14 Unit 1 - Saratoga High School
advertisement

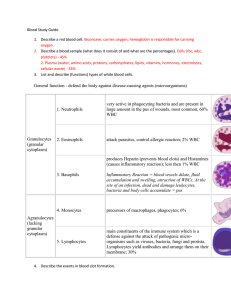
The Cardiovascular System: 14 Blood Unit 1 Chapter 14 Function 14 • 3 components of the cardiovascular system = blood, heart, blood vessels • Function of CV system = transports substances to and from body cells • Hematology = branch of science that deals with study of blood, bloodforming tissues and disorders associated with them Unit 1 • Is a type of connective tissue • Transportation- gasses (O2 & CO2), nutrients (GI tract), heat & waste, hormones (endocrine system) • Regulation- pH, temperature, water balance in cells • Protection- loss of blood via clotting, WBC vs. disease; production of 14 Unit 1 Functions of Blood •5 1. 2. 3. 4. 5. facts about blood Blood is thicker than water Temp is 38° C Slightly alkaline 7.35 – 7.45 8% of total body weight Volume = males – 5-6 liters females – 4-5 liters 14 Unit 1 Components • Connective tissue-Two parts • Plasma = straw-colored liquid with dissolved materials (~55%) • Formed Elements = cells and cells fragments (~45%) 99% of the formed elements are RBCs 14 Unit 1 Composition Composition 14 • Buffy coat – part made up by white blood cells (WBC) and plateletes ~1% Unit 1 • hematocrit (Hct) = Percent of blood volume occupied by red blood cells (RBC) Figure 14.1a Figure 14.1b • ~91% water, 7% proteins, 1.5 % other solutes • Proteins: Albumin (54%)- maintains osmotic pressure; • Globulins (38%)- antibodies for defense • Fibrinogen (7%)- clotting • Other solutes in plasma: Electrolytes , nutrients, gases, hormones, vitamins & waste products 14 Unit 1 Plasma Formed Elements 14 I. Red Blood Cells II. White blood cells A. granular Leukocytes 1. Neutrophils 2. Eosinophils 3. Basophils 1. T & B lymphocytes & natural Killer cells 2. monocytes III Platelets Unit 1 B. Agranular leukocytes • Hemopoiesis – production of formed elements • 3 months before birth and throughout life occurs in red bone marrow • Contains pluripotent stem cells • In response to specific hormones these develop through a series of changes to form all of the blood cells 14 Unit 1 Formation of Red Blood Cells Formation of Red Blood Cells 14 Unit 1 • Bone marrow contains pluripotent stem cells – cells that can develop into many different types of cells • In response to specific hormones these develop into myeloid stem cells (RBC, platelets, and some WBC) and lymphoid stem cells (T and B lymphocytes) Figure 14.2a Figure 14.2b Red Blood Cells 14 • AKA = Erythrocytes • Contains - hemoglobin proteincarries oxygen • Male has ~ 5.4 million cells/µl; Female has ~4.8 million Unit 1 Also carries some CO2 Erythrocytes (RBCs) 14 • Production rate = 2 million/sec • Contain no nucleus & other organelles • Consists of membrane, cytosol, hemoglobin • Biconcave shape provides for greater surface area for the diffusion of gas molecules into/out of a RBC Unit 1 • Wear out fast- live ~120 days due to wear and tear as they squeeze through capillaries • Worn out and ruptured cells are cleared by macrophages (liver spleen, red bone marrow) • Fe- recycled in bone marrow Carried in blood on transferrin – plasma protein acts as a transporter for iron 14 Unit 1 RBC Cycling • biliverdin bilirubin – what the non-iron portion of heme is converted into and excreted (bile) • Urobilinogen and stercobilin – by products of bilirubin; some absorbed in large intestine; ultimately excreted in urine or feces 14 Unit 1 RBC Cycling Figure 14.3 RBC Production 14 • called erythropoiesis • Released as reticulocytes (almost a RBC) • Production & destruction is balanced Unit 1 Mature to erythrocytes in 1-2 days • If O2 carrying capacity falls, RBC productions is inc. by a negative feedback loop • Low O2 delivery (hypoxia) • erythropoietin (EPO)- kidney hormone stimulates erythropoiesis 14 Unit 1 RBC Synthesis • Cyanosis – life threatening condition caused by prolonged hypoxia; bluish-purple skin coloration • Anemia – reduced O2 carrying capacity – reduced # of RBC or ↓ amount of hemoglobin in blood; pale skin 14 Unit 1 RBC Synthesis Figure 14.4 • aka = leukocytes • Classified as either 1. granular which contains a chemical filled cytoplasmic granule/vesicle (neutrophils, eosinophils, basophils) or 2. agranular (lymphocytes, monocytes) • Function in defense: phagocytosis or antibody production 14 Unit 1 White Blood Cells 14 White Blood Cells • Phagocytes: Unit 1 Neutrophil- first responders; release lysozomes that destroy bacteria Monocytes slower response; become wandering macrophages (big eaters compared to neutrophils) Eosinophil- work in interstitial fluid; Involved in suppressing allergic responses; phagocitize antibody-antigen complexes and are effective against some parasitic worms Basophil- intensify allergic reactions White Blood Cells 14 • Phagocytes: Unit 1 a. Neutrophil- first responders; release lysozomes that destroy bacteria b. Monocytes slower response; become wandering macrophages (big eaters compared to neutrophils) White Blood Cells 14 d. Basophil- release heparin, histamines, serotonin; intensify allergic reactions Unit 1 • Phagocytes: c. Eosinophil- phagocitize antibody-antigen complexes involved in suppressing allergic responses 14 White Blood Cells • Producing antibodies (Immune response): Unit 1 B-cells – plasma cells – produce antibodies to help destroy bacteria/inactivate toxins T-cells – attack viruses, fungi, cancer cells, transplanted cells, bacterial cells Natural killer (NK) cells – attack infectious microbes and some types of tumor cells White Blood Cells 14 Unit 1 • Major histocompatibility (MHC) antigens – proteins on the surface of a cells that act as “cell identity markers” that are unique for each person; used to type tissue for transplants WBC Life Span 14 • Life span is a few days normally; a few hour during an active infection; some B and T cells live for years Unit 1 • Number of RBC vs. WBC is 700:1; 5000-10,000 WBC /µl blood 14 WBC Life Span Unit 1 • Leukocytosis= normal increase in WBC #’s response to stresses; indicates inflammtion/infection • Differential white blood cell count is the measure of the different types of WBC per 100 WBC (helps in diagnosis) • Leukopenia = abnormally low WBC numbers; never good; radiation, shock, some chemotherapeutic agents Platelets 14 Unit 1 • Myeloid stem cells megakaryoblasts megakaryocytes 2000 -3000 fragments = platelets • Plug damaged blood vessels • Promote blood clotting • Life span 5-9 days Hemostasis 14 • Hemorrhage - loss of large amounts of blood Unit 1 • Hemostasis = stationary blood – a series of responses that stop bleeding when blood vessels are injured 1. Vascular reactions (spasm) 2. platelet plug formation 3. blood clotting (coagulation) • 1. Vascular spasm – contraction of smooth muscle in the walls of a damaged blood vessel; effective for several minutes to several hours; platelets at the site release chemicals to enhance vasoconstriction maintaining vascular spasm Quick reduction of blood loss 14 Unit 1 Hemostasis Hemostasis 14 Unit 1 • 2. platelet plug formation – platelets stick to parts of a damaged blood vessel; they release chemcials to make other platelets sticky; eventually forms a platelet plug Hemostasis 14 • 3. blood clotting –when blood is withdrawn it separates into serum and a gel called fibrin (protein fibers that make up a clots) • Clotting (coagulation) –process of clot formation; series of chemical reactions involving clotting factors • Thrombosis – clotting in an unbroken blood vessel Unit 1 • 1. prothrombinase is formed • 2. prothrombinase converts prothrombin (a protein) thrombin (an enzyme) • 3. thrombin converts fibrinogen (another protein) fibrin (fibers that form the threads of a clot) clot 14 Unit 1 3 Stages of Clotting Prothrombinase Formation 14 • Extrinsic pathway happens quickly; • Intrinsic Pathway takes several minutes Materials “intrinsic” to blood make prothrombinase Unit 1 tissue factor(TF) from damaged cells makes prothrombinase • Clot retraction- consolidation or tightening of the fibrin clot • As the clot retracts damaged edges of blood vessels pull closer together • Permanent repairs take place when fibroblasts form connective tissue and endothelial cells repair the vessel lining 14 Unit 1 Clot Retraction & Vessel Repair Control Mechanisms 14 Unit 1 • Fibrinolysis: dissolving of unnecessary clots by activated plasmin which digests fibrin threads in a clot • Clots can be triggered by 1. Roughness on vessel wall as a result of atherosclerosis, trauma, infection 2. If the flow of blood becomes too slow clotting factors accumulate enough to trigger a clot 14 Unit 1 Clotting in Blood Vessels • Thrombosis - clotting in an unbroken vessel (thrombus = clot) • Blood clot, air bubble, or fat from a broken bone transported by blood= embolus and can block a small blood vessel • Pulmonary embolism – blockage of blood vessel in the lungs 14 Unit 1 Control Mechanisms Figure 14.5 • Agglutinogens – antigens composed of glycolipids/proteins on the surface of RBC • Blood groups are categorized based on the presence or absence of various antigens • >24 blood groups and >100 antigens 14 Unit 1 Blood Group and Types • We will deal with ABO and Rh groups • ABO blood group has two antigens A and B • Your blood type is determined by which you have (if you have the A antigen you have blood type A; AB blood has both the A and B antigen; O has no antigen) 14 Unit 1 Blood Types ABO Group 14 • Blood usually has antibodies or agglutinins that can react with antigens e.g. anti-A antibody or anti-B antibody Thus: type A has anti-B and vice versa Unit 1 • You don’t react with your own antigens Figure 14.6 • The Rh blood group is named after the rhesus monkey where the Rh antigen was discovered • If have antigen you are Rh+ • Normally we don’t have anti-Rh antibodies they develop after the first exposure from transfusion 14 Unit 1 Rh Blood Group • Transfusion – transfer of whole blood or blood components (plasma) • If mismatched blood is given antibodies in the recipient's blood bind to the antigens on the donated RBC and causes hemolysis (rupture of RBC) 14 Unit 1 Transfusions • Universal recipients - Type AB has no AB antibodies so can receive any ABO type blood • Universal donors - Type O have neither antigen so can donate to any other ABO type • Misleading because of many other blood groups that must be matched 14 Unit 1 Transfusions