Lymphatic System and Immunity Chapter 16
advertisement
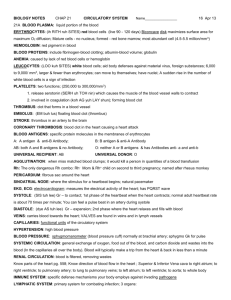
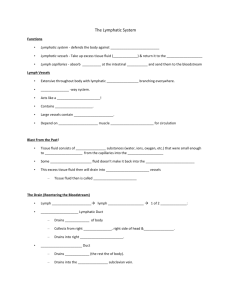
Lymphatic System and Immunity Chapter 16 Functions of Lymphatic System 1. Draining interstitial fluid 2. Transporting dietary lipids 3. Protection Lymphatic Vessels • Begin as closed ended lymph capillaries in tissue spaces between cells • NOT A CIRCULATING FLUID • Interstitial fluid drains into lymphatic capillaries, forming lymph. • Lymph capillaries merge to form lymphatic vessels Lymphatic vessels carry lymph into and out of lymph nodes • • and finally back to the vascular system. Lymphatic capillaries • Made of a single layer of squamous epithelial cells • Slightly larger than blood capillaries • Cells overlap and act as one-way valves • Opened by pressure of interstitial fluid • Anchoring filaments attach cells to surrounding tissue Lymphatic vessels • Resemble veins (same 3 layers) • Found throughout body except: – Avascular tissues – Central nervous system – Splenic pulp – Bone marrow Lymphatic vessels join to form lymphatic trunks. Lymphatic trunks join to form : Thoracic duct (3/4 of body) Right lymphatic duct (drains right arm, and right side of head, neck and upper torso) These empty into subclavian veins at junction with internal jugular vein. Formation of lymph: Fluid leaves capillaries by diffusion and filtration Escaped proteins If lymph flow blocked = tissue swelling or edema Specialized lymphatic capillaries in vili of small intestine transport lipids - they are called lacteals, and the fluid is called chyle. Lymphatic Organs • • • • • Red bone marrow Thymus gland Lymph nodes Lymph nodules Spleen Primary organs Secondary organs Lymph Nodes • • • • • Lymph is filtered through lymph nodes Found in clusters “Waste water treatment plants” Vary in size Principal groupings in cervical, axillary and inguinal regions. • Provide biological filtration • Site of cancer growth and metastasis • Vessels enter node on convex side • Lymph passes through irregular channels called sinuses • Leaves node through one or two efferent vessels at the hilum or hilus • Capsule, cortex and medulla • Cortex contains lymph nodules • Follicular dendritic cells • Germinal centers – B cells proliferate Lymph nodules are also found singly or in groups throughout the mucous membranes of the respiratory, urinary, reproductive and digestive tracts. MALT – mucosa associated lymphoid tissue Peyer’s patches in ileum Tonsils Some in appendix Tonsils – lymphoid tissue under the mucous membranes of the throat palatine tonsils pharyngeal tonsil – adenoid lingual tonsils First line of defense Tonsillectomy Thymus gland • in mediastinum above the heart • largest at age 10-12 then begins to atrophy • Pre - T cells come from bone marrow and develop into T cells • T cells then go to other lymphatic tissues • Thymus produces hormone thymosin - aids maturation of T cells elsewhere in body Spleen • • • • Largest lymphoid organ In upper left quadrant of abdomen Has a hilum and a capsule Sinuses contain blood instead of lymph White pulp: little islands, mostly B cells Red pulp: Venous sinuses Splenic cords – RBCs, macrophages, lymphocytes, plasma cells and granulocytes Functions of Spleen • Blood formation – – All blood cells in fetus – Only lymphocytes and monocytes after birth • Blood filtration – Removes bacteria, particles, worn out RBCs and platelets (recycles iron) • Blood storage – Can contain over one pint of blood Nonspecific Resistance The ability to ward off disease is called resistance. Lack of resistance is susceptibility. Nonspecific resistance refers to a wide variety of body responses against a wide range of pathogens. A pathogen is any microorganism that causes disease. Immunity Immunity involves activation of specific lymphocytes to combat a specific foreign agent. Nonspecific Resistance Species (Inborn) Resistance – certain species contract certain diseases, while other species do not. Mechanical Barriers • Skin and mucous membranes : – – – – – – – First line of defense Physical barrier Shedding of dead cells Mucus Hairs Cilia Coughing and sneezing, production of tears, saliva, urine, defecation and vomiting physically remove harmful substances Chemical Protection Sebaceous glands produce sebum – fatty acids inhibit growth of bacteria and fungi Lactic acid further decreases skin pH Accumulation of salt Vaginal secretions are also slightly acidic Gastric juice – acid, enzymes and mucus Lysozyme in tears, perspiration, saliva and tissue fluids Normal Microbiota – bacteria living on skin inhibit the growth of pathogens by producing antibiotics Antimicrobial Substances Transferrins are proteins that tie up the free iron in the blood and interstitial fluid. Interferon – “Paul Revere Chemical” – a glycoprotein produced by virus infected cells that cause neighboring cells to produce anti-viral proteins. These also enhance phagocytosis and can suppress growth of tumor cells. The Complement System: 10- 20 normally inactive proteins When activated, they “complement” or enhance certain immune, allergic and inflammatory reactions. 1.Activation of inflammation 2. Opsonization – enhances phagocytosis 3.Cytolysis – membrane attack complex Fever : Causes liver and spleen to sequester iron Increases phagocytosis Inhibits growth of microbes Speeds up body repair Inflammation: Characterized by: Heat, swelling, redness, and pain (and sometimes loss of function) calor, tumor, rubor and dolor Stages of inflammation 1. Vasodilation and increased permeability of blood vessels 2. Phagocyte migration 1. Neutrophils come first 2. Followed by macrophages 3. Tissue Repair Phagocytosis Three phases: 1. Chemotaxis 2. Adherence 3. Ingestion Natural Killer Cells • Next line of defense (with phagocytes) • Lymphocytes – but do not respond to specific antigens • Can kill a variety of microbes plus tumor cells. • May release perforins, or attack directly • Cell may not display correct MHC antigens Immunity • Specific resistance to disease involving the production of a specific lymphocyte or antibody against a specific antigen. • An antigen is any substance that elicits an immune response. Best antigens are: – Large – Complex – Recognized as foreign Haptens are molecules that are small, foreign and complex. To elicit an immune response, they must piggy-back on a larger molecule, often blood proteins. Epitopes: a foreign protein may result in several different antibodies. Each antibody recognizes a different portion of the protein. These regions are called epitopes. Two forms of immunity: Humoral or antibody mediated immunity B cells (mature in bone) make antibodies: specific proteins that bind to specific antigens OR Cell-mediated immunity Tcytoxic lymphocytes attack virus infected or tumor cells directly “The Story” • Macrophage destroys a bacterium • Takes bacterial antigen and fuses it with MHC II complex • MHC II complex and antigen are placed on cell membrane. • Displays antigen (like a proud cat) – so it is called an antigen presenting cell. It shows antigen to helper T cells, until it finds one that has a receptor that matches the antigen complex. The helper T cell binds to the antigen complex, and the macrophage is stimulated to produce the cytokine Interleukin -1 A cytokine is a protein hormone which regulates normal cell functions, like growth and differentiation. Every step needs 2 signals to proceed. IL-1 binds to receptors on the helper T cell, causing helper T-cell to clone itself and produce IL-2. IL-2 causes lymphocytes to multiply. These steps are common to both humoral and cell-mediated immunity. Humoral or Antibody mediated immunity In order for B cells to become activated and make antibodies against an antigen, two things must happen: 1. B cell must encounter the antigen 2. IL-2 produced by helper T cell must be present. When both signals are present (the antigen and IL-2). The B cell becomes activated and forms two types of cells: plasma cells and memory cells. Plasma cells produce large quantities of their specific antibody into the blood. Memory cells lie in wait for the next infection. Antibodies “Y” shaped proteins – gamma globulins have a variable region that matches a specific antigen (Fab region) Have a constant region – activates complement (Fc region) The first antibodies produced are IgM. Pentamers – with ten combining sites – very effective in opsonization and activating complement Several days later, IgG is produced – single unit antibodies, abundant in serum, cross the placenta, and have the longest half-life. Cell mediated immunity A virus is a core of nucleic acid wrapped in a protein. To reproduce, it must make use of a host cell to replicate the viral nucleic acids and proteins and assemble new viruses. Infected cells put viral proteins on their membranes. This antigen is processed by macrophages. Antibodies can’t get at viruses inside a cell, so we need something different : a Tcytotoxic or Tc Cell. The Tc encounters the viral antigen with the MHC -1 complex on the infected cell. Now needs the second stimulus – IL-2 from the helper T cell. Tc cell clones itself, and makes activated Tc cells and memory cells. Tc Cells bind to antigens on infected cells and release: Perforins – punch holes in cell membrane. Lymphotoxins- activate the cell’s own selfdestruct mechanism Tc Cells are effective against bacteria which are intracellular parasites, viruses, fungi, cancer cells associated with viral infections, and transplanted cells. Immune Response The first time you encounter an antigen, you have few B cells or Tc cells against that antigen = primary response The next time, you have many memory cells, so response is much quicker, so you don’t come down with the disease = secondary response HIV/AIDS Human immunodeficiency virus Attacks helper T cells Without production of IL-2, there is no second signal, and humoral and cell mediated immunity are shut off. See increase in rare diseases: TB, Kaposi sarcoma, etc. Hypersensitivity “The immune system gone bad.” Delayed Hypersensitivity A type of cell mediated immunity. Td cell – requires usual two signals Second time antigen is encountered, Td cell produces several cytokines that attract and activate macrophages, resulting in an inflammatory reaction. Examples: poison ivy (urushiol), TB skin test Immediate Type Hypersensitivity • Exposure to certain antigens (allergens) results in the formation of IgE antibodies • IgE antibodies bind to mast cells by the Fc end. • When the antigen is encountered again, binding with the antibody causes mast cell to release histamine granules. May be able to desensitize individual by giving allergen to stimulate IgG antibodies. These tie up antigen before they can bind with IgE. Acquired immunity Active = person makes own antibodies Passive = person receives antibodies from someone else Natural = “just happens” Artificial = caused by man (often using a needle) Natural active acquired immunity: person comes down with measles Artificial active acquired immunity: person is immunized with a vaccine Artificial passive acquired immunity: Person receives serum with antibodies Natural passive acquired immunity: Baby receives antibodies with mother’s milk - colostrum