Basics of Mechanical ventilation
advertisement

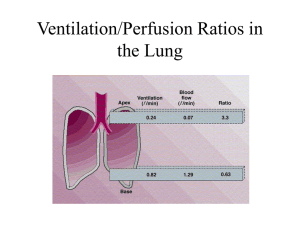
PRINCIPLES OF MECHANICAL VENTILATION BY: DR. AHMED S. EL-KOMI, MD Specialist of Anaesthesia & ICU Farwaniya Hospital 1 Introduction • Cornerstone for intensive care medicine • The ventilators must overcome the pressure generated by the elastic recoil of the lung at end inspiration plus the resistance to flow at the airway. • Ventilators provide infusion of a blend of air or oxygen into the circuit. History • In 1543, Vesalius demonstrated the ability to maintain the beating heart in animals with open chest. • In 1780, such technique were first applied to humans • In 1887, fell-o-dwyer apparatus was used for translaryngeal ventilation via a bellows. • In 1928, the drinker–Shaw iron lung based on negative pressure ventilation • From 1930-1950 – such machines were the mainstay in ventilation of victims of polio epidemics Drinker-Shaw iron lung MECHANICAL VENTILATION 1. 2. 3. 4. 5. 6. 7. Objectives Clinical conditions need ventilator support Physiological effects Types Complications Monitoring Weaning Objectives Overcome mechanical problems: • Rest fatigued muscles • Administer anesthesia and NMB • Prevent or treat atelectasia Regulate gas exchange: • • • • • Normalize PaCO2 PaCO2 < Normal ICT and correct metabolic acidosis PaCO2 > Normal Permissive hypercapnia Reverse hypoxaemia Myocardial O2 consumption Increase Lung volumes • During end inspiration improve V/Q Treatment of severe hypoxemic respiratory failure • During end expiration improve FRC by PEEP Treatment of ARDS, postoperative atelectasis and alveolar collapse • It is the volume remaining after normal expiration • Act as an oxygen reserve maintain oxygenation of blood passing the lung during expiration / breath holding. (PAO2 decreased by 3 mmHg during expiration) Clinical conditions need ventilator support Pulmonary Extra pulmonary ARDS P’ cardiothor. Surg BA Head Trauma Acute COPD Severe NM def. Chest Trauma Drug overdose Severe pneumonia Sepsis Physiological effects • Cardiovascular system Positive pressure ventilation results in: 1. Rise in pleural pressure 2. Rise in intra-abdominal pressure 3. Increased lung volumes All these produce cardiovascular changes Physiological effects Preload LV preload reduced by a variety of mechanisms Venous return • In a volume resuscitated patient venous return does not fall • Intrathoracic pressure is positive rather than negative but • Intra-abdominal pressure also rises • Pressure gradient between abdomen and thorax is maintained Physiological effects • In a volume depleted patient Positive pressure intrathoracic Collapse of intra-abdominal veins and SVC • Abdomen collapse behind the liver as a result of positive pleural pressure transmitted through the diaphragm and liver • Superior vena cava results in a fall in venous return • RV stroke volume and hence LV preload Physiological effects • Renal • Renal blood flow falls if cardiac output falls • Decreased sodium secretion due to fall in cardiac output and decreased secretion of atrial natriuretic factor • Increased water retention due to increased secretion of ADH, particularly in children. • CNS Increased intrathoracic pressure decreases venous drainage from head and may increase ICP. MECHANICAL VENTILATION • Non-invasive ventilation • Invasive ventilation Non-invasive ventilation • Indications » Decreased ventilation » Increased work of breathing » Post-extubation for some COPD patients • Types – Face mask / Nasal cannula – Non-invasive mechanical ventilation Non-invasive ventilation Non-invasive mechanical ventilation – BiPAP • Bi-level CPAP • Two pressure levels (PH & PL) – IPAP (PH) – EPAP (PL) • Delivered by nasal or full face mask Non-invasive ventilation • Advantages 1. Avoids intubation 2. Preserves lower airways defense mechanisms decrease noso-comial infection (Pneumonia or sinusitis) 3. Decreases patient’s discomfort 4. Preserves speech and swallowing 5. Decreases the amount of sedation 6. Allows application of therapy intermittently 7. Decreases the work of breathing • Hypocarbia • O2 Consumption Non-invasive ventilation • Disadvantages 1. 2. 3. 4. Limited access for airway management Mask discomfort and complications Leaks inadequate ventilation Needs alert and cooperative patient • Contraindications: 1. 2. 3. 4. 5. Facial deformity / fracture Inability to protect airway Excessive secretion Decreased mental status Hemodynamic instability Invasive Ventilation With Intubation 1. Mechanical ventilation 2. T-piece tube What is a breathing machine (mechanical ventilator)? • A breathing machine helps the patient breathe. • It is designed to help patients who cannot breathe adequately on their own. • The breathing machine does not fix any problems of the lungs. • It is a device that simply pushes air and oxygen into the lungs and withdraws carbon dioxide from the lungs. • The lungs must function in order for the breathing machine to be effective Invasive Mechanical Ventilation INDICATIONS Clinical Indices: • Unconsciousness • Apnea • RR > 35 breaths / min • Respiratory muscle paradox (agonal breathing) Invasive Mechanical Ventilation INDICATIONS Respiratory Gas Tension • Direct indices • PaO2 < 50 mmHg (room air) / < 60 mmHg (FiO2 > 0.5) • PaCO2 > 50 mmHg (pH < 7.25) • Derived indices • PaO2/ FiO2 ratio < 200 • PA-aO2 gradient > 300 (FiO2 1.0) • Vd / Vt > 0.6 (N = 0.3) * • Virtual shunt fraction > 20% (N < 5%) Invasive Mechanical Ventilation INDICATIONS Mechanical Indices: • • • • Vt < 5 mL/Kg (N = 7-10 mL/Kg) Vital capacity (VC) < 10-15 mL/Kg (N = 50-55 mL/Kg) Max inspiratory force > -25 cmH2O (-20 or -15) Rapid shallow breathing index (RR/Vt) > 200 breath/min/L • VE < 4 L/min or > 10 L/min Ventilator cycle inspiration pause pause expiration Invasive Mechanical Ventilation CLASSIFICATIONS OF MECHANICAL VRNTILATORS Idea Indications Advantages 1. 2. 3. Disadv. Pressure Controlled Volume Controlled Deliver a volume of air till a preset pressure is reached Constant Pinsp & Variable vol. Deliver a preset volume of air regardless the oposing pressure Constant vol. & Variable Pinsp Neonatal ventilators Transport ventilators Compensate for leaks Protect against barotraumas Recruit collapsed alveoli Deliver less Vt in Paw e.g. circuit kink, obstruction or bronchospasm Adult ICU ventilators OR ventilators Deliver enough Vt in Paw e.g. circuit kink, obstruction or bronchospasm 1. 2. No compensation for leaks Barotraumas Components 1. Bacterial filter 2. Pneumotachometer, valves & solenoids 3. Humidifier 4. Heater/ theremostat 5. Oxygen analyser 6. Pressure manometer 7. Chamber for nebulising drug Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. 2. 3. 4. 5. 6. 7. Tidal Volume (Vt) Respiratory Rate (RR) Inspiratoty Oxygen Fraction (FiO2) I:E Ratio Inspiratory Flow Rate (IFR) Trigger Sensitivity PEEP Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. Tidal Volume (Vt) preset at 7-10 ml/Kg Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. Tidal Volume (Vt) 2. Respiratory Rate (RR) – If the patient is clinically stable 8-14 breath/min – Restrictive lung disease RR – Chronic respiratory acidosis RR – Too high RR Respiratory alkalosis - barotraumas – Too low RR hypoventilation - work of breathing Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. 2. Tidal Volume (Vt) Respiratory Rate (RR) 3. Inspiratoty Oxygen Fraction (FiO2) Adjusted according to ABG within 20-30 min to keep SaO2 > 90% and PaO2 > 60mmHg 4. I:E Ratio Normally 1:2 - in ARDS: IRV 2:1 Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. 2. 3. 4. Tidal Volume (Vt) Respiratory Rate (RR) Inspiratoty Oxygen Fraction (FiO2) I:E Ratio 5. Inspiratory Flow Rate (IFR) = tidal volume/inspiratory time Vt/Ti set at 40-90 L/min • High IFR ≥ 90 L/min – Used in COPD to increase Te AutoPEEP – Disadvantages: PIP risk of barotrauma • Low IFR ≤ 40 L/min – Used in ARDS to avoid PIP and risk of barotraumas – AutoPEEP Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. 2. 3. 4. 5. Tidal Volume (Vt) Respiratory Rate (RR) Inspiratoty Oxygen Fraction (FiO2) I:E Ratio Inspiratory Flow Rate (IFR) 6. Trigger Sensitivity Determines start of inspiration Pressure set at -0.5 to 2.0 – -0.5 too sensitive self cycling – -2.0 too insensitive work of breathing Invasive Mechanical Ventilation INITIAL VENTILATOR SETTINGS 1. 2. 3. 4. 5. 6. Tidal Volume (Vt) Respiratory Rate (RR) Inspiratoty Oxygen Fraction (FiO2) I:E Ratio Inspiratory Flow Rate (IFR) Trigger Sensitivity 7. PEEP Positive end-expiratory pressure Holds alveolar sacs open and recruits more alveoli Preset (physiological) = 3-5 cmH2O Invasive Mechanical Ventilation Invasive Mechanical Ventilation Your patient acutely develops inadequate alveolar ventilation despite correct alveolar settings What causes must you rapidly rule out? Invasive Mechanical Ventilation Invasive Mechanical Ventilation MODES OF MV i. ii. iii. A/C SIMV PSV Assisted Control Synchronized IMV Pressure Support Vent. Invasive Mechanical Ventilation MODES OF MV i. A/C • • • • Assisted Control Volume controlled mode (preset Vt + RR) The ventilator senses any patient-generated resp. effort and intermediately follows with a full machine-powered breath Little patient’s work of breathing Respiratory alkalosis is common Invasive Mechanical Ventilation MODES OF MV iii. • • SIMV Synchronized IMV The ventilator senses the patient’s spontaneous breath and times the machine-delivered breaths with the patient’s breathing cycle SIMV prevents breaths stacking Which is the best ventilation mode for each of the following clinical scenarios ? A trauma patient who is totally apneic SIMV ARDS patient with very low lung compliance A/C 24HRS P’ laporotomy with spont. breaths PCV Which is the best ventilation mode for each of the following clinical scenarios ? A trauma patient who is totally apneic SIMV ARDS patient with very low lung compliance A/C 24HRS P’ laporotomy with spont. breaths PCV Invasive Mechanical Ventilation COMPLICATIONS 1) RESPIRATORY: – Hypo or hyperventilation – Complications of excessive pressure and flow rates • Pulmonary barotraumas • Pulmonary volutrauma – – – – Patient/ventilator asynchrony Ventilator malfunction Ventilator associated pneumonia Complications of tracheal intubation Invasive Mechanical Ventilation COMPLICATIONS 2) CVS: Effects of ITP and PEEP Cardiac output Hepatic blood flow RBF ICP 3) OXYGEN TOXICITY: 4) GIT: GIT bleeding GIT colonization Invasive Mechanical Ventilation COMPLICATIONS 5) 6) RENAL: NUTRITIONAL: UOP – Caloric requirements – PaCO2 7) PSYCHOLOGICAL TRAUMA: 8) ADJUVANT DRUGS SIDE EFFECTS: – Morphine – Benzodiazepines – NMBs Monitoring • Clinical • Radiological • Biochemical • Bacteriological • others Clinical monitoring General Appearance • Level of activity • Response to stimulus • Eye opening • Posture • Perfusion • Color • Edema Clinical monitoring Adequacy of mechanical breath • Movement of chest • Retractions • Synchronization • Air entry Clinical monitoring Monitoring of O2 & CO2 status • Pulse oximetry • EtCO2 monitoring • ABG analysis • Capillary gas determination • Transcutaneous monitoring • Oxygenation indices Clinical monitoring Ventilator Parameters • PIP • PEEP • MAP • RR • Ti & I:E Ratio • FiO2 • VT • Trends of Ventilator Parameters • Pulmonary Graphics Hemodynamic Stability • Oxygenation • Adequacy of Circulation Radiological Monitoring When to do CXR ? • At the start of ventilation • After ET tube change • Sudden deterioration • Prior to extubation • Post extubation Biochemical Monitoring • Blood Gases • Blood Sugar • Serum calcium • Serum electrolytes Bacteriological Monitoring Blood culture ET tube culture Other Monitoring • Humidification & warming of ventilator circuit gases • Position of patient • Skin • Fluid & electrolytes • Nutrition status • Sensorium • Infection control Invasive Mechanical Ventilation WEANING Definition: Process by which ventilator-dependent patient is removed from ventilator Invasive Mechanical Ventilation VC > 15 ml/kg Standard criteria for initiating Max inspiratory pressure > -25 cm H2O weaning: Tobin Index of rapid and Patient awake and shallow breathing RR/Vt cooperative Clinically and radiologically – RR/Vt>105 95% wean attempts unsuccessful resolving lung disease – RR/Vt<105 80% successful PaO2>60 mmHg on FiO2 <0.4 and < 10 cm PEEP PaCO2 <50 mmHg RR < 30/min Minute volume >10 L/min WEANING Approaches To Weaning • • • • SIMV – low rate Spontaneous breathing trials (SBT) Pressure support ventilation (PSV) New weaning modes - ASV Mechanical Ventilation Rest 24 hrs PaO2/FiO2 ≥ 200 mm Hg PEEP ≤ 5 cm H2O Intact airway reflexes No need for continuous infusions of vasopressors or inotrops > 100 RSBI <100 Stable Support Strategy Assisted/PSV 24 hours Daily SBT Low level CPAP (5 cm H2O), Low levels of pressure support (5 to 7 cm H2O) “T-piece” breathing 30-120 min Yes RR > 35/min Spo2 < 90% HR > 140/min Sustained 20% increase in HR SBP > 180 mm Hg, DBP > 90 mm Hg Anxiety Diaphoresis No Extubation Invasive Mechanical Ventilation WEANING Correction of factors complicates weaning: a) Bronchospasm b) Malnutrition c) Anemia d) Infection e) Metabolic alkalosis f) Sleep deprivation g) Increased CO2 production h) Hypothermia or hyperthermia