To Intubate or Not to Intubate…
advertisement

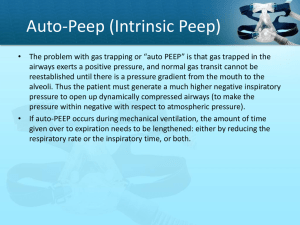
Hi and Welcome Everybody! To Intubate or Not to Intubate… (or the Effective Use of NPPV in the Acute Setting) By Timothy A. Revell RRT St. Joseph Mercy Hospital, Ann Arbor, MI Patient Population • COPD (including Asthma) Exacerbations • CHF • Community Acquired Pneumonia (CAP,with increased W.O.B. and/or hypoxemic / hypercarbic resp. failure) • With regards to location, it’s wherever the patient presents with an exacerbation of their disease; ER, GMB, ICU, etc. Here’s the scenario…or “no kiddin’, there I was…” It’s a typical day/night at work, when you receive a stat call from the emergency room stating that EMS is bringing in a “diff breather” into the resuscitation room and that they’re about 5 minutes out. So, being the super-therapist that you are, you decide to bring both a vent and a bipap machine with you. EMS soon arrives, and sure enough, there sits Mr. Claus in the classic “tripod” position. He’s in severe respiratory distress, only speaking 1-2 words at a time… Fearing that you’ll “never get this guy off the vent” if he ends up intubated, you decide to try BiPAP first. For settings, you decide to put him on 12/6 and an Fi02 of .50 and encourage Mr. Claus to “breathe slow deep breaths” as best he can. Over the course of the next 30 minutes, Mr. Claus is given IV steroids and several NMTs through the BiPAP (which have little, if any, effect). You next draw an ABG and await the results. A CXR is done which shows classic hyperinflation with no infiltrates present). In the meanwhile, Mr. Claus doesn’t appear to be making much in way of progress and is becoming somnolent. Finally, about 20 minutes later you receive the ABG results. Mr. Claus’ PaC02 is 68 and his pH is 7.25. At this point, you discuss the results with the ER physician and you both decide that Mr. Claus has “failed” BiPAP and needs to be intubated. Sound familiar? It should. This very same scenario is played out countless times every day in the ER’s, ICU’s, GMB’s, etc. throughout the nation. And, in my opinion, in most cases, these intubations can be avoided. How? The key, I believe, is in the settings we use with BiPAP in meeting our patients’ physiologic needs. So let’s back up and try this again… But first… A few quick points: • Our patients’ physiologic needs are very different in the acute setting (they are also very dynamic) than their baseline. • The goal when using BiPAP is to match our patients’ needs. • It is in our assessment that we find out what those needs are (and what settings to use to meet those needs), i.e. no “cookie cutter” settings. This time, when you put Mr. Claus on BiPAP, you notice that there is a delay between Mr. Claus’ trying to initiate a breath (by observing his abdomen) and the machine delivering the breath. You recognize this as auto-peep and dial up the EPAP 1-2 cmH20 at a time until the delay goes away (you find that you also have to dial up the IPAP to keep the EPAP from encroaching on it). You find that the EPAP is now 14cmH20, but the delay is gone. You next look at his inspiratory effort and notice that he’s still trying to take a breath when the machine terminates it. You also notice that he still has supraclavicular retractions. You then dial up the IPAP to meet his efforts, going up 1-2 cmH20 at a time until those retractions go away. You find that your IPAP is now 24 cmH20 (you also make other changes to fine-tune the delivered breaths, such as Rise Time % and I-Time). You then ask Mr. Claus if he feels like he’s “getting enough air” and he nods his head in the affirmative. Over the course of the next 30 minutes, Mr. Claus is becoming more alert, using less accessory muscles and attempting to talk through the mask (now asking for water). 20 minutes later you draw an ABG and find that Mr. Claus’ PaC02 is 48 and his pH 7.41 An hour after Mr. Claus is started on BiPAP, he begins to say that “it’s too much!”, a great sign that he’s doing much better. You begin to turn down the IPAP and EPAP until, a half hour later, he wants it taken off. You oblige, and long story short, he does just fine without it and is admitted to a “step-down” bed instead of the ICU on a vent. So, what’s the moral of the story? Recognizing our patients’ needs when using NPPV and choosing settings based on that patients’ needs at that moment (and adjusting as our patients’ condition changes). If we commit to doing that, I believe we can keep a good number of those patients from being intubated and out of the ICU.