RedEye111
advertisement

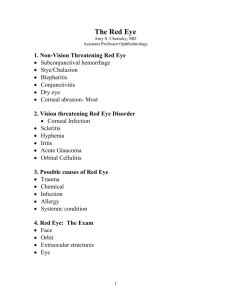
Red Eye GPVTS - November 2010 Overview • • • • History & Examination When to refer Causes or red eye Case studies Rectus muscle Ciliary Body Retina Iris Choroid Cornea Sclera Optic nerve Aqueous Lens Vitreous History • • • • • • • • • • • • • Onset Location (unilateral /bilateral /sectoral) Pain/ discomfort (gritty, FB sensation, itch, deep ache) Photosensitivity Watering +/or discharge Change in vision (blurring, halos etc) Exposure to person with red eye Trauma Travel Contact lens wear Previous ocular history (eg hypermetropia) URTI PMHx eg autoimmune disease Examination • • • • • • • • • Inspect whole patient Visual acuity- each eye + PH Pupil reactions + shape Lymphadenopathy- preauricular nodes Eyelids Conjunctiva (bulbar and palpebral) Cornea (clarity, staining with fluorescein, sensation) Fundoscopy Eye movements When to consider referral • • • • • Reduced VA Pain deep in eye Absent or sluggish pupil response Corneal damage on fluorescein staining History of trauma Differential (by structure) • Lids Pain 1. Blepharitis 2. Trichiasis 3. Chalazion/ Stye 4. Sub-tarsal foreign body +/+/+/+ Differential (by structure) • Conjunctiva & Sclera Pain 1. Bacterial conjunctivitis 2. Gonococcal conjunctivitis 3. Chlamydial conjunctivitis 4. Viral conjunctivitis 5. Allergic conjunctivitis 6. Subconjunctival haemorrhage 7. Episcleritis 8. Scleritis + Differential (by structure) • Cornea – Keratitis (pain) – Corneal abrasion / foreign body • Anterior chamber – Iritis (pain) • Glaucoma (pain) • Cellulitis (pain) • Shingles (pain) Blepharitis ►Symptoms Foreign body sensation/ gritty Itching Redness Mild pain ►Mainstays of treatment Lid hygiene, diluted baby shampoo Topical antibiotics Lubricants Trichiasis Inward turning lashes Aetiology: Idiopathic/ Secondary to chronic blepharitis, herpes zoster ophthalmicus Symptoms- foreign body sensation, tearing ►Treatment Lubricants Epilation Electrolysis- few lashes Cryotherapy- many lashes QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Chalazion Staphylococcal infection of meibomian gland Tender nodule within the tarsal plate May be associated cellulitis Treatment Hot compresses Topical antibiotic ointment Incision and drainage once the infection subsided Stye Bacterial abscess of hair follicle Tender nodule at lid margin Treatment: Hot compress Topical abx Epilation of lash Subtarsal Foreign Body History of foreign body Must evert eyelid Remove with cotton bud Stain with fluorescein +/- abx Conjunctivitis QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Conjunctivitis • Viral – Hx URTI, no photophobia, bilateral • Bacterial – Discharge, consider swab • Allergic – Itchy, atopy, NSAIDs, Antihist, Steroids • Chlamydial, Gonnococal – Sexually active, Swab, GUM referral Spontaneous subconjunctival haemorrhage • Painless red eye without discharge • VA not affected • Clear borders • Masks conjunctival vessels • Check BP • No treatment (lubricants) • 10-14 days to resolve • If recurrent: clotting, FBC • NB Remember base of skull fracture in trauma Episcleritis • Episcleral inflammation • Localized (sectoral) or diffuse • Symptoms/Signs: – Often asymptomatic – Mild tearing/ irritation – Tender to touch – Vessels blanch with phenylephrine • Self-limiting (may last for months) • Treatment – Lubricants – NSAIDS (Froben po 100mg tds) – Rarely low dose steroids (predsol) Scleritis Pain - often severe boring Ocular tenderness to movement and palpatation Photophobia Bluish-red appearance: Localised, diffuse or nodular Strong assosciation w/ autoimmune disease - esp RA Treat w/ NSAIDs, steroids Keratitis • • • • • • • • • Contact lens wear Chronic corneal disease Pain, discharge, FB sensation Decreased vision, photophobia Corneal ulcer may be visible Hypopyon Ofloxacin if bacterial - initially hourly Steroids afterwards can reduce scarring HSV - cold sores, run down, reduced corneal sensation - top aciclovir Corneal abrasion/ foreign body • • • • • • Hx foreign body Severe pain (worse on blinking) Watering ++ Remove FB w/ cotton bud Refer if crosses visual axis High impact w/out goggles exclude intraocular f/b- seidel test Anterior uveitis (Iritis) • Symptoms/Signs – – – – – Pain (ache) Photophobia Perilimbal conjunctival injection Blurred vision Pupil miotic / poorly reactive • Causes – 70 % idiopathic – Arthritic - HLA B27 – Infection • Treatment – Mydriatic + topical steroids Glaucoma - Acute Angle Closure • Opthalmic emergency • Peripheral iris blocking outflow of aqueous humour • Risk factors Shallow anterior chamber Age - ave 60 F:M 4:1 Hypermetropia FHx Asian 10 x caucasian Acute Angle Closure • Symptoms – severe ocular pain – headache – nausea and vomiting – decreased vision – coloured haloes around lights – Photophobia • Signs – – – – – – – semi-dilated non reactive pupil ciliary injection corneal oedema shallow AC Flare in AC raised IOP tense on palpation Acute Angle Closure • Treatment: – – – – – Medical: to lower the pressure IOP Topical steroid Iopidine pilocarpine Iv acetazolamide – Surgical: Laser iridotomy (curative in most cases) – Prophylactic to other eye NB It is very unusual for someone who has had an iridotomy to have angle closure again Pre-septal and Orbital Cellulitis • Orbital septum is a fibrous membrane that originates from the orbital periosteum and inserts into the anterior surface of the tarsal plate of the eyelid • Bacterial infection usually results from local spread of adjacent URTI • Preseptal usually follows periorbital trauma or dermal infection • Orbital most commonly secondary to ethmoidal sinusitis Pre-septal and Orbital Cellulitis • Preseptal infection causes erythema, induration, and tenderness of the eyelid • Amount of swelling may be so severe that patients cannot open the eye • Patients rarely show signs of systemic illness • Treatment - augmentin. Paeds refer Orbital Cellulitis • Additional signs seen which will not be present in preseptal cellulitis: – – – – proptosis chemosis ophthalmoplegia decreased visual acuity • Refer immediately Herpes Zoster • Crusting and ulceration of skin innervated by 1st division of trigeminal nerve • Lesions to tip of noseHutchinson’s sign, increased chance ocular involvement • Treatment - Oral aciclovir within 48hrs of onset of vesicles 800mg 5x day for 7 days (No effect if later) Case 1 • An 82 year old woman with no previous history of eye problems presents with an acutely painful, red left eye. The pain radiates to her forehead. On examination you also find that she has an unresponsive, mid dilated pupil (amaurotic pupil) and her vision is reduced to Snellen 6/60 in the left eye. The cornea is slightly cloudy. She is known to be long sighted. Case 2 • A 25 year old man comes to see you with painful and red eyes. He also has photophobia and there is a watery discharge from both eyes. On further questioning it appears that these symptoms started in his left eye eight days ago and spread to his right eye in the last two days. He does not report any loss of vision. He has palpable, rubbery, preauricular lymphadenopathy. His three year old daughter also had a red eye about two weeks ago, but she has now recovered. Case 3 • A 78 year old woman presents at your surgery with a three day history of a rash on the right side of her forehead. The rash is painful. Her right eye is slightly red and photophobic. Her pupils are reactive and her visual acuity is normal. On staining with fluorescein dye her eyes show no corneal epithelial lesions. Case 4 • A 28 year old man presents with an acutely painful eye. He has not had any eye problems before and does not wear contact lenses. On further questioning he tells you that he occasionally gets cold sores. Examination reveals central corneal staining. Case 5 • A 78 year old man presents with a painful eye. On further questioning he says he has a mild reduction in vision and photophobia. His past ocular history includes a previous history of rheumatoid arthritis. Case 6 • A 40 year old man presents with a severely painful and red left eye for five days. He wears a contact lens. His vision has decreased to perception of light only. The patient confirms that cleaning contact lens solution has always been used up to this date. There is purulent discharge. Case 7 • A 48 year old man presents with a three week history of double vision, a gritty, red right eye. He says the eye feels protruding and enlarged. His vision is normal and he is otherwise well.