nerve cells
advertisement

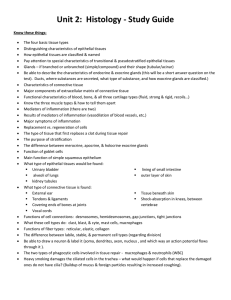
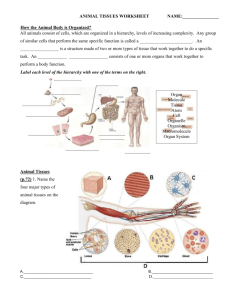
Chapter 5: Histology 1 INTRODUCTION Tissue: group of similar cells that perform a common function Matrix: nonliving intercellular material 2 PRINCIPAL TYPES OF TISSUE Epithelial tissue (Table 5-1) Connective tissue Muscle tissue Nervous tissue Embryonic development of tissues Primary germ layers • Endoderm • Mesoderm • Ectoderm Histogenesis: process of the primary germ layers differentiating into different kinds of tissue 3 EXTRACELLULAR MATRIX Extracellular matrix (ECM) is a complex, nonliving material between cells in a tissue (Figure 5-1) Some tissues have a large amount of ECM; other tissues have hardly any Different kinds of components give ECM in different tissues a variety of characteristics 4 5 EXTRACELLULAR MATRIX (cont.) Components (Table 5-2) Water Proteins • Structural proteins Collagen: strong, flexible protein fiber Elastin: elastic fibers • Includes glycoproteins: proteins with a few carbohydrate attachments Fibronectin and laminin help connect the ECM components to cells by binding with integrins in plasma membranes Glycoprotein attachments also allow local communication within a tissue 6 EXTRACELLULAR MATRIX (cont.) Proteoglycans • Hybrid molecules that are mostly carbohydrates attached to a protein backbone • Examples: chondroitin sulfate, heparin, and hyaluronate • Different proteoglycans give different characteristics to ECM, such as thickness and shock absorption (Table 5-2) 7 EXTRACELLULAR MATRIX (cont.) Functions Helps bind tissues together structurally • ECM components bind to each other and to integrins in plasma membranes of cells • Some tissues are held together primarily by intercellular junctions Allows local communication among ECM and various cells through connection with integrins in plasma membranes 8 Major Types of Tissues (4) Epithelial tissue Connective tissue ie: Bones, joint cartilage, tendons and ligaments, blood and fat Muscle tissue ie: outer layer of skin; lining of respiratory digestive, urinary and reproductive tracts as well as glands of the body. ie: Heart, skeletal and smooth mm. Nervous tissue ie: CNS, PNS and sensory organs of the body 9 EPITHELIAL TISSUE Types and locations Epithelium is divided into two types: • Membranous (covering or lining) epithelium • Glandular epithelium Locations • Membranous epithelium: covers the body and some of its parts and lines the serous cavities; blood and lymphatic vessels; and respiratory, digestive, and genitourinary tracts • Glandular epithelium: secretory units of endocrine and exocrine glands 10 EPITHELIAL TISSUE (cont.) Functions Protection Sensory functions Secretion Absorption Excretion 11 EPITHELIAL TISSUE (cont.) Generalizations about epithelial tissue Limited amount of matrix material Membranous type attached to a basement membrane Avascular Cells are in close proximity, with many desmosomes and tight junctions Capable of reproduction UNDERGOES MITOSIS 12 EPITHELIAL TISSUE: MEMBRANOUS Classification of epithelial tissue Membranous (covering or lining) epithelium (Table 5-3) Number of cell layers – Simple vs. Stratified Classification based on cell shape (Figure 5-2) Squamous Cuboidal Columnar Pseudostratified columnar 13 14 Simple Squamous Epithelium Structure: single layer of flat cells Location: simple squamous- lining of blood and lymphatic vessels (endothelium) and small ducts, alveoli of the lungs, loop of Henle in kidney tubules, lining of serous membranes (mesothelium) and inner surface of the eardrum. Functions: diffusion, filtration, some protection against friction, secretion, absorption. 15 Simple Cuboidal Epithelium Locations: Kidney tubules, glands and their ducts, choroid plexus of the brain, lining of terminal bronchioles of the lungs, and surface of the ovaries. Structure: single layer of cube-shaped cells; some types have microvilli (kidney tubules) or cilia (terminal bronchioles of the lungs) Functions: Secretion and absorption in the kidney Secretion in glands and choroid plexus Movement of mucus out of the terminal bronchioles by ciliated cells. 16 Simple Columnar Epithelium Location. Glands and some ducts, bronchioles of lungs, uterine tubes, stomach, intestines, gallbladder, bile ducts and ventricles of the brain. Structure: single layer of tall, narrow cells. Some have cilia (bronchioles of lungs, auditory tubes, uterine tubes, and uterus), microvilli (intestine) or goblet cells. Functions: Movement of particles out of the bronchioles by ciliated cells Aids in the movement of oocytes through the uterine tubes by ciliated cells Secretion by glands of the stomach and the intestine Absorption by cells of the intestine. 17 Stratified Squamous Epithelium Locations: Moist- mouth, throat, larynx, esophagus, anus, vagina, inferior urethra, and cornea Keratinized- skin Structure: multiple layers of cells that are cuboidal in the basal layer and progressively flatten toward the surface. In moist, surface cells retain a nucleus and cytoplasm. In keratinized, surface cells are dead. Functions: protection against abrasion, caustic chemicals, water loss, and infection. 18 Stratified Cuboidal Epithelium Locations: sweat gland ducts, pharynx and salivary gland ducts Structure: multiple layers of somewhat cube-shaped cells. Functions: secretion, absorption and protection against infections. 19 Stratified Columnar Epithelium Locations: rare in the body, mammary gland duct, larynx, portion of male urethra. Structure: multiple layers of cells with tall thin cells resting on layers of more cuboidal cells. Cells ciliated in the larynx. Function: protection and secretion. 20 Pseudostratified Columnar Epithelium Locations: air passages: lining of nasal cavity, nasal sinuses, auditory tubes, pharynx, trachea, and bronchi of lungs; male reproductive system Structure: all cells reach basement membrane. Appears stratified because nuclei are at various levels. Almost always ciliated and associated with goblet (mucus-producing) cells. Functions: Synthesize and secrete mucus onto the free surface (goblet cells) Move mucus (or fluid) that contains foreign particles over the free surface and from passages (cilia) 21 Transitional Epithelium Location: lining of urinary bladder, ureters and superior urethra. Structure: stratified; cells change shape depending upon amount of distention of the organ. Functions: accommodates fluctuations in the volume of fluid in an organ or tube; protection against the caustic effects of urine. 22 EPITHELIAL TISSUE: GLANDULAR EPITHELIUM Glandular epithelium • Specialized for secretory activity • Exocrine glands: discharge secretions into ducts and lead to the exterior of the body • Endocrine glands: “ductless” glands; discharge secretions directly into blood or interstitial fluid 23 EPITHELIAL TISSUE: GLANDULAR EPITHELIUM (cont.) • Structural classification of exocrine glands (Figure 511; Table 5-5) Multicellular exocrine glands are classified by the shape of their ducts and the complexity of their duct system Shapes include tubular and alveolar Simple exocrine glands: only one duct leads to the surface Compound exocrine glands: have two or more ducts 24 25 EPITHELIAL TISSUE: GLANDULAR EPITHELIUM (cont.) • Functional classification of exocrine glands (Figure 5-12) Apocrine glands – Secretory products collect near apex of cell and are secreted by pinching off the distended end – Secretion process results in some damage to cell wall and some loss of cytoplasm – Mammary glands are good examples Holocrine glands – Collect secretion products within the cell, rupture to release causing death of the cell – Sebaceous glands are holocrine Merocrine glands – Secrete directly through cell membrane – Secretion proceeds with no damage to cell wall and no loss of cytoplasm – Most numerous gland type – Salivary glands 26 27 CONNECTIVE TISSUE Functions, characteristics, and types General function: connects, supports, transports, and protects General characteristics extracellular matrix (ECM) predominates in most connective tissues and determines its physical characteristics; consists of fluid, gel, or solid matrix, with or without extracellular fibers (collagenous, reticular, and elastic) and proteoglycans or other compounds that thicken and hold together the tissue (Figures 5-1 and 5-14) 28 Composition of Extracellular Matrix: Fibers Protein fibers Collagen. Most common protein in body; strong, flexible, inelastic Reticular. Fill spaces between tissues and organs. Fine collagenous, form branching networks Elastic. Returns to its original shape after distension or compression. Contain molecules of protein elastin that resemble coiled springs; molecules are cross-linked 29 CONNECTIVE TISSUE (cont.) Four main types (Table 5-6) • Fibrous Loose (areolar) Adipose Reticular Dense – Irregular – Regular (collagenous and elastic) • Bone Compact bone Cancellous bone • Cartilage Hyaline Fibrocartilage Elastic • Blood 30 Functions of Connective Tissue Enclose organs as a capsule and separate organs into layers Connect tissues to one another. Tendons and ligaments. Support and movement. Bones. Storage. Fat. Cushion and insulate. Fat. Transport. Blood. Protect. Cells of the immune system. 31 Adult Connective Tissues Loose (areolar). Collagenous fibers are loosely arranged Dense. Fibers form thick bundles that nearly fill all extracellular space Dense regular Dense irregular With special properties Cartilage Bone Blood and hemopoietic tissue 32 Loose (Areolar) Connective Tissue Most widely distributed of all tissues Loose packing material of most organs and tissues Attaches skin to underlying tissues. Contains collagen, reticular, elastic fibers Cells include fibroblasts (make ground substance), mast cells (release histamine to produce an inflammation response), adipose cells, macrophages Soft gel matrix due to hyaluronic acid 33 Connective Tissue Adipose tissue (Figures 5-17 and 5-18) Similar to loose connective tissue but contains mainly fat cells (adipocytes) Functions—protection, insulation, support, and food reserve 34 Connective Tissue Reticular tissue (Figure 5-19) Consists of network of branching reticular fibers with reticular cells overlying them Forms framework of spleen, lymph nodes, and bone marrow Functions—defense against microorganisms and other injurious substances; reticular meshwork filters out injurious particles, and reticular cells phagocytose them 35 Dense Irregular FibrousTissue Bundles and sheets of collagenous and elastic fibers oriented in multiple directions Strong, can withstand stress Dermis, fascia surrounding muscles,encapsulates organs 36 Dense Regular Collagenous Fibrous Connective Tissue Collagenous: tensile strength Tendons: Connect muscles to bones; fibers are not necessarily parallel Elastic: more stretch Ligaments: Connect bones to bones. Collagen often less compact, usually flattened, form sheets or bands Arteries – recoil and stretch depending on blood pressure 37 Connective Tissue Bone tissue Highly specialized connective tissue type • Cells—osteocytes—embedded in a calcified matrix • Inorganic component of matrix accounts for 65% of total bone tissue and add hardness Functions: • • • • • Support Protection Point of attachment for muscles Reservoir for minerals Supports blood-forming tissue 38 Connective Tissue Compact bone (Figures 5-25 and 5-26) Osteon (Haversian system) • Structural unity of bone • Spaces for osteocytes called lacunae arranged in concentric rings called lamellae • Canaliculi are canals that join lacunae with the central Haversian canal Cell types: • Osteocyte—mature, inactive bone cell • Osteoblast—active, bone-forming cell • Osteoclast—bone-destroying cell 39 Connective Tissue Cancellous bone (Figures 5- 25 and 5-27) Trabeculae—thin beams of bone which form framework Supports red bone marrow • AKA Myeloid tissue—a type of reticular tissue • Produces blood cells Called spongy bone because of its spongelike appearance 40 Cartilage Composed of chondrocytes located in matrix-surrounded spaces called lacunae. Type of cartilage determined by components of the matrix. Firm consistency. Avascular and no nerve supply. Heals slowly. Perichondrium. Membrane which surrounds cartilage which allows diffusion of nutrients. Types of cartilage Hyaline Fibrocartilage Elastic 41 Hyaline Cartilage Structure: low amount of collagen fibers evenly distributed in proteoglycan matrix. Smooth surface in articulations Locations: Found in areas for strong support and some flexibility: rib cage, trachea, and bronchi In embryo forms most of skeleton Covers ends of bones which articulate to form joints 42 43 Fibrocartilage Strongest and most durable Shock absorption; slightly compressible and very tough Locations: found in areas of body where a great deal of pressure is applied to joints Knee, jaw, between vertebrae 44 Elastic Cartilage Structure: elastic and collagen fibers create flexibility, rigid but elastic properties Locations: external ears, larynx and epiglottis 45 Blood Matrix: plasma 55% Liquid and lacks fibers. Formed elements 45%: red cells (erythrocytes), white cells (leukocytes), and platelets (thrombocytes) Movement of respiratory gases,nutrients and waste, constant body temp, regulates pH Hematopoietic tissue Forms blood cells Two types of bone marrow • Yellow • Red 46 Muscle Tissue 47 Skeletal Muscle Voluntary, striated,multinucleate, long nonbranching cylindrical cells 48 Cardiac Muscle Involuntary, striated, uninucleate, branched cells, intercalated discs 49 Smooth Muscle Involuntary, uninucleate, spindle shaped, found in lumen 50 Nervous Tissue Functions—rapid regulation and integration of body activities Organs Brain Spinal cord Nerves - neurons -neuroglia 51 Nervous Tissue: Neurons Neurons or nerve cells have the ability to produce action potentials Parts: • Cell body (soma): contains nucleus • Axon: cell process; conducts impulses away from cell body; usually only one per neuron • Dendrite: cell process; receive impulses from other neurons; can be many per neuron 52 Support cells of the brain, spinal cord and nerves Nourish, protect, and insulate neurons Types -astrocytes form BBB -microglia – destroy pathogens -oligodendrocytes – insulate nerve cells to increase conduction speed Neuroglia 53 TISSUE REPAIR Tissues have a varying capacity to repair themselves; damaged tissue regenerates or is replaced by scar tissue Regeneration: growth of new tissue (Figure 5-36) Scar: dense, fibrous mass; unusually thick scar is a keloid (Figure 5-37) Epithelial and connective tissues have the greatest ability to regenerate Muscle and nervous tissues have limited capacity to regenerate 54 Body Membranes Thin tissue layers that cover surfaces, line cavities, and divide spaces or organs (Figure 5-39, Table 5-8) Epithelial membranes are most common type (Figure 5-40) Cutaneous membrane (skin) • Primary organ of integumentary system • One of the most important organs • Composes approximately 16% of body weight, largest organ Serous membrane (serosa) • • • • Parietal membranes—line closed body cavities Visceral membranes—cover visceral organs Pleura—surrounds a lung and lines the thoracic cavity Peritoneum—covers the abdominal viscera and lines the abdominal cavity • Pericardium – surrounds heart 55 Body Membranes • Mucous membrane (mucosa) Lines and protects organs that open to the exterior of the body Found lining ducts and passageways of respiratory, digestive, other tracts Lamina propria—fibrous connective tissue underlying mucous epithelium Mucus is made up mostly of water and mucins—proteoglycans that form a double-layer protection against environmental microbes (Figure 5-41) Connective tissue membranes • • • • • Do not contain epithelial components Synovial membranes—line the spaces between bone in joints Have smooth and slick membranes that secrete synovial fluid Help reduce friction between opposing surfaces in a moveable joint Synovial membranes also line bursae 56