Parasites for the Primary Care
Physician
Stephen J. Gluckman, M.D., F.A.C.P.
Case 1
A 22 year old woman see you for several weeks
of crampy abdominal pain and loose stools
– Travel: Philadelphia
– Diet: Unremarkable
– Medications: Triphasil for 3 years
– Physical Examination: Normal
– Stool Culture: negative x 1
– Stool for O and P: loaded with Iodamoeba
butschlii trophozoites and cysts
WHAT IS YOUR NEXT STEP?
Non-Pathogenic Protozoa
•
•
•
•
•
•
•
Entamoeba coli
Endolimax nana
Entamoeba gingivalis
Iodamoeba butschlii
Entamoeba dispar
?Dientamoeba fragilis
?Blastocystis hominis
Amoebiasis
• Treatment of amoeba in the stool
– Is it E. histolytica or a non-pathogen?
– Trophs: metronidazole
– Cysts: diloxanide, paromomycin, iodoquinol
Case 2
A 45 year old man has a history of 4 days of
watery diarrhea, abdominal cramps, bloating,
and flatulence. His 46 year old wife was
recently diagnosed with irritable bowel
syndrome. One of their two children has been
seeing a pediatrician because of failure to gain
weight. The other child is well.
Case 2 (cont)
• Travel: nothing remarkable other than
frequent trips to a vacation home in the
mountains
– Having been well trained you naturally think of
giardia. However you are told that the drinking
water comes from a public reservoir and is well
chlorinated.
NOW WHAT?
Giardiasis
• Epidemiology
– Cysts live in cold water for months
– Cysts are relatively resistant to chlorine
– Associated with decreased IgG and secretory IgA
• Clinical
– Asymptomatic
– Acute diarrhea
– Chronic malabsorption
• Treatment
– Metronidazole: 250 TID x 5-7 days
– paromomycin
Case 3
A student from the emergency room calls
you on August 6th about a patient he has
just evaluated for severe headache, fever,
rigors, and diffuse myalgias. Examination is
normal. WBC 4500 with normal
differential.
The student’s tentative diagnosis is “flu”
and has called to ask your advice about
treatment with amantidine v. oseltamivir.
YOUR RESPONSE?
“Flu” in the Summer
•
•
•
•
•
Rocky Mountain Spotted Fever
Ehrlichiosis
Anaplasmosis
Malaria
Babesiosis
Babesiosis (cont)
• Laboratory
– Anemia, leucopenia, thrombocytopenia
• Diagnosis
– Peripheral smear: looks like P. falciparum,
tetrads
– Serum antibody test
• Treatment
– Quinine/Clindamycin
– Atovaquone/Azithromycin
Case 4
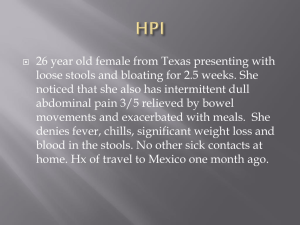
You are referred a 26 year old woman who has
had three episodes of trichomonas in the last 6
weeks. She is married and monogamous. They
both have been treated on each occasion. All
treatment was with metronidazole. The first
course was with 2 grams as a single dose. The
second was 250 mg TID for 7 days. The last was
250 mg TID for 21 days. On each occasion she
responded, but then the symptoms recurred
IS SOMEBODY CHEATING?
NOT NECESSARILY
Relapsing Trichomoniasis
• Is the diagnosis correct?
– Can not distinguish the etiology of vaginitis
without laboratory testing.
• Have ALL of the partners been treated?
– Need to explore this in a non-judgmental way
• Was the medication taken properly?
– Adherence is always an issue with metronidazole
• Resistance occurs
– Can culture and get MIC’s
Trichomonas (cont)
• Treating resistant strains
– High dose metronidazole
– Combine with intravaginal metronidazole
– Tinidazole
– Nonoxynol 9
Case 5
• A 12 year old Nicaraguan girl, who recently
immigrated to the U.S. was seen in a regional
health center because of malaise and loose
stools
• A stool smear revealed
NOW WHAT?
MAKE SURE YOU ARE USING AN
EXPERIENCED LABORATORY
Case 6
A 45 year old lawyer is generally healthy. He plays
racquetball four times a week and sweats heavily. He has
noticed some peri-anal discomfort, primarily itching, for
the last several weeks. He called his physician who
suggested that his discomfort was due to a combination of
irritation from sweating and general anxiety related to an
upcoming major trial. He prescribed Tucks and Ativan
which gave the patient partial relief from his symptoms.
The patient’s 8 year old daughter, who has previously slept
well is now getting up in the middle of the night. Her
school work is suffering. A 3 year old child, two older
children, and his wife are fine.
NOW WHAT?
• Epidemiology
– Widespread in the USA
– Widespread in the house
• Diagnosis
Scotch Tape Samples
1
2
3
% Positive
50
90
99
• Treatment: single dose of mebendazole
– Be cool. Do not make a project out of hygiene
– Treat the entire household
– Treat the entire household again in two weeks
Case 7
A 28 year old woman who grew up in Puerto Rico
but has been in this country for the past 8 years
has difficult to control SLE. She has required high
dose prednisone therapy for the past 4 months to
control her SLE. She is now admitted with fevers
and rigors. The only localizing symptom has been
watery diarrhea for the past 2 weeks.
•
•
•
•
•
Blood cultures: 2 sets growing E. coli
Chest x-ray: normal
Stool Culture: normal flora
Urine Culture: no growth
RUO and Pelvic ultrasound: negative
She responds to treatment, but returns three weeks
later with the same symptoms. This time her
blood grows klebsiella.
WHAT IS GOING ON HERE?
Strongyloidiasis
• If there is one intestinal nematode to learn
about this is it?
– Autoinfection
• Chronic infection
• Hyperinfection syndrome
– Occurs in persons with defects in CMI
• Recurrent gram negative bacteremia
Strongyloidiasis
• Diagnosis
– Larva in stool, duodenal aspirate, or sputum
– May take many stool specimens
• Treatment
– Ivermectin
• Confirm cure
• Consider asymptomatic infection before beginning
immunosuppressive therapy in patients from
endemic areas.
Case 8
• A 5 year old child is sent home from school
because the school nurse notices head lice.
The child’s father calls in a panic with a
number of questions.
– What diseases do they carry?
• None
– Should they shave the child’s head?
• No
Case 8
– What medication should they use to treat them?
•
•
•
•
•
Pyrethrin (Several preparations, OTC)
Permethrin (Nix) (OTC)
Malathion (Ovide)
Lindane (Kwell)
Ivermectin (Stromectol) [not FDA approved for this]
– What should they do with bedding and clothing?
• Wash in routine manner
– How many courses of treatment?
• Retreat in 7-10 days
– Should they treat the family dog?
• No
Case 9
• 24 year old college student with several weeks
of intense pruritus on trunk and associated
rash.
• Minimal response OTC hydrocortisone lotion
• Sex partner developed similar problem a few
days ago
Case 9
• Treatment is single dose Ivermectin
• Pruritus may last for many weeks
– This does not require retreatment
– Manage with topical steroids and antihistamines
Case 10
• A 86 year old healthy man returns from his
honeymoon in Egypt with new onset diarrhea.
He has about 5 loose to watery stools/day. He
is otherwise well. This persists for 2 weeks.
Stool cultures and three stools for O & P were
negative.
NOW WHAT?
There are several reasons why parasites, though
present, might not be identified in a stool
•
•
•
•
Who was doing the looking?
How many stools were collected?
How well were the stools collected?
Should one sample the duodenum?
Intestinal Spore-Forming Protozoa
Cryptosporidia, Isospora, Microsporidia, Cyclospora
• All, but microsporidia are common causes of
disease in normal hosts
• In normal hosts the disease is typically an
acute diarrhea that lasts 3 - 25 days
• No leucocytes in the stool
• Modified acid fast stain can be routinely used
to visualize all but microsporidia
Intestinal Spore-Forming Protozoa
• All are transmitted from human to human
– cryptosporidia can also be acquired from animals
– resistant to halides
• All cause disease in the enterocyte.
– they do not invade below the epithelial surface
• All have a world-wide distribution
• All are frequently AIDS related pathogens
• All can produce asymptomatic infection
Case 11
• A 24 year-old from Montana went on a three
week Central American excursion by bicycle.
Two days before he returned home he
developed low-grade fevers. The next day he
had rigors and myalgias.
• After returning home he was taken to a
hospital emergency room by his mother.
• A blood smear revealed:
Malaria Made Simple
• Think of it
• Is it falciparum or not?
• If falciparum was the traveler in an area where
there is chloroquine resistance?
Falciparum Features
• Where was the
traveler?
• How long has the
traveler been back?
• Smear
– High likelihood
• Only rings
• High % parasitemia
• Banana shaped
gametocyte
• Cells of all sizes
– Suggestive
• Multiply infected cells
• Applique
• Double chromatin dots
Diagnosis? Treatment?
EXO-ERYTHROCYTIC
S
HYPNOZOITES
GAMETOCYTES
ERYTHROCYTIC
CASE 12
• A 45 year old municipal judge comes in with
the compliant of parasites coming out of her
skin. For the past 4 months she has noticed
intense migratory but total body pruritus.
When she scratches at her skin she pick off
small black “parasites” that seem to emerge
spontaneously. In addition she has been
checking her stool and has noticed long
mucinous worms.
CASE 12 (cont)
• She is otherwise well.
• This all started after a one week vacation in Jamaica
• She has been to two dermatologist and an infectious
diseases physician who have told her she does not have
parasites and that “it is in my head”. She has brought in 25
examples wrapped in tissue paper for you to see.
• Weight stable. Menses normal
• Physical Examination: well, anxious appearing. Scattered
areas of excoriation
• Basic blood testing normal. Her “parasites” are a collection
scabs, lint, dried mucous, and some plant material
CASE 12
• Does she have “real” disease?
– DELUSIONAL PARASITOSIS (MORGELLONS
DISEASE)
• Can she be effectively treated?
• Yes
• Pimozide
QUESTIONS?