Benign_biliary_disease_for_med_students
advertisement
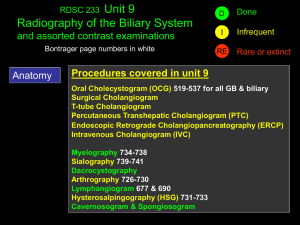
Benign biliary disease Dr. Gili Halfteck Department of General Surgury Shaare Zedek Medical Center January 2014 Anatomy Calot’s triangle Physiology • Roles of bile secretion: 1. Excretion of toxins and cellular metabolites (bilirubin) 2. Lipids absorption Components of bile: 1. Bile salts 2. Lipids (phospholipids and cholesterol) 3. proteins 4. pigments Bile flow Stimuli of bile secretion 1. Vagal activity 2. Secretin 3. CCK (bile secretion and gallbladder wall contraction) • Fasting state: - entero-hepatic circulation - Accumulation of bile in the gallbladder - Retrograde filling of the gallbladder - tonic activity of the sphincter of Oddi • Fed state: - CCK (acid, fat and protein in duodenum) - Vagal activity Symptoms of biliary tree disease • Pain • Fever • Juandice Pain • • • • Biliary colic Usually constant pain Location: RUQ/epigatrium Can be associated with meals (1 hour or more after a meal) • Caused by contraction of the gallbladder against an obstructed neck • Stasis + pressure + bacterial inoculum – infection and inflammation (RUQ tenderness on palpation) • Murphy’s sign Fever • Accompanies infection and inflammation of the gallbladder or biliary tree • Not present in biliary colic Juandice • • • • • Elevation of serum bilirubin Surgical (obstruction) / medical (hepatocellular) >2.5 mg/dl – scleral icterus >5 mg/dl – cutaneous juandice Pathogenesis: failure to excrete bile from the liver to the intestine • Charcot’s triade: fever, RUQ pain, juandice • Reynold’s pentad: + hypotension and altered mental status Laboratory tests • Bilirubin (conjugated/unconjugated) • Alkaline phosphatase, GGT • Serum transaminases (AST, ALT) Imaging 1. US • study of choice for initial evaluation of jaundice and gallbladder or biliary disease • Surgical/medical jaundice • High sensitivity and specificity for gallstones 2. HIDA (hepatic iminodiacetic acid) scan • Nuclear medicine test – demonstrated physiologic bile flow but does not provide anatomic delineation • Failure to fill the gallbladder 2 hours after injection – cystic duct obstruction (cholecystitis) • Obstruction of the biliary tree, bile leaks 3. CT scan • Superior anatomic information • Most gallstones are isodense to bile • Identifies cause and site of biliary obstruction • Preoperative planning in pancreatic/hepatic neoplastic processes 4. MRI/MRCP • Superior anatomic definition of intra- and extrahepatic biliary tree and pancreas • Non-invasive • No radiation exposure 5. ERCP (endoscopic retrograde cholangiopancreatography) • Invasive test using endoscopy and fluoroscopy • Contrast injection through the ampulla and imaging of the biliary tree • Able to diagnose and treat many biliary tree diseases (choledocholithiasis, tissue sampleing, CBD stenting) • Complication rate - 10% Bacteriology • Without previous biliary intervention bile is considered sterile • The presence of gallstones or obstruction and stasis increases the likelihood of bacterial contamination • Mostly gram-negative aerobes – passage of bacteria upward from the duodenum into the biliary tree • E. Coli, Klebsiella, Enterobacter, Enterococcus spp. Gallstones Types: 1. Mixed stones (70%) – cholesterol and calcium 2. Pure cholesterol stones (10%) 3. Pigment stones – brown/black (10%) Gallstones formation: - Supersaturation of bile - Concentration of bile in the gallbladder - Crystal nucleation - Gallbladder dysmotility Natural history of gallstones • Vast majority are asymptomatic – incidentale finding • Biliary colic – temporary obstruction of the cystic duct or gallbladder neck • 1% of patients with asymptomatic stones develop complications before onset of symptoms - prophylactic cholecystectomy is not warranted • High risk patients: - Hemolytic anemias - Porcelain gallbladder - Large (>2.5 cm) stones - Long common channels of bile and pancreatic duct - Bariatric surgery (sleeve, bypass) - Immunocompromised patients Non-operative treatment of cholelitiasis • Generally unsuccessfull and rarely used!!! - Oral dissolution - Contact dissolution - Shock-wave lithotripsy • Up to 50% recurrence rate Acute calculus cholecystitis • • • • • • Pathogenesis: unresolved cystic duct obstruction Inflammation, edema, subserosal hemmorhage Infection of stagnant bile pool Can progress to ischemia and necrosis (gangrenous cholecystitis) Presentation: Fever RUQ pain Tenderness to palpation Laboratory finding: leukocytosis, mild elevation of bilirubin, transaminases, alk-phos. diagnosis 1. Transabdominal US - sensitive, inexpensive and reliable - Sensitivity – 85%, specificity – 95% - Gallstones, gallbladder wall thickening, pericholic fluid, sonographic murphy’s sign 2. Hida scan - Atypical cases - Cystic duct obstruction 3. CT scan - Less sensitive then US Treatment • NPO • IV fluids • IV antibiotics (broad-spectrum) • Pain control • Cholecystectomy (open/lap.) • Percutaneous cholecystostomy Chronic cholecystitis • Inflammation and scarring of the gallbladder neck and cystic duct • Pathogenesis: recurrent biliary colic which cause temporary cystic obstruction and do not cause acute cholecystitis • Presentation: recurrent biliary colic (usually after fatty meals), nausea, vomiting • RUQ/epigatric pain radiating to the scapula, usually resolves within few hours • Symptomatic cholelithiasis – indication for chlecystectomy Diagnosis • History • Transabdominal US – stones, sludge Treatment • Elective cholecystectomy • Curative in > 90% of patients choledocholithiasis 1. Primary common duct stones - De novo in the bile duct - Usually brown pigment stones - More common in Asian population - Associated with bacterial bile duct infection 2. Secondary common duct stones - Arising from the gallbladder - Most common bile duct stones in the USA • Retained common duct stones – found within 2 years of cholecystectomy Presentation • 80-90% of common duct stones remain clinically silent • Routine cholangiography – 10% choledocholithiasis • Selective cholangiography (pain, abnormal liver function test) – 1-2% of patients will present with retained stones • - Symptoms: Biliary colic Obstructive juandice Ascending cholangitis (fever, pain, juandice) Diagnosis • • • • Hepatic function panel abnormalities Leukocytosis US – choledocholithiasis, biliary ductal dilatation, gallstones Bile duct dilatation (>8 mm) in the presence of biliary colic, juandice or gall stones is suggestve of choledocholithiasis • ERCP - highly sensitive and specific - Usually therapeutic - Sphincterotomy, balloon stone extraction - Complication rate – 5-8% • MRCP - highly sensitive and specific - Does not provide therapeutic solution treatment 1. ERCP - Sphincterotomy and stone extraction - Reasons for endoscopic failure: large stones, multiple stones, intrahepatic stones, altered anatomy, duodenal diverticula, impacted stones - Does not eliminate the risk of recurrent biliary stone disease (up to 50% recurrence) 2. Common bile duct exploration (lap./open) - Intraoperative cholangiogram - Trans-cystic/common duct incision Ascending cholangitis • Acute ascending bacterial infection of the biliary tree cause by obstruction • Obstruction: stones, malignancy • Presentation: Charcot’s triad (fever, RUQ pain, jaundice), Reynold’s pentad (+hypotension, altered mental status) Diagnosis • Tachycardia, shock symptoms • Laboratory test: leukocytosis, abnormal liver panel • US – dilatation of the biliary tree • CT – site of obstruction • ERCP/PTC – diagnostic as well as therapeutic Treatment • • • • NPO IV fluids IV antibiotics Most patients respond to medical therapy • Emergent decompression of the biliary tree (ERCP/PTC) Questions?