Ophthalmology - York General Practice VTS
advertisement
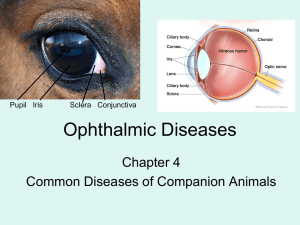
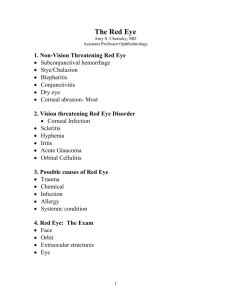
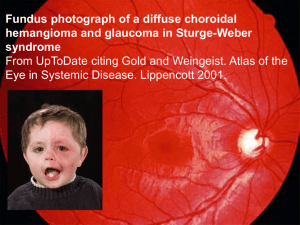
OPHTHALMOLOGY: THE RED EYE Barbara Adams Shyni Nair Aims Know how to manage the red eye in general practice Know what, when and how to refer to secondary care Know what happens in the eye clinic The Red Eye: taking a history Questions to ask: One eye or both Time and speed of onset Pain, itchy or gritty, photophobia, VA- blurred/double vision etc, discharge, headaches, nausea, rashes ? Trauma Contact lens wearer Associated URTI Any other family members affected Any treatment The Red Eye: taking a history (2) Past ocular history: similar episodes, wears glasses, recent eye test, any eye surgery, lazy eye, contact lens wear- ? Do they leave in at night/forget to clean lenses Social history: ? Contact with children with sticky eye, e.g. Nursery. Elderly patient- ? Able to manage eye drops at home Examining the Red Eye: useful tips ? Visual acuity affected- use pinhole when assessing VA to remove refractive error Ophthalmoscope is a good magnifier for looking at eye surface – adjust diopter If taking a swab – don’t use fluorescein first (chlamydia test relies on fluorescence) Examining the Red Eye (2) Look at pattern of redness Pupil- ? Reactive, shape Cornea bright or cloudy Look for foreign body Magnifier- have good look at cornea, ? lumps on palpebral conjunctiva Evert lid if FB suspected (wipe) Feel for pre auricular lymph nodes Fluorescein stain- shows any corneal injury (e.g. abrasion, FB, herpes) all unilateral If using local anaesthetic ? pain relieved Causes of red eye Infection Trauma Allergy Chemicals Systemic illness Classification of Red Eye Vision threatening corneal infections; Scleritis; Hyphaema; Iritis/uveitis; Acute Glaucoma; orbital cellulitis Non vision threatening subconjuctival haemmorhage; Hordeolum; Chalazion; Blepharitis; Conjunctivitis; Dry Eyes; Corneal abrasions Symptoms associated with red eye (1) Itching = allergy Scratchy / burning = anything on front of the eye e.g. eyelids, conjunctiva, FB Localised eyelid tenderness = Chalazion Deep intense pain = usually serious Corneal abrasions (exception) scleritis Iritis/uveitis acute glaucoma (+vomiting) non eye related e.g. sinusitis Symptoms associated with red eye (2) Photophobia = anything that damages surface of the eye Corneal abrasions Uveitis/Iritis Acute Glaucoma (haloes around lights) Conjunctivitis Can be viral, bacterial, allergic, chlamydial Gritty or itchy discomfort. If moderate to severe pain, suspect more serious pathology Photophobia rare (and VA usually normal) unless severe form of adenoviral infection which may involve the cornea Can be unilateral or bilateral Discharge in infective conjunctivitis, follicles or papillae May be eyelid swelling Viral conjunctivitis Watery Unilateral then bilateral Often with URTI and pre auricular nodes May be trivial or severe May need referral if painful May last weeks Sometimes epidemic Viral is highly contagious and can cause keratitis (photophobia & haloes) refer Bacterial conjunctivitis Usually bilateral Sticky in am Not usually painful Self limiting, lasts days Treat with chloramphenicol or fucidin in children In neonates- swab & refer (used to be notifiable disease). Slightly sticky vs. full blown conjunctivitis. Allergic conjunctivitis Itchy Seasonal or perennial Hayfever Chronic severe types may need steroids esp in children/teenagers Sensitised to drops or preservatives Corneal causes of red eye Abrasion Trauma: e.g foreign body, more serious- blunt trauma, e.g champagne cork- need to refer urgently as risk of retinal detachment, orbital fracture, raised IOP and visuaL loss. May need urgent surgery Corneal ulcer: contact lenses, herpetic Other rare causes: Look for cloudy cornea; any corneal cause needs slit lamp examination to confirm Herpetic Herpes simplex usually corneal except as primary infection and commonly recurrent Herpes Zoster causes immune mediated intraocular inflammation any time from two weeks after the initial infection - signs of uveitis - corneal denervation - raised intraocular pressure (IOP) common Chemical injury Ocular emergency Alkali worse than acid Irrigate (anything you can drink is suitable) but water is preferable, as much as possible. LA prior Send up to Eye clinic same day Dry eyes Caused by disturbance in the tear film. It may be the result of deficient aqueous production (eg, Sjogren syndrome, lacrimal gland dysfunction/obstruction) or increased evaporation (eg, contact lens use, allergies, Meibomian gland dysfunction, low blink rate) Females Autoimmune association (RA, Sjogren’s) Burning, FB sensation, reflex tearing (confuses patients) Rx artificial tears and lubricating ointment for nighttime Schirmer test uses filter paper to wick up tears and measure the amount of production, as shown in a patient with Sjogren syndrome Blepharitis: symptoms Itching Burning Mild pain FB sensation Tearing or dry eyes Crusting Recurrent and variable Blepharitis: causes V common, no cure, aim is to manage symptoms Anterior (eyelashes) & Posterior (meibomian glands) Anterior: crusting of eyelid margin Posterior: inflammation of meibomian glands, usually more symptomatic (itching/irritation/FB sensation) Often assoc with systemic disease, e.g. rosacea or seborrhoeic dermatitis Treatment: lid hygiene, lubricant eye drops, systemic antibiotics for refractory cases. (e.g. doxycycline- 100mg od 1m then 50mg od 2m) Styes and chalazions A stye (hordeolum) is an acute, localised abscess of the eyelid caused by staphylococcal infection Two types External stye (external hordeolum or common stye): edge of eyelid. Caused by infection of eyelash follicle or gland (sebaceous- Zeiss or apocrine- Moll) Internal stye (internal hordeolum or meibomian stye) occurs on conjunctival surface of the eyelid and caused by infection of a meibomian gland (within tarsal plate) Styes and Chalazions (2) Chalazions are lipogranulomas of either a meibomian or Zeiss gland. Lipid breakdown products leak into surrounding tissues from either bacterial enzymes or retained sebaceous secretions and cause a granulomatous inflammatory reaction. They are non tender nodules deep within the lid or tarsal plate Treated conservatively with lid massage and moist heat to express secretions Surgical incision and curettage performed for large symptomatic chalazions (need exceptions panel) ? Biopsy for recurrent lesions to r/o sebaceous cell carcinoma Uveitis Usually unilateral or asymmetric Painful (worse on accomodation), unrelieved by local Circumcorneal injection Recurrent May be systemic associations HLA B27, sarcoid etc Needs secondary care referral Only indication in primary care for steroids before slit lamp exam- if recurrent (usually have ROC card and have direct access to eye clinic) Episcleritis Sectorial or diffuse Usually asymptomatic other than redness Self limiting Scleritis Immune mediated- complex deposition Needs systemic investigation and treatment Painful and usually bilateral Try NSAIDs, then steroids, then others Subconjunctival haemorrhage May be spontaneous or traumatic, e.g. Prolonged coughing, childbirth Blood under conjunctiva, normal VA Refer if traumatic, otherwise check BP in elderly patients (hypertension) Reassure, resolves within few weeks Acute glaucoma Age 60-80s, in wwinter Degree of pain Fixed pupil, mid dilated Variable injection Before treating any red eye: Exclude foreign body Exclude corneal problem Exclude uveitis, scleritis, acute glaucoma History, degree of pain, lack of discharge, laterality, examination NO OTHER PROBLEM WOULD SUFFER FROM A COURSE OF ANTIBIOTIC DROPS