Maternal and Child Nursing
advertisement

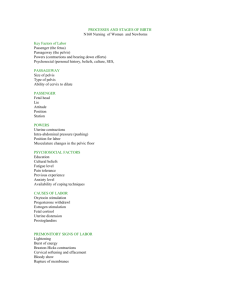
Intrapartum Care Maternal and child Nursing NUR 362 Lecture 7 Intrapartum care Intrapartum period extends from the beginning of contractions that cause cervical dilatation to the first 1 to 4 hours after delivery of the newborn and placenta. Factors affecting the intrapartum experience Experience Culture Prepregnant health & biophysical preparedness for childbearing Motivation for childbearing Socioeconomic readiness Age of mother Phenomena and process of labor and delivery Onset of labor labor is the process by which the fetus and products of conception are expelled as the result of regular ,progressive frequent and strong uterine contractions. Theoretically ,labor is thought to result from: a- progesterone depriviation. b- oxytocin stimulation. c- fetal endocrine control. d- Uterine decidua activation Factors affecting labor 1-passageway: The adequacy of the pelvis and birth canal allowing fetal descent 2-passenger: refer to the fetus Size of fetal head. Fetal presentation. Fetal position. Fetal attitude-the relationship of fetal parts to one another Fetal presentation-the part of the fetus that enters the maternal pelvis first. Fetal position Factors affecting labor 3- power: Frequency, duration and strength of the uterine contractions to cause complete cervical effacement and dilatation. 4-placental factors.-site of placenta. 5-Psyche: client’s psychological state Signs and symptoms of impeding labor 1-lightening: The descent of the fetus and uterus into the pelvis cavity 2 to 3 weeks before the onset of labor. Signs and symptoms of impeding labor 2-Braxton Hicks contractions: Irregular ,intermittent contractions that have occurred throughout the pregnancy ,become uncomfortable and produce a drawing pain in the abdomen. Signs and symptoms of impeding labor 3-Cervical changes: include softening 4-Rupture of the amniotic membrane 5-Burst of energy or increased tension and fatigue. 6- weight loss: about 1 to 3 pounds may occurs 2 to 3 days before the onset of labor. True and false labor False labor -contractions may be irregular. True labor -regular contractions -decrease in frequency and intensity. -progressive frequency and intensity. -longer interval between contractions. -shorter interval between contractions. -activity has no effect or decrease contractions -activity increase contractions. False Contractions -disappear while sleeping. -sedation decrease or stop contractions. -bloody show usually not present. -no appreciable changes in the cervix. True contractions -continue while sleeping. -sedation does not stop contractions. -bloody show usually present. -progressive thinning and opening of the cervix. Stages of labor 1-First stage. begins with the onset of regular contractions. Latent phase: dilation of cervix to3 to 4 cm. contraction become increasing Active phase: dilation continues from 3 to 4 cm to 7 cm. Contraction become stronger and painful Transition phase: cervix dilates from 8 to 10 cm Stages of labor 2- Second stage. (expulsive stage)-begins with complete dilatation of the cervix and ends with delivery of the newborn. -it should be complete within one hour after complete dilatation. Cont, second stage -Movements.. 1. descent. 2. flexion. 3. internal rotation. 4. extension. 5. external rotation. 6. expulsion. Cont, second stage -”crowning” occurs when the newborns head or presenting part appears at the vaginal opening. -”Episiotomy” surgical incision in the perineummay be done to facilitate delivery and avoid laceration of the perineum. 3-Third stage (placental stage) -This stage begins with delivery of the newborn and ends with delivery of placenta. -It occurs in two phases –placental separation and placental expulsion. 4-Fourth stage -It lasts from 1 to 4 hours after birth. -the mother and the newborn recover from physical process of labor. -systems readjustment. Newborn body systems begins to adjust to extrauterine life. -Intrapartum pain experience. -overview of pain. -factors affecting perception of intrapartum pain. -physiologic causes of intrapartum pain. -uterine anoxia. -compression of the nerve ganglia in the cervix. -stretching of the cervix. -traction on, stretching of the perineum. -pressure on the urethra, bladder and rectum during fetal descent. -distension of the lower uterine segment. - Intrauterine pain management -overview of goals. -none pharmacologic pain management. -pharmacological pain management. -narcotic analgesics. -barbiturates. -tranquilizers. -regional anesthesia. - general anesthesia.