Shuan Dai - The Goodfellow Symposium 2012
advertisement

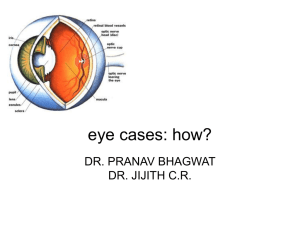
How to Handle Common Eye Problems in Your Practice Shuan Dai, FRANZCO Eye Doctors Ascot Hospital shuandai@eyedoctors.co.nz The Red Eye • A “Red Eye” may be due to an abnormality of the ocular structures including: • Adnexa • Lid Disorders • Lacrimal System • Orbital Disease • Globe • • • • Conjunctival / Scleral Disorders Corneal Disease Uveitis Glaucoma Adnexal Redness • Lids • • • • Blepharitis Stye Chalazion Topical Allergic • Lacrimal System • Dacryocystitis • Canaliculitis • Dacryoadenitis • Orbit • Cellulitis • Preseptal • Orbital Blepharitis • Symptoms & signs • Crusting • Oil droplets • Grittiness • Treatment • Lid hygiene • Doxycycline 100mg daily 4-6 weeks Stye & Chalazion Dacryocystitis • Recurrent watering eye • Mucous/purulent discharge • Abscess /lump over lacrimal sac • Blocked tear duct Ophthalmia Neonatorum • Infantile purulent conjunctivitis • Chemical from antibiotic drops/silver nitrate • Chlamydia • Gonorrhea • An ocular emergency as GC can invade the intact cornea and perforate the globe Lacrimal sac mucocele • An uncommon variant • Look for an elevated mass extending medially • Life threatening if infected – refer for intravenous antibiotics Dacryoadenitis • Acute painful • Swelling lateral upper lid • Viral/bacteria infection • Oral/iv antibiotics Orbital Cellulitis • Proptosis • Limited eye movement • Reduced vision Redness Confined to the Globe • Conjunctiva / Sclera • Subconjunctival hemorrhage • Ocular injection – conjunctivitis • Pingueculum / Pterygium • Episcleritis • Scleritis • Cornea • Keratitis • Corneal abrasion • Corneal ulcer • Anterior chamber • Iritis • Endophthalmitis Conjunctivitis • Bacterial • Purulent discharge • Papillary reaction • Associated blepharitis • Viral • Mucoid discharge • Follicular reaction • Associated URTI, epidemic • Allergic • Seasonal • Papillary reaction • Associated rhinitis, itching Bacterial Conjunctivitis • Symptoms: discharge, irritation • Signs: papillary conjunctivitis, perilimbal injection if associated keratitis • Treatment: chloramphenicol/fucithalmic • Danger: if hyperpurulent (gonococcal) or recent intraocular surgery REFER! Viral Conjunctivitis • • • • • Highly contagious, epidemics Symptoms: previous URTI, previous contacts, mucoid discharge, often photophobia Signs: preauricular node, pseudoptosis, follicular conjunctivitis ,conjunctival injection, punctate keratitis Treatment: cool compresses, ocular lubricants. Referal Warning: extreme infectivity, second eye at one week, lasts 10 – 14 days Allergy -Papillary conjunctival reaction Allergic Conjunctivitis • Symptoms: itching, seasonal, atopic history, rhinitis • Signs: papillary reaction, mucus • Treatment: cool compresses, ocular lubricants, anti-histamines topical (Vasocon A) or systemic, Opticrom (Na chromoglycate) prophylaxis • Possible history of contact lens wear with giant papillary conjunctivitis • Treatment: • Lomide • Patanol • Steroid, i.e. FML Pingueculum & Pterygium Pingueculum is degenerative collagen within the interpalbebral fissure Pterygium extends onto the cornea Episcleritis & Scleritis Episcleritis Diffuse Scleritis Less painful Extremely painful Younger age Elderly, No systemic association RA, systemic vasculitis Herpes Simplex Keratitis • Viral replication in cornea • Symptoms: irritation, photophobia • Signs: • • • • red eye involving limbus, dendrite with terminal bulbs seen best with staining ulcer formation • Treatment: refer, antivirals, BEWARE STEROIDS! Herpes Zoster • Herpes Zoster Ophthalmicus • Suspect ocular involvement if the tip of the nose is involved (Hutchinson’s sign) • Oral acyclovir & topical acyclovir Iritis • Etiology • 50% idiopathic, unknown • Ocular disease • Large abrasion • HSV, HZV • Primary disease in young patients • Systemic disease • JRA – pauciarticular disease • Ankylosing spondylitis • Symptoms • Extreme photophobia • Reduced vision • Signs • Miosis • Red eye to limbus • Flare with cell • Treatment • Cycloplegia • Topical steroids REFER Acute iritis • Light sensitivity • Deep dull ache • Smaller/ irregular pupil • Often idiopathic Angle Closure Glaucoma Subconjunctival Hemorrhage • Can occur secondary to blunt trauma or can be spontaneous • Lubrication if foreign body sensation • Warm compression Corneal Abrasion • Management • Non-contact lens wearer • Antibiotic ointment and patch • Follow-up one day • Contact lens wearer • DO NOT PATCH • Antibiotic ointment or drops • Follow up daily until healed • Treat abrasions created with organic material in this manner Corneal Ulcer • Risk of corneal ulcer when epithelium compromised, especially in contact lens wearers • Contact lens wearers have a higher rate of colonization with Pseudomonas Abrasion versus Ulcer Abrasion Ulcer Stain Stain Transparency Transparent Opaque Corneal contour Unchanged Uneven Epithelial only Involves stroma Fluorescein Level Superficial Corneal Foreign Body • Removed under topical anesthetic • With burr or 25 gauge needle • Manage same as corneal erosion • Encourage safety glasses • Polycarbonate lenses Anterior Segment • Linear epithelial defects is suggestive of a foreign body under the eye lid Ultraviolet Radiation(arc eye) • Sources • Sunlamps, welding arcs • Management • Cycloplegics, antibiotic ointment, patch • Avoid long term topical anaethetic drop !!! Chemical Injury • Acid precipitates quickly • Alkali continues to penetrate • Therefore can progress over an extended period of time • Management • Continuous irrigation with saline until neutral pH • Test fornices with Litmus paper • Sweep fornices to remove retain debris • Antibiotic ointment, cycloplegics Chemical Injury Thorough irrigation before referral !!! Blunt Trauma • Hyphema • Indicates damage to angle and/or to the iris • Management • Vertical position • No anti-coagulants • Cycloplegics Blunt Trauma • Damage to Iris and Lens • Iridodialysis, cataract • Dislocation Blunt Trauma - Sequelae • Angle damage which can lead to glaucoma: can develop days to years after injury Blunt Trauma - Sequelae • A retinal tear which can progress to a retinal detachment Open Globe Injuries • Blunt trauma – rupture • Sharp trauma – laceration • Projectile trauma • Penetrating – in and out • Perforating ± intra ocular foreign body – just in Blunt Trauma • Severe trauma that resulted in a scleral rupture with delivery of the lens Sharp Trauma • Corneal laceration and traumatic cataract from a thrown beer bottle Penetrating Eye Injuries • Intraocular foreign bodies generally have to be removed, unlike orbital (extraocular) foreign bodies Perforating Trauma • Patient was hammering and noticed a spark fly up to his eye. Child with poor red reflex