,
+/- blind
• Chronic – painful, blind eye which is unresponsive to med. therapy. Make pet comfy w/salvage procedures
Clin. Signs: Enlarged lobe, corneal striae, optic disk cupping, pain, blindness
• Dx: IOP > 30 mm Hg,/ clin. signs/ r/o luxated lens
• Tx: Acute – true emergency – decrease IOP rapidly, sx
Chronic – sx – enucleation
• Bilateral disease – even if one eye is asymptomatic
Corneal Ulcers
Ulcerative Keratitis
• Cornea:Window of the eye- has 4 layers
▫ Epithelium
▫ Stroma
▫ Descemet’s membrane
▫ Endothelium
• Full-thickness loss of corneal epithelium exposing stroma
• Etiology: Trauma, chemicals, foreign body, prev. dz. ie:
KCS/ Herpes in cats, conformation issues, distichiasis (tiny, inwardly –facing meibomian gland hairs)
• Clinical signs
▫ Pain
▫ Epiphora
▫ Blepharospasm
▫ Conjunctival hyperemia
Corneal Ulcers
• Dx:
▫ Fluorescein dye- absorbed by stroma, not by epithelium (green uptake of dye)
WARN client about fluorescent green dye !!
• Tx:
▫ Topical Atropine
▫ Topical abx
▫ Sx
• Meds. w/ cortisone slow healing & makes condition worse
• Frequent re-evaluations needed to monitor progress/healing
Pannus:
Chronic Superficial Keratitis
• Superficial corneal vascularization & infiltration of granulation tissue (lymphocytes & plasma cells)
• Progressive, bilateral, degenerative, can result in blindness
• Cause – immune-mediated, animals at > 5000 ft most susceptible (G.shep, B. Terv, B. Collie, Greyh, SibHusky)
• C/S: breed predisposed with opaque lesion – pink or tan
• Dx: corneal scraping – infiltrate, eye exam
• Tx: Antiinflam. for life of patient, +/- subconj. inj., cryosurgery, superficial keratectomy
• No cure
Treatment to maintain regression of lesion is life-long
Pannus
“KCS”:
Keratoconjunctivitis Sicca
• Loss of both lacrimal glands
• Viral inf., drug-related toxicities, Imm-mediated dz, inflamm, breed predisp., congenital abn
• Most cases idiopathic, older >7 yr. – neutered
• Clinical signs
▫ Recurrent conjunctivitis
▫ Corneal ulcers
▫ Keratitis
▫ Cornea & conj. appear dull, dry, & irregular
▫ Ocular discharge
▫ Blepharospasm
▫ Crusty nares
KCS cont’d …..
• Dx:
▫ Schirmer Tear Test <15mm/min on repeat testing (k9 15-
25, fel 11-23) NOTE: Perform this test 1st
▫ 2 nd : Fluorescein dye –assess ulcer presence
• Tx:
▫ Stimulate tear prod. w/meds (cyclosporine)
▫ Topical art. tears
▫ Surgery if medical tx are unsuccessful
(parotid duct transposition)
• Failure to treat will result in blindness
Cataracts :
• Most common dz. involving the lens
• An opacity of the lens sufficient enough to cause a reduction in visual function – aging cells w/in lens become dehydrated & overlap each other, producing a central change in the reflection of light- lens may appear grey and opaque
• Freq. cause of blindness in dog, occas. seen in cat
• Etiology: Inherited, secondary to diabetes mel., hypocalcemia, trauma, nutritional deficiency, electric shock, uveitis, or lens luxation
(Photo Credits: dog-health-handbook.com )
Cataracts cont’d
• Clinical signs
▫ Progressive loss of vision
▫ Opaque pupillary opening
▫ Signs related to systemic dz. (diabetes mellitus or hypocalcemia)
• Dx:
▫ Complete eye exam/Assess via obstacle course/
Lack of menace /Failure to track visual responses
Photo Credits: petdig.com
Cataracts cont’d……..
• Pupillary light response is usually normal
• Tx:
▫ Sx removal
▫ Tx of any other dz
Anterior Uveitis
• Inflammation of the uvea (iris, ciliary body, choriod)
• Trauma, extension of local infx, foreign body, neoplasm, thermal trauma, parasites, protozoa
(bact, viral, mycotic dz – hematogenous spread)
• C/S: epiphora, photophobia, blepharospasm, +/vision defects, corneal edema, chemosis, prolapsed
3rd eyelid, pain, change in iris color
• Dx: c/s, hx, labs, x-ray, ultrasound, tonometry
• Tx: I.D. & elim. cause, control inflamm w/topical steroids (w/o tx, vision will eventually be lost)
Progressive Retinal Atrophy
• Group of hereditary retinal disorders seen in many breeds of dogs
(can occur in cats, but not as frequently)
• Toy poodles, min poodles, goldens, Irish sett, cockers, min sch, collies, samoyed, gordon sett,
Norw. Elkhound
• C/S: defective night vision, slowly progressive loss of day vision, cataract formation
• Dx: labs, eye exam of retina
• No Tx. currently exists
Horses
• Entropion
• Conjunctivitis – Summer/ dry, dusty condition /flies
• Corneal ulcers
• Cataracts – Sx. prognosis is good in foals
• Many blind horses can still be ridden safely, if owner doesn’t exceed horse’s ability & comfort level … (or the owner’s !)
“Moon Blindness”
Periodic Opthalmia, Recurrent Uveitis
• Comes & goes/ exact cause undetermined
• Many animals have high Lepto antibody titer
• Signs: cloudy eye, blepharospasm, excessive tears
• Dx: visualization of protein flare in fluid of anterior chamber, affected eye may be smaller, corneal stain, Lepto titer
• Tx: topical corticosteroids, atropine, banamine or Subconjunctival long-acting steroid injections
Sheep and Goats
• Entropion – most common ocular abnormality in neonatal lambs
• Infectious Conjunctivitis (Pinkeye) – responds well to medication – herd management
• Cataracts – most common lens abnormality in sheep and goats