File - Respiratory Therapy Files
advertisement

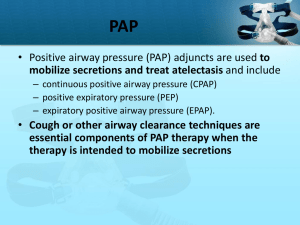
Auto-Peep (Intrinsic Peep) • The problem with gas trapping or “auto PEEP” is that gas trapped in the airways exerts a positive pressure, and normal gas transit cannot be reestablished until there is a pressure gradient from the mouth to the alveoli. Thus the patient must generate a much higher negative inspiratory pressure to open up dynamically compressed airways (to make the pressure within negative with respect to atmospheric pressure). • If auto-PEEP occurs during mechanical ventilation, the amount of time given over to expiration needs to be lengthened: either by reducing the respiratory rate or the inspiratory time, or both. CPAP • CPAP is the application of continuous positive airway pressure, patient is breathing spontaneously. Pressure is at one level • CPAP is a mode, and also a setting • Synonymous with PEEP, and EPAP • Given for a variety reasons, including: – Refractory hypoxemia – OSA – RDS… CPAP • CPAP can be applied non-invasively, through a BiPAP machine, CPAP machine, or SiPAP machine or it can be given invasively through a continuous mechanical ventilator • CPAP is otherwise known as PEEP, can be given to all age groups NASAL CPAP Home vs. Hospital NPPV • Application of positive pressure without airway intubation for the purpose of augmenting alveolar ventilation • Patient’s using NPPV are typically awake/alert and breathing spontaneously Goals of NPPV • Acute Care – Avoid intubation – Improve mortality – Relieve symptoms – Enhance gas exchange – Improve ventilator-patient synchrony – Maximize patient comfort – Decrease incidence of ventilator-acquired pneumonia (VAP) Goals of NPPV • Chronic Care – Relieve or improve symptoms – Enhance quality of life – Avoid hospitalization – Increase survival – Improve mobility Indications for NPPV • Disease states – Asthma • Used in treatment of acute attack to avoid intubation, HHN can be given inline • Many tend to be claustrophobic and don’t tolerate procedure – Acute exacerbation of COPD • Studies indicate that NPPV should be first-line intervention in treatment • Only beneficial in acute exacerbation/HHN treatment can be given inline – Acute cardiogenic pulmonary edema • Administered as first-line treatment, NO HHN treatment indicated • Not recommended for patients with myocardial infarction, arrhythmias, hemodynamic instability, or depressed mental status Indications for NPPV • Other indications – Neurologic/neuromuscular disease • Should always be considered as a first-Line treatment • Works well when applied to patients with progressively deteriorating disease • Will use NPPV until the patient requires invasive PPV – Weaning from ventilatory support • May be indicated for patients who have failed at weaning attempts but for whom clinical signs indicate they should be weaned • May be used with patients failing extubation Indications for NPPV • Other indications – Immunosuppressed patients/patients awaiting lung transplant • Avoidance of intubation – leads to nosocomial pneumonia • Should always be considered as a first-Line treatment – Acute lung injury • Should be applied with caution to ALI patients • If no response within a few hours, patient should be intubated – DNR patients (controversial) • Used to prolong life until family members arrive • Used to transport patient home to die • Provide comfort during last hours of life Indications for NPPV • Chronic care settings – Relief of nocturnal hypoventilation in COPD patients – Nocturnal use for restrictive thoracic diseases • Rest respiratory muscles • Lower PaCO2 to establish new baseline value • Improve lung compliance, lung volume, and reduce dead space – Treat nocturnal hypoventilation • Obesity hypoventilation • Obstructive sleep apnea • Central sleep apnea NPPV for OSA Patients with OSA often use CPAP via face, nasal or nasal pillow masks. Often poorly tolerated. NPPV for OSA • Obstructive sleep apnea (OSA) is the most common type of sleep apnea and is caused by obstruction of the upper airway. It is characterized by repetitive pauses in breathing during sleep, despite the effort to breathe, and is usually associated with a reduction in blood oxygen saturation. These pauses in breathing, called apneas (literally, "without breath"), typically last 20 to 40 seconds. • The individual with OSA is rarely aware of having difficulty breathing, even upon awakening. It is recognized as a problem by others witnessing the individual during episodes or is suspected because of its effects on the body (sequelae). OSA is commonly accompanied with snoring. • Leads to cardiac problems, brain problems, HTN… Selection Criteria for NPPV in Acute Respiratory Failure • Use of accessory muscles • Paradoxical breathing • Respiratory rate > 25 breaths/min • Dyspnea (moderate to severe or increased over normal levels) • PaCO2 > 45 mmHg with pH < 7.35 • PaO2/FIO2 ratio < 200 BiPAP • Two levels of non-invasive positive pressure. • BiPAP is a trademarked name from Respironics • IPAP: Inspiratory positive airway pressure, a pressure limit, increases in IPAP = increases in VT • EPAP: Expiratory positive airway pressure, PEEP, applied on expiration to increase FRC • Set IPAP and EPAP at least 5 apart to create a pressure gradient, this difference is called pressure support Bipap • The BiPAP machine has two basic modes: – S/T (Spontaneous timed): You set a IPAP, EPAP, Rate, inspiratory time and FIO2. The rate only applies when the patient falls below the minimum back up rate, once he or she does the machine is termed time cycled. Otherwise all breaths are spontaneously triggered. Set alarms – CPAP: Set a PEEP/EPAP level, along with FIO2, no back up rate set. Watch for apnea, set apnea alarm Bipap • Typical settings for Bipap: – IPAP 10-15 cmH2O (increase or decrease based on PaCO2) – EPAP 5-10 cmH2O (increase/decrease based on PaO2) – Rate 6-10 (rate set low, patient should be breathing spontaneously) – FIO2 21-100% (based on SpO2, PaO2…) – I-time 1.0 second (usually a non issue since rate is low) – Rise time 0.4 seconds (only applies to timed breath) – Once BiPAP is applied, assess comfort, monitor Vte, RR, HR, SpO2, BP, cardiac rhythm, Ve… – Get a ABG about 1-2 hours after initiation – Leaks are the number one cause of alarm BiPAP • Bipap is typically setup quickly with the mask being the most cumbersome aspect of setup • BiPAP should be used as a temporary means of augmenting/ assisting in a patients respiratory distress. Prolonged use typically suggests the patient may need intubation • Commonly used in the ER for CHF/pulmonary edema, but also for a wide range of other reasons Bipap • The most important factors in applying BiPAP are: – Is the patient a proper candidate for BiPAP or do they need to be intubated – Note contraindications for device – Is the mask appropriate for the patient (correct size and fit) – Proper settings Exclusion Criteria for NPPV in Acute Respiratory Failure • Apnea (NPPV/BIPAP only for spontaneously breathing pts) • Hemodynamic instability • Uncooperative patient behavior (may need sedation) • Facial burns or other trauma • Copious secretions (Devices can dry secretions) • High risk of aspiration • Anatomic abnormalities that interfere with gas delivery Exclusion Criteria in the Chronic Care Setting • Unsupportive family • Lack of financial resources • Uncooperative patient behavior • Copious secretions • High risk of aspiration • Anatomic abnormalities that interfere with gas delivery • Ventilatory support required most waking hours Administration of NPPV – Patient Interfaces • Nasal mask – Triangular in shape; made to fit around the nose – Most common interface – Fitting of mask dependent upon manufacturer’s specifications – Leakage through the mouth can be a significant problem, may need chin strap Administration of NPPV – Patient Interfaces • Full face masks – Surrounds nose and mouth, resting below lower lip – Seal easier to maintain because both mouth and nose covered – Associated with increased dead space, risk of aspiration, and claustrophobia – Asphyxiation can occur in Ventilator failure so alarms must be functional Administration of NPPV – Patient Interfaces • Nasal pillows – Consists of two small cushions that fit under the nose – Has limited pressure range of use – 3 to 20 cmH2O – More comfortable than facial masks, but gas leakage may be a problem. Gas leaks out of the mouth, may need chin strap Administration of NPPV – Patient Interfaces • Total face mask – Surrounds entire face – One size available for quick application in emergencies – Does have increased dead space, but decreases claustrophobic feeling because it does not obscure vision – Alternate masks to reduce pressure sores on face Administration of NPPV – Humidification • Heated humidification has been noted to decrease nasal resistance and congestion • Cold passover humidification does not significantly relieve nasal resistance • Heated humidification increases patient compliance with the procedure Administration of NPPV – Initiation • Successful application requires that the patient be part of the process. They must understand what is to be done and be fully cooperative in the process. Administration of NPPV – Initiation • Place patient at an angle ≥ 30⁰ • Determine correct size and type of patient interface (very important, if patient is uncomfortable they are non-compliant) • Attach patient interface to circuit • Select initial settings – PEEP: 0 – 4 cmH2O – Ventilating pressure: < 5 cmH2O (typically 10-15) – Expected VT: 200 – 500 mL • Once you input your settings and alarms connect to patient Administration of NPPV – Initiation • Select initial settings – FIO2: maintain SpO2 > 90% – Rate: determined by patient, again set low Administration of NPPV – Initiation • Hold the mask on the patient’s face or have the patient hold the mask on the face • When patient is comfortable with mask, use straps to hold in place • Do not overly tighten or let too loose Administration of NPPV – Initiation • Adjust FIO2 as necessary to maintain SpO2 > 90% • Adjust mask as necessary to correct any air leaks, do not put tape on mask to prevent leaks. Ensure exhalation ports are open Administration of NPPV – Initiation • As patient becomes comfortable, adjust inspiratory positive airway pressure (IPAP) until VT is between 4 and 6 mLs/kg or until signs of respiratory distress improve Administration of NPPV – Initiation • Increase expiratory positive airway pressure (EPAP or PEEP) to reduce dyssynchrony from air trapping or to improve oxygenation Administration of NPPV – Assessment • Assessment after initial two hours indicating successful administration – Decrease in PaCO2 – Increase in pH – Increase in PaO2 – Decreased WOB Administration of NPPV – Assessment • Assessment after initial two hours indicating successful administration – Decrease in respiratory rate – Normalization of heart rate and respiratory rate – Normalization of ventilatory pattern Administration of NPPV – Assessment • Failure to observe improvement requires reassessment to determine need for intubation • If patient shows some signs of improvement, continue to evaluate to determine success or failure of procedure and initiate appropriate action • NPPV should be used as a short term application, or used on a nightly or intermittent basis Administration of NPPV – Assessment • Be cautious to avoid prolongation of the procedure; allowing patient to continue too long without significant improvement can create difficulties for intubation or stabilization later Side Effects Side Effect Mask related Discomfort Facial skin erythema Claustrophobia Nasal bridge ulceration Acneiform rash Air pressure or flow related Nasal congestion Sinus or ear pain Nasal or oral dryness Eye irritation Gastric insufflations Possible Remedy Check fit, adjust strap, change to new type of mask Loosen straps, apply artificial skin Use a smaller mask, change type of mask, give sedative Loosen straps, apply artificial skin, change mask type Administer topical steroids or antibiotics Administer nasal steroids, decongestant, or antihistamines Reduce pressure if pain is intolerable Apply nasal saline solution, add humidifier, decrease leak Check mask fit, readjust straps Reassure the patient, give simethicone, reduce pressure to relieve excessive pain Side Effects Side Effect Air leaks Major complications Aspiration pneumonia Hypotension Pneumothorax Possible Remedy Encourage mouth closure, try chin straps, try oronasal mask if using nasal mask, reduce pressure slightly Select patients carefully Reduce IPAP Stop ventilation if possible, reduce airway pressure; insert chest tube if indicated Side Effects Slow skin breakdown by applying Mepilex or DuoDerm tape to patient’s face, typically the bridge of the nose and forehead and sides of face Contraindications • Absolute – Untreated pneumothorax – Patient without a paten airway – Apnea – Inability to fit interface due to deformity Contraindications • Relative – Unstable hemodynamic state – Facial trauma HW assignment • Part 1. Assess the use and application of IPPB and IPV as a means for hyperinflation and bronchial hygiene therapy. Is there evidence supporting there effective use? (2 pages) • Part 2. Explain why or why not the use of BiPAP in DNR patients is justified. I want your opinion on the ethical implications as well as the functionality of the Bipap as a ventilation assistant(2 pages) • Use peer reviewed literature to write a minimum of two pages on each topic. You may email me your articles or attach them with your paper. Use correct referencing • DUE OCTOBER 8th • Michaines@hotmail.com