Clostridium difficile: Epidemiology, management
advertisement
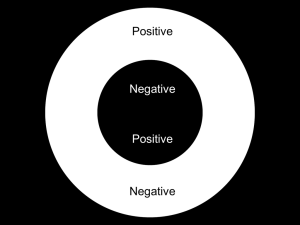
Jayesh Patel, MD, DTM&H Infectious Disease Consultant Chair Infection Prevention and Pharmacy/Therapeutics/Nutrition (Skyline) No financial conflict of interest ( Past speaker for Dificid) Learn current epidemiology of C. difficile infection Understand clinical presentation of C. difficile disease Understand testing methodology for C. difficile infection Learn about prevention and treatment of C. difficile infection Learn about rationale and methods of treatment by fecal microbiota transplantation Gram positive anaerobic bacillus Produces spores Commensal intestinal flora in 2-5 % of healthy adults, over 50% of infants Fecal-oral transmission Colonizes 20-40 % hospitalized patients Produces toxins A, B, and Binary toxin NAP1/BI/027strain of C. difficile "North American Pulse-field type 1" pattern (on gel electrophoresis) and a "BI" pattern (on restriction endonuclease analysis), and type "027" (on ribotyping) Resistance to quinolone antibiotics Hypersporulation Binary toxin production High levels of toxin A,B (20 x greater) High morbidity and mortality USA 15,000 – 20,000 deaths annually, rising 20 % of all episodes of antibiotic associated diarrhea are due to C. difficile 4-10 cases per 10,000 patient days Relapse occurs in over 20 % of cases Increase in average hospital cost : $ 27,000 Over 1 billion dollars in costs annually Current and prior antibiotics Elderly Immunocompromized Hospital stay, nursing home residence NG tube, tube feeding Recent Endoscopy, Gastrointestinal surgery Proton pump inhibitors, H2 blockers, Chemotherapy Private rooms Contact isolation: gloves, gowns Hand washing ( instead of alcohol based ) Special entry signs EPA approved sporicidal agents, diluted bleach for cleansing all environmental surfaces and reusable devices Isolation till diarrhea resolved or discharged Diarrhea, abdominal pain, N/V, fever, loss of appetite Pseudomembranous colitis Toxic megacolon Perforation of colon Severe sepsis Death ? Smell WBC , creatinine, albumin Stool testing Culture for C. difficile — — — — slow labor intensive, technical expertise expensive requires second test for toxin detection Cell Cyto-toxicity Neutralization Assay — Toxin B detection only — Slow, Labor Intensive/technical expertise — Moderate sensitive, High specificity Antigen detection ( Glutamate DeHydrogenase EIA) — — — — Highly Sensitive Rapid Cheaper Not specific Toxin Enzyme Immuno Assay — Detects toxin A and B — Quick, inexpensive — Less sensitive — Toxin is heat labile so testing must be done within 2 hours or keep stool sample refrigerated PCR — Toxin B gene — Very sensitive and specific — Rapid if done in house — Expensive Antigen negative: no further testing, not C. difficile Antigen positive, Toxin positive: has C. difficile Antigen positive, Toxin negative: send for PCR — PCR negative: not C. difficile — PCR positive: has C. difficile Indication: mild to moderate CDI Administration: 500 mg PO or IV tid for 1014 days First line therapy for mild to moderate CDI, but increasing rates of refractory infection are being observed Indication: Moderate to severe CDI Administration: ~125-500 mg PO qid for 1014 d Oral, nasogastric, or rectal therapy may be combined with IV metronidazole in critically ill patients. Tapered/Pulse therapy for recurrent CDI Indication: index infection or recurrent CDI Administration: 500 mg PO bid for 10 days More studies are needed to clarify its role in CDI. Indication: recurrent CDI Administration: 200 mg PO bid to 400 mg PO tid for 28 d. May be given as a “chaser” after completion of vancomycin therapy for recurrent CDI. More controlled studies needed to decide best use of this drug. Indication: index infection of recurrent CDI Administration: 200 mg PO bid for 10 d Non-inferior to vancomycin and is associated with a significantly lower rate of recurrent infection Expensive Indication: symptomatic adjunct to antibiotic treatment Administration: Cholestyramine 4 g PO tid or qid. ?? Duration Toxin binders such as cholestyramine should be used to control symptomatic diarrhea but not as the only treatment. Indication: refractory CDI Administration: IV infusion at a dose of 400 mg/kg (IVIG) of body weight given with antibiotic therapy. Enhances overall efficacy of treatment and reduces further recurrences. Expensive Indication: prevention of recurrent CDI Administration: 500 mg PO bid for 28 d. Usually started after 7 days of antibiotic treatment. Avoid using in severely immunosuppressed patients; should not be given chronically. (Lactobacillus not proven to help) Bacitracin suspension Rifampin Teichoplanin Tigecycline Surgery: Colectomy Fecal bacteriotherapy/FMT Indication: recurrent/refractory CDI; unclear role in severely ill CDI patients as first-line therapy. Administration: stool suspension from a healthy donor administered by nasogastric/NJ tube, via colonoscopy or enema. Excellent preliminary results in patients with severe and refractory disease. Best methodology is yet to be clarified. 62 yr old white male Had URI ( ? Viral), got abx. and 3 days later, develops diarrhea, becomes severe, Metronidazol started. Gets worse, abd cramping, weakness, mucousy stools, stools every ½ hour. PMH: splenectomy, multiple sinus surgeries, fracture/laceration finger one month earlier, had pinning and got prophylactic antibiotic. Admitted to Hospital WBC 12.9k, Cr 1.2, C. diff Ag/Toxin positive Oral vancomycin started Slow/poor response, Nitozoxanide added Slow improvement, discharged on oral Nitozoxanide. Nitozoxanide not covered by insurance so changed to Metronidazol. Had 1-2 soft/loose stools daily. 2 days after completing Metronidazol, develops explosive diarrhea 20 BM/day, nausea, chills, abdominal pain, weak Readmitted Ill looking, T 100.1, HR 110, BP 100/52 Abdomen tender Treatment: IV fluids, Vanco PO, Metronidazol, Nitozoxanide Poor response: ? Fidoxamicin ? FMT ?Colectomy Patient elects to have FBT/FMT Approx. 70 grams donor stool instilled via Naso-duodenal tube, partial response, 2nd instillation of fresh 100 gram stool next day. Diarrhea resolves 3rd day. Patient observed 2 more days than discharged home free of symptoms Patient free of symptoms after 6 months Diagnosis will be confirmed by Gastroenterologist or Infectious Disease Specialist. Gastroenterologist or Infectious Disease Specialist wishing to use(FBT) will notify designated departments to schedule the testing/procedure, and discuss the process with donor and recipient for Informed Consent. FBT/FMT Policy and Procedure Patient Consent Patient Education Brochure Donor Consent Donor Instruction Bowel Motion Record All recipients will have the following laboratory tests: — HIV antibody — Hepatitis A antibody — Hepatitis B surface antigen — Hepatitis C antibody Ideally the stool transplant donors should be related to the recipient but not the spouse, significant other or a family household member. They should be healthy and have not received antimicrobial therapy in the last 2 months. The donor should have normal bowel habits and be free of blood-borne or stool-borne pathogens. Screening tests prior to the transplant Acute Hepatitis Panel, HIV antibody, and CBC Donor stool testing for Clostridium difficile toxin, Stool culture , Cryptosporidium stain, Stool O & P Obtain signed consent for Fecal Bacteriotherapy/FMT Start Liquid diet the day prior to the scheduled FBT/FMT Cleanse patients’ bowel using 3-4 liters of Golytely, the day before FBT/FMT Give PPI agent day of procedure for upper GI administration Stop antibiotics 24-48hr before FMT Obtain 250-300 gms (approx one cup) of fresh stool from donor as soon as possible prior to the transplantation procedure, never more than 4 hours prior. Using a blender, add stool to 250ml of Normal Saline or Sterile Water. Mix until stool particles are dispersed throughout the liquid Remove large particles by straining the stool/liquid mixture twice, utilizing strainer. Mixture should be administered within 2 hours of preparation. No more than 6 hours should elapse between stool specimen collection and fecal administration. Administer as Enema or by Colonoscopy into terminal ileum and colon. Enema can be given by standard enema set or by Fecal Management System (ActiFlo). Retain enema for 1-2 hours. Repeat enema with fresh stool next day if ordered. On the day of the procedure, obtain 100 g (approx 1/3 to 1/2 cup) of donor stool. Using a blender, add stool to 100 ml (or necessary amount to facilitate installation) of Normal Saline or Sterile water. Mix until stool particles are dispersed throughout the solution. Remove large particles by straining the stool/saline mixture twice, utilizing a strainer. Transfer solution into catheter tip syringes for transport to patient. Place NG tube or Naso-duodenal tube morning of procedure in radiology department. If NJ tube is used, it is inserted into Jejunum through endoscope. Don gown, gloves, mask, and eye protection. Using a syringe administer the freshly mixed stool via NJ/ Dobhoff tube. After stool installation, flush with 50ml of normal saline. (DO NOT REMOVE NJ/DOBHOFF TUBE). Repeat stool infusion procedure next day. Do not remove NJ/Dobhoff tube until ordered by physician. Listen to your mother: Don’t forget to wash your hands after using the restroom and before eating!