eye cases how
advertisement
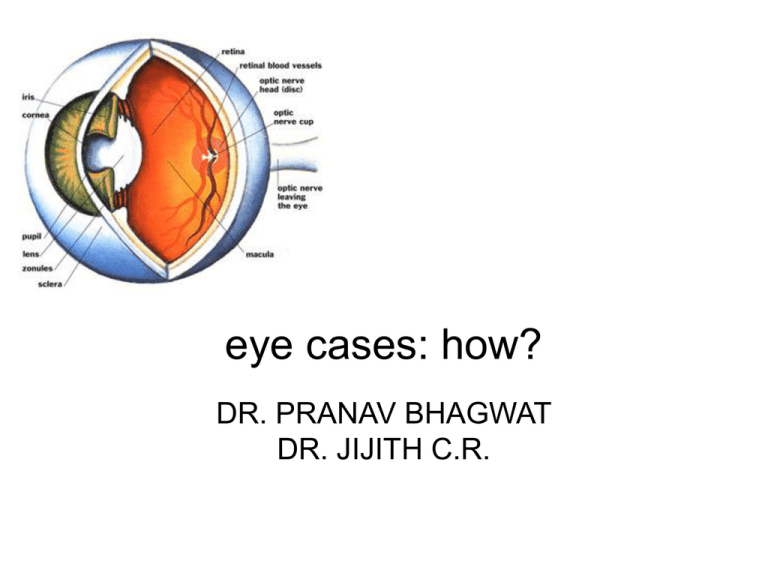
eye cases: how? DR. PRANAV BHAGWAT DR. JIJITH C.R. HISTORY TAKING – Allow patient to tell story. Decreased vision Ask for • • • • • • Onset Duration Uni / Bilateral Distant or near vision Whether the patient wears glasses Diurnal variation Sudden unilateral loss of vision • • • • • • • • Acute congestive glaucoma Acute optic neuritis Acute iridocyclitis Retinal detachment Central retinal artery occlusion Spasm of retinal artery Vitreous haemorrhage Injuries Sudden bilateral loss of vision • Acute methanol toxicity • Hysteria Reduced vision in the morning, improved in afternoon • Intermittent corneal edema Gradual onset loss of vision • • • • Cataract Refractory errors Retinopathy-DM, HT Retinal degenerations and RP • Chronic iridocyclitis • Chronic simple glaucoma • • • • • • Keratitis K opacities Chorio retinitis Chronic optic neuritis MS Drug toxicity Pain in the eye • • • • • Type Onset Duration Diurnal variation Associated complaints e.g., nausea, vomiting, DV Severe eye pain • • • • • • • Adhimantha K abrasions and ulcers Acute iridocyclitis Panopthalmitis Acute glaucoma Scleritis Episcleritis Dull Aching pain • Cases with eye strain Mild eye pain • Corneal FB • Conjunctival FB • Conjunctivitis Pain around the eye • Pathology of the lid and lacrimal apparatus (eg: stye) Redness of the eye Normal eye lid with normal corrected visual acuity • • • • • Conjunctivitis Keratitis Corneal ulcer Arjuna Episcleritis Abnormal eye lid with normal corrected visual acuity • • • • Ectropion Entropion Stye Blepharitis Reduced corrected visual acuity without diplopia • • • • Iritis ACG K foreign body K ulcer Reduced corrected visual acuity with diplopia • Carvernos sinus thrombosis • Orbital cellulitis • Caratico carvernos fistula Common causes –red eye. Photophobia • Acute infective or inflammatory lesion of the anterior segment • Recently operated eyes Watering of the eyes 1)Excessive lacrimation • Keratitis • Uveitis • Glaucoma 2) Epiphora • Mechanical obstruction to drainage- stricture, punctal stenosis & chronic dacryocistitis • Defective orbicularis action Discharge • • • • Watery-Mild bacterial infection Serous -viral Mucoid -mild conjunctivitis Mucopurulent & purulent- acute pyogenic infection of anterior segment • Serosanguinous- opthalmia neonatrum Itching • • • • Allergic disoders- phlycten Episcleritis Spring catarrh Allergic blepharo conjunctivitis Netra daaha • Pittotklishta • Pittaja abhishyanda • Pitta vidagdha drishti. Foreign body sensation • • • • Presence of FB Distorted eye lashes- trichiasis, entropion Conjunctival concretion, calcification Contact lenses Black spots in front of eyes • 1) Stationary K scars, lens opacity • 2) Mobile- Vitreous opacities Headache • Refractive errors • Improperly corrected refractive errors • Zoster Haloes around light • 1) Early ACG • 2) Acute mucopurulent conjunctivitis • 3) Early stages of cataract Photopsiae • Irritative lesions of retina • Impending RD Diplopia • 1) Unioccular- high K astigmatism, subluxated or dislocated lens • 2) Binocular- Squint Nyctalopia • • • • Vitamin A deficiency Retinitis pigmentosa Pathological myopia Glaucoma Occupation • Welders • Black smiths- foreign body in the eye • Farmers- fungal keratitis Medication • 1) Gentamicin, miotics, Atropin- follicular response • 2) Topical anasthetics for long timesevere corneal reactions • 3) Topical and systemic steroids- K disease, cataract, glaucoma • 4) Thiomersal- allergic conjunctivitis, epithelial Keratitis • 5) Benzalkonium- toxic papillary reaction Past history • Systemic diseases- diabetis mellitus • Arjuna-HT • Iritis- ankylosing spondylitis History of previous ocular disease • Childhood squint- lazy eye • Blunt injury- traumatic mydriasis ( could be confused with partial third nerve palsy) Family history • Chronic glaucoma- the incidence nearly 5 times greater in siblings and children of affected patients Examination of the function of eye Visual acuity • • • • • • • Snellen’s chart- 6 mtrs Wear his distant corretion One eye at a time 6/60 - 6/6 CF at 1 meter Hand movements PLPR • Jaeger’s test type • N5 to N48 Visual field • 1) Peripheral field- confrontation or perimeter • 2) Central field by scotometery Colour vision • Ishiahara chart Ocular and periocular examination • 1) Head postureParalytic squint. Face • • • • Look for Asymmetry Signs of paralysis Obvious skin changes Orbit • Inspection and palpation Eye brows • Look for loss of hair- lepromatous leprosy, myxoedema • Depigmentation Eye lid • 1) Position of the lid margin in relation to cornea- drooping of lids • • 2) Thickness of the lid 3) Swelling a) b) Localised eg) Stye, chalazion GeneralisedOedema,ecchymosis Pakshma mandal • • • • Trichiasis- misdirection of lashes Distichiasis- double row Madarosis- scantiness Matting- conjunctivitis Shuklamandal (conjunctiva & sclera) • 1) Bulbar conjunctiva a) congestion- ciliary/conjunctival b) Chemosisc) Subconjunctival haemorrhage d) Pigmentation e) Nodule Upper tarsal conjunctiva • Congestion • Alteration of normal vertical vascular pattern • Follicle/papilla • • • • Scarring Membrane formation Granuloma Foreign body Lower tarsal conjunctiva • As above + any sign of symblepheron Staining • 2% fluorescein- raw area- green • 1% rose bengal- conjunctiva- pinkish red Sclera • Colour change • Pigmentation • Protrusion of uveal tissue • Congestion • Nodule formation Krishnamndal (cornea & iris) • Cornea • 1) Size- normal (12 to 13 mm) • 2) Curvature-conical / globular / flat • Surface- examine by window reflex / placido disc / slit lamp • Irregular surface- corneal ulcer, scarring • Depression / corneal facets • Elevation- epithelial bulla • • • • Opacity 1) density- nebula / macula / leucoma 2) Situation and extent in relation to pupil 3) Iris adhesion • Pannus (sirashuklam)• Keratic precipitates • Corneal sensations Diminished sensation• Herpes • 5th nerve paralysis • ACG and absolute glaucoma • Leprosy • Prolonged use of contact lens • Post surgery • Local anaesthesia • Corneal stains Iris • • • • 1) Iris pattern 2) Colour 3) Vessels- visible = patho. 4) Atropic patches = end stage of glaucoma Defect in the iris • Iridodonesis- aphakia / buphthalmos • Iridodyalisis • Anterior synechia • Anterior chamber Depth and content Pupil • • • • • • Size- (3 to 4mm) Shape Position Pupillary margin Pupillary aperture Pupil reaction Lens • Colour • Opacity • Position Pakshmavarthmagathasanthi • • • • Entropion Ectropion Tylosis Milphosis Kaneenika sandhi • Lacrimal puncta- eversion / stenosis / absence • Skin around it Shuklakrishnagatha santhi • Nodule • Congestion tonopen Tonometry Shiotz tonometer. Fundoscopy Ocular coherence tomography • Thank you!