Fecal Microbial Transplant:
You’re doing what?
Objectives:
1. Review the benefits of Fecal Microbial
Transplant for patients.
2. Discuss considerations in developing an FMT
program.
3. Review current FDA regulations regarding
FMT.
“It is now well-appreciated that intestinal
microbiota constitute a microbial organ that is
integral to overall host physiology, including
pivotal roles in metabolism and immune
system function.”
Disorders associated with an altered intestinal microbiome
GI
• Cholelithiasis
• Colorectal cancer
• Hepatic encephalopathy
• Idiopathic constipation*
• IBS*
• IBD*
• Familial Mediterranean fever
• Gastric carcinoma and lymphoma
• Recurrent Clostridium difficile infection*
Disorders associated with an altered intestinal microbiome
Non-GI
• Arthritis
• Asthma
• Atopy
• Autism*
• Autoimmune disorders
• Chronic fatigue syndrome*
• Diabetes mellitus and
insulin resistance*
• Eczema
• Fatty liver
• Fibromyalgia*
• Hay fever
• Hypercholesterolemia
• Idiopathic
thrombocytopenic purpura*
• Ischemic heart disease
• Metabolic syndrome*
• Mood disorders
• Multiple sclerosis*
• Myoclonus dystonia*
• Obesity
• Oxalic acid kidney stones
• Parkinson’s disease*
Reasons for FMT
• “So far, recurrent CDI appears to represent the
clearest known example of near-complete
disruption of the intestinal microbiota
resulting in gastrointestinal dysfunction. “
C. difficile Statistics
• The average total cost for a single inpatient C.
difficile infection (CDI) is more than $35,000, and
the estimated annual cost burden for the
healthcare system exceeds $3 billion.
• C. difficile infection (CDI) is the leading cause
of antibiotic-associated diarrhea and a highly
problematic healthcare-associated infection.
• In at least one U.S. region, C. difficile has replaced
methicillin-resistant Staphylococcus aureus (MRSA)
as the most common cause of HAI.
• A total of 336,600 CDI-related hospital stays
were documented in 2009; representing 0.9
percent of all U.S. hospital stays. In 67 percent
of these hospital stays, CDI was listed as a
secondary diagnosis.
• The highest rate of CDI-related hospital stays
were in the Northeast, followed by the
Midwest, South, and West regions.
• Persons 65 years of age or older have been
most affected, representing over two-thirds of
patients with CDI.
• The incidence of CDI has increased to epidemic
proportion over the past 10 to 15 years.
• In the United States, from 1996 to 2003, CDI
increased from 98,000 to 178,000 cases and to
61/100,000 hospital discharges, whereas the
unadjusted case-fatality rate rose from 1.2% in
2000 to 2.3% in 2004.
• It is now estimated that 500,000 to 3 million
cases of CDI occur annually in U.S. hospitals and
long-term care facilities, with an estimated
hospital excess cost of care of approximately
$3.2 billion.
C. dificile Infection
• first-line treatment is cessation of the culprit
antibiotic, if possible, then
• treatment with metronidazole, vancomycin, or
fidaxomicin, depending on disease severity.
Recurrence
• recurrence rates are 15 %to 35 %
• Patients who have one recurrence have up to
a 45 % chance of a second recurrence.
• after a second recurrence, up to 65 % of
patients will have a third.
Quality of life in recurrent C. difficile
infection
•
•
•
•
•
Symptoms
Lifestyles changes
Worklife affected
Financial considerations
Hopelessness
Recurrence Treatments
• Recurrences are usually treated with
additional courses of metronidazole, oral
vancomycin, or prolonged oral vancomycin in
various pulsed-tapered regimens, occasionally
"chased" by other antibiotics such as
rifaximin.
What is FMT?
• Transplanting a donor’s feces into a recipient’s
colon via a range of methods.
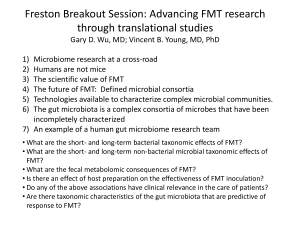
FMT research
• In all, 92 percent of patients were cured of
their recurrent C. difficile, with a range of 81
percent to 100 percent.
Long term follow up on FMT
•
•
•
•
5 medical centers and 77 patients
Patients followed for three months
Primary cure rate: 91%
Secondary cure rate: 98% (defined as cure enabled
by use of antibiotics to which the patient has not
responded before the FMT or by a second FMT.)
• Patients had an average of 11 months of
symptoms prior to FMT.
• Resolution of diarrhea within three days: 74%
Netherlands study 2012
• randomly assigned patients to receive one of
three therapies:
• an initial vancomycin regimen (500 mg orally four times
per day for 4 days) followed by a bowel lavage and
subsequent infusion of a solution of donor feces
through a nasoduodenal tube
• a standard vancomycin regimen (500 mg orally four
times per day for 14 days);
• a standard vancomycin regimen with bowel lavage.
• The primary end point was the resolution of
diarrhea without relapse after 10 weeks.
Research study halted for ethical reasons
• Success rate necessitated offering the FMT to all
participants
Results
• 16 patients received FMT
• 81% had resolution of diarrhea after first FMT
• second infusion of FMT from a different donor : 67%
resolution of diarrhea
• 31% of patients receiving vancomycin had resolution
of diarrhea
• 23% of patients receiving vancomycin with bowel
lavage had resolution of diarrhea
• No significant differences in adverse events among
the three study groups were observed except for
mild diarrhea and abdominal cramping in the FMT
group on the infusion day.
John Muir Health’s story
• Once upon a time, Stephanie Haskell RN went
to the national SGNA conference in 2012 and
heard about the effective and life
transforming treatment utilized on a patient
with recurrent cdi.
• She remembered that one of her departments
physicians had been advocating for FMT for
years and the whole department had
responded “over our dead bodies” (or
something like that)
• She became an advocate for FMT
Starting an FMT program
• Who wants it to happen?
• More than just knowing HOW to do FMT
• Many hospital departments have an opinion,
lots of key players
• Make it a team effort. Get lots of input from
different specialities.
• Know that it will take longer than you think it
should and you may have unexpected speed
bumps along the way.
• Avoid making promises to patients who are
waiting for procedures.
Key players
• Identify your core team: MD, RN’s and Tech’s,
Department Director.
• Get administrative buy-in and support.
• Add in Infection Control (both hospital
department staff and Infectious Disease
MD’s), Tissue Bank MD, Laboratory leadership,
research department MD, Investigational
Research Board, Legal/Risk personnel, Medical
chair of hospital.
Build a structure with policy
•
•
•
•
•
Purpose
Who can perform FMT and where
Donor Selection Criteria
Donor Exclusion Factors- relative and absolute
Donor Screening – time frame, testing
Policy (con’t.)
•
•
•
•
•
•
•
•
Recipient Exclusion Criteria
Recipient Screening
Procedure
Informed Consent
Patient/Family Education
Patient and donor contact information
Documentation
Reference literature for your policy rationale.
Follow with procedural plan
• This is where little details get figured out
• Allow room for individual processes while
describing key considerations. ( i.e. containers
for mixing donor stool with saline is less
important than the goal of mixing stool and
saline to achieve a thin slurry. )
• New considerations will come up as you do
your first cases.
Equipment
• Donor supplies
• Transplant preparation
• Recovering isolation patient
Current FDA Considerations
• Is FMT a biologic agent requiring an
investigational drug application?
• FDA requirements as of July 2013
• http://www.fda.gov/downloads/BiologicsBloodVaccines/Guid
anceComplianceRegulatoryInformation/Guidances/Vaccines/
UCM361393.pdf
We, FDA, are informing members of the medical
and scientific community, and other interested persons
that we intend to exercise enforcement discretion
regarding the investigational new drug (IND)
requirements for the use of fecal microbiota for
transplantation (FMT) to treat Clostridium difficile (C.
difficile) infection not responding to standard
therapies. FDA intends to exercise this discretion
provided that the treating physician obtains adequate
informed consent from the patient or his or her legally
authorized representative for the use of FMT products.
Informed consent should include, at a minimum, a
statement that the use of FMT products to treat C.
difficile is investigational and a discussion of its
potential risks. FDA intends to exercise this discretion
on an interim basis while the agency develops
appropriate policies for the study and use of FMT
products under IND.
Translation
• Informed consent with discussion of risks and
benefits
• Patient must be notified that FMT is
investigational
References:
1. Petrof , E., Gloor, G., Vanner, S., Weese, S., Carter, D., Daigneault, M., Brown, E., Schroeter, K., Allen-Vercoe,
E.,: Stool substitute transplant therapy for the eradication of Clostridium difficile infection:
‘RePOOPulating’ the gut. Microbiome 2013 1:3.
2. O’Keefe SJD. Tube feeding, the microbiota, and Clostridium difficile infection. World Journal of
Gastroenterology. 2010;16(2):139-42.
3. Bakken, J. S., Borody, T., Brandt, L. J., Brill, J. V., DeMarco, D. C., Franzos, M. A., ... Khorut, A. (2011).
Treating Clostridium difficile Infection With Fecal Microbiota Transplantation. CLINICAL
GASTROENTEROLOGY AND HEPATOLOGY, 9, 1044-1049.
4. Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, Pepin J, Wilcox MH: Clinical practice
guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare
epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect
Control Hosp Epidemiol 2010, 31:431–455.
5. Brandt, L., Aroniadis, O., Mellow, M., Kanatzar, A., Kelly, C., Park, T., Stollman, N., Rohlke, F., Surawicz, C.,
Long Term Follow-Up of Colonic Fecal Microbiota Transplant for Recurrent Clostridium difficile
Infection. The American Journal of Gastroenterology. 2012, 107
6. Kelly, C.P. Fecal Microbiota Transplantation – An Old Therapy Comes of Age. The New England Journal of
Medicine :2013, 368:5.
7. Van Nood, E., Vrieze, A., Nieuwdorp, M., Fuentes, S., Zoetendal, E., deVos, W., Visser, C., …Keller, J.
Duodenal Infusion of Donor Feces for Recurrent Clostridium difficile. The New England Journal of
Medicine. 2013,368:5
8. Brandt, L., Aroniadis, O., An overview of fecal microbiota transplantation: techniques, indications, and
outcomes. Gastrointestinal Endoscopy, August 2013, Vol. 78, Issue 2, Pages 240-249