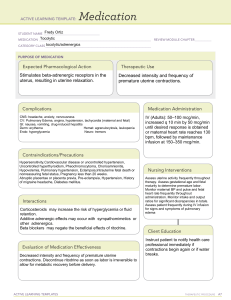
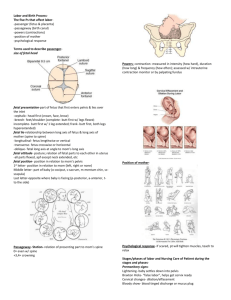
NUR230 Review #1 Signs of Pregnancy Presumptive Amenorrhea Fatigue Nausea and vomiting Breast tenderness Urinary frequency Quickening Probable sign-Lower uterine segment softens -Cervical softening -Bluish discoloration of vagina, cervix Positive pregnancy test Braxton hicks contractions or ballotment Positive Hearing fetal heart tones Visualization of the fetus Palpation of fetal movements by examiner Signs of Pregnancy (Table 7-2, p.152) Pregnancy Terms Gravida- # of pregnancies (including current) Para- # of pregnancies 20 weeks or > Term- 37-40+ weeks (postterm-42+ weeks) Preterm-20-36 6/7 weeks Abortion-any pregnancy that ended prior to 20 weeks (spontaneous or elective Living- # of living children Rule Method for calculating Estimated Due Date (EDD) First day of last menstrual period (LMP) Subtract 3 from the month Add 7 to the day Adjust year if needed Fetal Assessment Fetal heart rate- 110-160 Uterine height in centimeters should equal gestational age +/-2 Fetal movement Cardiac Changes B Blood volume increases 40-50% results in physiological anemia Cardiac output increases 30-50% Respiratory Changes Ligaments of rib cage relax Diaphragm is displaced due to enlarging uterus; chest breathing vs. abdominal breathing Upper respiratory more vascular: congestion, epistaxis, changes in voice Gastrointestinal Changes Hyperemesis gravidarumChanges in taste and smell Pytalism Pica First Trimester Labs Hgb and Hct (CBC) Blood type and Rh Antibody screen Rubella titer (may offer booster after pregnancy) Urinalysis Screening for HIV Screening for Hepatitis B Syphilis (VDRL or RPR) Offer Sickle Cell Offer Cystic Fibrosis Pap Smear Gonorrhea/Chlamydia First Trimester Discomforts Breast enlargement, pain, tingling, tenderness Urgency and frequency of urination Fatigue Nausea and vomiting (morning sickness) Ptyalism (excessive salivation) Gingivitis and epulis (gum hypertrophy, bleeding) Nasal stuffiness Leukorrhea (clear or light colored mucus) Second Trimester Discomforts Acne, pigmentation changes Palmar erythema Pruritus Palpitations Supine hypotension (vena cava syndrome) Faintness, syncope Heartburn Constipation, flatulence Headaches Carpal tunnel syndrome Periodic numbness, tingling of fingers Round ligament pain Joint pain, backache, pelvic pressure Third Trimester Discomforts Shortness of breath and dyspnea Insomnia Mood swings, increased anxiety Urinary frequency and urgency return Perineal discomfort and pressure Leg cramps Ankle edema Third Trimester Labs 1 hour glucose tolerance test, if elevated 3 hour glucose tolerance test Group B Strep vaginal/rectal swab Second and Third Trimester Complications Persistent severe vomiting Sudden discharge of fluid from vagina Vaginal bleeding; severe abdominal pain Chills, fever, burning on urination, diarrhea Severe backache or flank pain Decrease in or absence of fetal movement Uterine contractions Symptoms of preeclampsia Anemia Normal values during pregnancy -Hgb >11 -Hct >33 Occurs in 20% of pregnant women Associated with increased incidence of miscarriage, preterm labor, preeclampsia, infection, postpartum hemorrhage, and intrauterine growth restriction Factors that effect nutrition Incompetent Cervix Passive and painless dilation of the cervical os without labor or contractions of the uterus May occur in late 2nd or early 3rd trimester Related to: -cervical trauma -excessive cervical dilation - Incompetent Cervix: Management Bed rest, hydration, tocolysis Cerclage may be placed at 11-15 weeks, removed at 37 weeks Risks with cerclage: -premature rupture of membranes -preterm labor -infection Placenta Previa Low-lying (C) Partial or marginal (A) Complete (B) Painless bright red vaginal bleeding Never perform a vaginal exam on a woman who is bleeding unless you know location of placenta! Premature separation of placenta from implantation site after 20 weeks Abruptio Placentae (Abruption) Signs: -vaginal bleeding -severe abdominal pain, rigid board-like abdomen -uterine contractions; hypertonus -port wine stained amniotic fluid Preeclampsia: Symptoms Mild -BP 140/90 or greater Severe -BP 160/110 or greater -Persistent or severe headache -blurred vision; photophobia -epigastric pain -intrauterine growth restriction of fetus Only cure is delivery of infant! HELLP Syndrome Can occur with severe preeclampsia Laboratory diagnosis H E L L P Hemolysis Elevated Liver enzymes Low Platelets Medications Magnesium Sulfate- CNS depressant, smooth muscle relaxant; used to prevent seizures -Loading dose -Maintenance dose Assessment: -RR (12 or >) -LOC -Clonus -Urine output -Serum mag level (<9mg/dL) Calcium Gluconate at bedside as antidote Pregestational Diabetes Type 1 or Type 2 Glucose crosses placenta; insulin does not Fetus produces insulin around 10th week First trimester (weeks 7-15) prone to hypoglycemia due to metabolic changes related to hormones Second and third trimester insulin needs may double or quadruple Complication Risks Maternal: -early pregnancy loss -macrosomia (infant >4000gms) -comorbidities (esp hypertensive disorders) -preterm labor -polyhydramnios -more common & serious infections -postpartum hemorrhage - Complication Risks Fetal: -unexplained fetal death -congenital anomalies -macrosomia -hypoglycemia -respiratory distress -prematurity Gestational Diabetes Risk Factors: -obesity -family history -age >35 -comorbidities -having a previous infant >9lbs at birth Screening: -1 hour glucose tolerance test 24-28 weeks -if abnormal followed by 3 hour OGTT GDM: Treatment First step: dietary modifications and exercise Second step: insulin Oral antidiabetics not often used because they cross the placenta. Insulin does not cross the placenta. Complications: can be same as with pregestational diabetes At a greater risk of developing diabetes later in life Preterm Labor Diagnosis based on 3 factors: -20-36 6/7 weeks gestation -uterine activity (contractions) -progressive cervical change (effacement and/or dilation Risk factors: history of PTL, multiple gestation, 2 nd trimester bleeding, African-American race, low prepregnancy wt, genital tract infections Signs of PTL Painful or painless contractions every 10 minutes for 1 hour or more Lower abdominal cramping Painful menstrual-like cramps Dull, intermittent low back pain (below waist) Suprapubic pain or pressure Change in character of cervical discharge or amount Rupture of amniotic membranes Signs of UTI Treatment of PTL Tocolytic medications- (relax smooth muscle): -terbutaline: oral or SC (must take pulse rate, if >120 hold medication) -magnesium sulfate -Indocin -Procardia Passenger (fetus) Passageway (birth canal) Powers (Contractions) Position (mother) Psychologic response Passenger Presentation- part entering pelvic inlet first -cephalic (vertex) -breech (buttocks, feet or both) -shoulder (scapula) Fetal lie, attitude and position all factors that determine presenting part Fetal Lie RELATION OF LONG AXIS (SPINE) OF FETUS TO LONG AXIS (SPINE) OF MOTHER LONGITUDINAL/VERTICAL: PARALLEL TRANSVERSE: AT A RIGHT ANGLE OBLIQUE: AT AN ANGLE Fetal Attitude Fetal head flexed or extended Typically flexed, chin to chest, allows easy passage through maternal pelvis If extended may not be able to fit through pelvis Fetal Position Relationship of reference point on presenting part (occiput, sacrum, mentum) to the four quadrants of the maternal pelvis Denoted by 3 letters 1st- location of presenting part (right or left) 2nd- specific presenting part 3rd- location of presenting part in relation to pelvis (anterior, posterior or transverse) Fetal Position Occiput- back of head Mentum- face Fetus in occiput Fetus in occiput posterior position anterior position Station Relationship of presenting part to an imaginary line drawn between the maternal ischial spines Engagementlargest diameter of presenting part is at level of ischial spines 0 Station +2 Station Problems with Passageway Macrosomia Cephalopelvic disproportion(CPD)maternal pelvis Pelvic Shapes Powers Primary-involuntary contractions -effacement-thinning of cervix (0-100%) -dilation- opening of cervix (0-10cm) Secondary- mothers bearing down or pushing with contractions Ineffective Primary Powers Amniotomy- puncture hole in amniotic sac; fetal head applies pressure to cervix Priority assessment- FHR; also assess amount, color, odor Augmentation- IV Pitocin; increase amount until contractions are every 2-3 mins & moderate intensity Induction of Labor Chemical or mechanical initiation of uterine contractions before their spontaneous onset Chemical -prostaglandins to ripen (soften)cervix may stimulate contractions Cytotec, Cervidil, Prepidil -Pitocin Mechanical -foley catheter balloon -laminaria -stripping of membranes Ineffective Secondary Powers Maternal Position Change positions frequently- helps to relieve fatigue, promotes comfort Positions for second stage of labor (pushing) dependent on condition of mom and baby and PHCP preference Seven Cardinal Movements of Labor Signs Contractions True Labor vs False Labor Cervical Change Change in Position or Activity Mucous Plug (bloody show) True Labor Regular Become longer, stronger and closer together Cervix begins to dilate and/or efface No effect on contractions Present False Labor Irregular with no established pattern No cervical change Contractions will decrease or stop Not present Rupture of Membranes Methods to determine ROM -nitrazine paper -fern test -Amnisure swab Increased risk of infection if > 24 hours What do we assess? Priority FHR Monitor temperature q2 hours Stages of Labor Stage 1: Stage 2: Stage 3: Stage 4: Dilation (0-10 cm) Expulsion (delivery of infant) Delivery of Placenta Immediate Recovery (1-4 hours) Dilates 0-5 cms Contractions: 5-30 mins apart, 30-40 seconds, mild-moderate intensity Stage 1: Early Phase Promote comfort, ice chips, empty bladder q2h, encourage breathing and relaxation Assess FHR, VS q4h (unless ROM then q2h) Usually happy, excited, thoughts center on self, labor and baby. Dilates 6-10cm Contractions: 1.5-5 mins, 40-90 seconds, moderate to strong intensity Stage 1: Active Phase Becomes more labor focused, may ask for and receive pain medications; may feel rectal pressure and have urge to push Cannot push until 10cm, if she pushes before this the cervix may swell, a swollen cervix does not dilate! Promote comfort, position changes, ice chips, assist with breathing techniques and relaxation, empty bladder frequently (full bladder can inhibit fetal descent); lots of encouragement Monitor FHR (may note early decels on strip), VS More serious, doubtful, apprehensive, irritable, intense; may want companionship; needs encouragement; difficulty following directions Epidural anesthesia is a regional anesthesia that blocks pain in a particular region of the body. The goal of an epidural is to provide analgesia, or pain relief, rather than anesthesia, which leads to total lack of feeling. Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body. Pain Management in Labor Epidural medications fall into a class of drugs called local anesthetics, such as bupivacaine, chloroprocaine, or lidocaine. They are often delivered in combination with opioids or narcotics such as fentanyl and sufentanil in order to decrease the required dose of local anesthetic. This produces pain relief with minimal effects. These medications may be used in combination with epinephrine, fentanyl, morphine, or clonidine to prolong Low blood pressure Loss of bladder control Potential side effects of epidural anesthesia Itchy skin Feeling sick Inadequate pain relief Headache Slow breathing Temporary nerve damage Infection Permanent nerve damage Stage 2: Delivery of Infant Begins when 10 cm dilated, ends with deliver of infant Contractions may space out Can last up to 2 hours Requires a lot of energy May feel burning when fetal head reaches perineum (+4 station) Delivery of infant through abdominal incision Cesarean Section -low transverse (bikini cut) -vertical-ALWAYS a repeat c-section -hx of uterine rupture must always have repeat c-section Primary or elective Trial of labor after cesarean (TOLAC) Vaginal birth after a cesarean (VBAC) Stage 3: Delivery of Placenta Begins with delivery of infant, ends with delivery of placenta Spontaneous or manual Separation noted by firmly contracted uterus, sudden gush of dark blood and lengthening of umbilical cord Examined to ensure it is intact Fragments of placenta left in uterus can result in postpartum hemorrhage and infection Fetal side (shiny shultz), maternal side (dirty duncan) Cultural considerations Stage 4: Immediate Recovery First 1-4 hours after delivery Mother recovering from birth process, infant adapting to extrauterine life VS monitored q15 min first hour, q30 min second hour, temp at beginning and end unless abnormal Assess fundus (@U or slightly above), lochia, perineum, incision site with Cesarean section, keep bladder empty, assess for return of sensation and movement if pt had epidural Cultural Considerations Discuss any concerns or requests related to culture Want to ensure best experience possible Considerations: -some women may be very stoic during labor others very vocal -fathers may or may not be present -may prefer alternate positions for deliver such as squatting -may prefer or request female caregiver Uterine Contractions Contractions Duration is from the beginning of a contraction to the end of the same contraction. Frequency is from the beginning of one contraction to the beginning of the next contraction. Intensity is the strength of the contraction. V- Variable Decel E-Early Decel A-Acceleration L- Late Decel C- Cord Compression H Head - Compression O OK, oxygenated - P Placental Insufficiency - FHR Accelerations FHR-Early decelerations INTERVENTIONS Must take action: Put on oxygen Turn off Pitocin Turn to side Increase IV fluids Call HCP Actions to take for Prolapsed Cord Rapid descent in fetal heart rate Goal is to GET pressure OFF of umbilical cord to restore blood flow Prepare for emergency C-Section