Blood vocab
advertisement

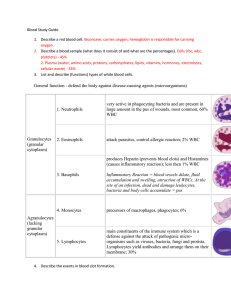
Hematopoiesis Blood cell formation that occurs in the red bone marrow found in flat bones (skull, pelvis, ribs, sternum, proximal epiphyses of the humerus and the femur. Erythropoietin (EPO) Hormone that controls rate of erythrocyte (RBC) production Is produced by the kidneys Targets the bone marrow Formed Elements Accounts for 45% of whole blood Erythrocytes Leukocytes Platelets Plasma Liquid portion of the blood – accounts for 55% of whole blood Is 90% water Helps to distribute body heat evenly Albumin Is a plasma protein Regulates osmotic pressure of blood Helps to keep water in the bloodstream Megakaryocytes Fragments of bizarre multinucleate cells They rupture and release thousands of pieces that seal off from surrounding fluids Platelets Are needed for the clotting process Formerly called thrombocytes (platelets) Thrombus A clot that develops in an unbroken blood vessel Embolus When a clot (thrombus) breaks away from a blood vessel and floats freely in the bloodstream Potentially life threatening Hematocrit The volume of a blood sample Leukocytes White Cells Are White Blood Cells (WBC’s) Protect, defense, immunity Account for less than 1% of total blood volume Are complete blood cells: contain nuclei and organelles Diapedesis Means “leaping across” WBC’s are able to slip in and out of blood vessels as needed Leukocytosis An increased white blood cell count Could be indicative of a bacterial or viral infection Leukopenia Abnormally low WBC count Commonly caused by certain drugs, and anticancer medications Granulocytes Contains granules (appears as grains of sand) Are “philled” with sand Types: Neutrophils Eosinophils Basophils Neutrophils Act as avid phagocytes at site of acute infections Eosinophils Kills parasitic worms Tend to increase during allergies Basophils Rarest form of WBC’s Contains histamines at sites of inflammation Agranulocytes Lack visible organelles Include: lymphocytes and monocytes “are a “cyte” for sore eyes” Lymphocytes Part of the immune system Reside in lymphatic tissues Monocytes Are the largest WBC Change into macrophages Help fight chronic infections Erythrocytes Red Blood Cells (RBC’s) Are anucleate Have few organelles No mitochondria Have biconcave disks for increased surface area for Oxygen/Carbon Dioxide Polycythemia Excessive or abnormal increase in RBC’s May result from: 1) bone marrow cancer 2) High altitudes Leads to increase viscosity, sluggish flow Hemoglobin (Hb) Is an iron containing protein Transports oxygen Also binds with CO2 250 million HB molecules in 1 RBC Normal levels 12-18g/100ml of blood Males: 13-18g; Females: 12-16g ABO Blood Groups 2 Antigens (A or B) inherits one or the other, both or none Absence of both antigens = Type O Presence of both = Type AB Either A or B if just one antigen present AB type is universal recipient O type is universal donor Agglutination Binding of the antibodies causing RBC’s to clump Leads to clogging of small blood vessels Antigens Is recognized as “foreign” Stimulates release of antibodies from the immune system Over 30 common RBC antigens Disorders of the clotting process Undesirable Clotting Thrombus embolus Bleeding disorders Thrombocytopenia – is a platelet deficiency Hemophilia – lack Pf factors for clotting Hemophilia Hereditary bleeding disorder “bleeder’s disease” Patients are given fresh plasma or injections of missing platelet factor (Pf) Hemostasis Hem = blood Stasis = standing still Means stoppage of blood flow Heparin Body’s natural anticoagulant Coagulation To clot Fibrin Is converted from fibrinogen to fibrin Is an insoluble protein formed during blood clotting process Process of Blood Clotting Is a multistep process: 1. Vascular spasms – of the smooth muscle in the vessel wall producing a vasoconstriction resulting from serotonin. Lasts up to 30 minutes Makes the platelets “sticky” as they are produced Process of Blood Clotting 2. Platelet plug forms – damaged blood vessel releases Von Willebrand’s Factor. Platelets release ADP causing aggregation and a plug to form An increase in the “stickiness” results Process of Blood Clotting 3. Coagulation (clotting phase) Platelet Factor III (PF3) releases thromboplastin. PF3 and Calcium forms an activator producing a cascade effect. Prothrombin (in the plasma) is converted to Thrombin (an enzyme) Formation of Fibrinogen (plasma protein) to Fibrin to trap platelets “meshwork.” Process of Blood Clotting Entire process normally takes 3 – 6 minutes A sudden and severe loss of blood leads first to shock and eventually death Use direct pressure to help Elevate body part above the heart to allow gravity to take effect 3 phases of hemostasis (process of blood clotting): •Vascular spasms – decreases the flow of blood to the area •Platelet plug formation – platelets become “sticky” and cause chemical release to form clot •Coagulation – prothrombin to thrombin and fibrinogen to fibrin http://www.mhhe.com/biosci/es p/2002_general/Esp/folder_stru cture/tr/m1/s7/trm1s7_3.htm