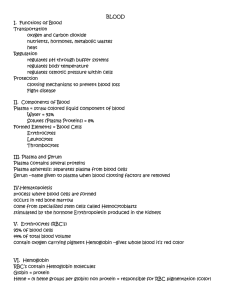
Lecture 11: Cardiovascular System (blood) Functions: Transport of gases, nutrients, and waste products. Transport of processed molecules. Transport of regulatory molecules. Regulation of pH and osmosis. Maintenance of body temperature. Protection against foreign substances. Clot formation. Composition of blood: Liquid matrix (plasma) – 55% Formed elements – 45% o Cells o Cell fragments Total blood volume in adults: Male – 5 – 6 Liters Female – 4 – 5 Liters Plasma It is the liquid matrix of blood. It is a pale-yellow fluid that consists of about 91% water and 9% other substances. Composition of Plasma Water – acts as a solvent and suspending medium for blood components. Plasma Proteins Albumin – partly responsible for blood viscosity and osmotic pressure. Globulins - They are antibodies produced by plasma cells in response to the presence of pathogens like bacteria and viruses. Fibrinogen – Functions in blood clotting. Ions Sodium, Potassium, Calcium, Magnesium, Chloride, Iron, Phosphate, Hydrogen, Hydroxide, Bicarbonate – involved in osmosis, membrane potentials, and acid-base balance. Nutrients Glucose, Amino Acids, Triglycerides, Cholesterol – source of energy and basic “building blocks” of more complex molecules. Vitamins – Promote enzyme activity. Waste Products Urea, uric acid, creatinine, ammonia salts – Breakdown products of protein metabolism; excreted by the kidneys. Bilirubin – Breakdown product of red blood cells; excreted as part of the bile from the liver into the small intestine. Lactate – End product of anaerobic respiration; converted to glucose by the liver. Gases Oxygen – Necessary for aerobic respiration; terminal electron acceptor in electron-transport chain. Carbon dioxide – Waste product of aerobic respiration; as bicarbonate, helps buffer blood. Nitrogen – Inert Regulatory Substances Enzymes catalyze chemical reactions; hormones stimulate or inhibit many body function. Serum Plasma without clotting factors. No fibrogen Formed Elements Consist of cells and cell fragments. The cells include red blood cells and white blood cells. Cell fragments are more commonly called platelets. Production of Formed Elements Hematopoiesis the process of blood cell production. Hemocytoblasts Precursor cells capable of dividing to produce daughter cells that can differentiate into various types of blood cells. Myeloid stem cells Give rise to several intermediate cell types. Proerythroblasts Produce red blood cells Myeloblasts Produce basophils, eosinophils, and neutrophils. Monoblasts Produce monocytes. Megakaryoblasts Produce platelets. Red Blood Cells (RBC) Also called erythrocytes. No nucleus Biconcave disc Normal life span is 120 days Oxygen transport Removal of metabolic waste Hemoglobin Is a complex protein consisting of four subunits. Each subunit is composed of one polypeptide chain called globin that is bound to one heme group. Erythropoiesis The process by which new red blood cells are produced. White Blood Cells (WBC) Also called leukocytes. Have a nucleus. Grouped into two categories based on their appearance in stained preparations: Granulocytes (with granules) o Neutrophils o Eosinophils o Basophils Agranulocytes (without granules) o Lymphocyte o Monocytes Granulocytes Neutrophils 60 – 70% of white blood cells Small cytoplasmic granules Statin with both acidic and basic dyes Normally remain in the circulation for about 10-12 hours. Eosinophils 2 – 4% of white blood cells Stain bright red with eosin, an acidic stain Two-lobed nucleus They attach to the worms and release substances that kill the parasites. Basophils 0.5 – 1% of white blood cells Large granules – stain blue or purple with basic dyes Increase in number in both allergic and inflammatory reactions. Contains large amounts of histamine. Vascular Spasm Immediate but temporary constriction of a blood vessel. Allows platelets to adhere to exposed tissue. ADP/ATP release – promotes platelet aggregation. Mast cell Similar to basophil Contains histamine and heparin. Matured in tissue site. Platelet Plug Formation Accumulation of platelets – seal small breaks in blood vessel Steps: 1. Platelet Adhesion 2. Platelet Activation 3. Platelet Aggregation Agranulocytes Monocytes 3 – 8% of white blood cells Largest of the white blood cells Kidney bean shaped nucleus Increase in chronic infection. Lymphocyte 20 – 25% of WBC Smallest WBC B cells – produces antibodies T cells – protect against viruses and other intracellular microorganism. Platelets (Thrombocytes) Minute fragments of cells. Consist of a small amount of cytoplasm surrounded by a plasma membrane. Life expectancy of platelets is about 5 – 9 days. Hemostasis Complex network of interactions involving vessels, platelets, and factors. Hemostasis involves: Vascular spasm Platelet plug formation Coagulation Coagulation Blood clotting – formation of clot Blood clot – network of threadlike protein fibers (fibrin) that traps blood cells, platelets and fluid Formation is dependent on the clotting factors. Activated only after injury. Extrinsic Pathway Begins with chemicals that are outside of blood. Factor III, Factor VII Damaged tissue releases THROMBOPLASTIN (tissue factor/factor III) Thromboplastin forms a complex with Factor VII (stable factor, proconvertin) Presence of Ca – begins common pathway Intrinsic Pathway Factory XII, XI, IX, VII It begins with chemicals that are inside the blood Damage BV expose collagen – active Factor XII – Factor XI – Factor IX and VII – common pathway Common Pathway Involves fibrinogen (factor I), factors II (prothrombin), V, X Thrombin converts soluble fibrinogen to insoluble fibrin. Control of Clot Formation Blood contains several anticoagulants – to prevent unwanted clotting. Clot Retraction Consolidation or tightening of fibrin clot. Clot retracts it pulls the edges of the damaged vessel close together. Fibrinolysis: Clot Dissolution Plasminogen/ Profibrinolysin – trapped the clot; activated plasmin (fibrinolysin) Plasmin – digests fibrin threads and other clotting factors and removes the clot. Blood Grouping Transfusion – transfer of blood or blood components from one individual to another. Infusion – introduction of fluids other than blood (saline or glucose solution) into the blood. Antigen – present in the surfaces of RBC (blood groups) Antibodies – proteins present in plasma. Donor – person who gives blood. Recipient – person who receives it. ABO Blood Group Used to categorize human blood based on the presence or absence of ABO antigens on the surface of red blood cells. Type A – A antigens; anti-B antibodies Type B – B antigens; anti-A antibodies Type AB – A and B antigens; neither type of antibody Type O – A nor B antigens; anti A and anti-B Rh Blood Group First studied in rhesus monkeys Rh-positive – Rh antigen (the D antigen) on the surface of their red blood cells Rh-negative – Do not have Rh antigen. Diagnostic Blood Tests Type and Crossmatch Blood typing - Determines the ABO and Rh blood groups of the blood sample. Crossmatch - Donor's blood cells are mixed with the recipient's serum; Donor's serum is mixed with the recipient's cells. Complete Blood Count Analysis of blood that provides much useful information Consists: o RBC count o Hemoglobin levels o Hematocrit levels o WBC count o Differential WBC RBC Count Number (expressed in millions) of red blood cells per microliter of blood. Normal: o Male 4.6-6.2 million/µL o Female 4.2-5.4 million/µl Hemoglobin levels Determines the amount of hemoglobin in a given volume of blood Expressed as grams of hemoglobin per 100 mL of blood Normal: o Male - 14-18 g/100 mL o Female - 12-16 g/100 mL Hematocrit levels Percentage of the total blood volume that is composed of red blood cells RBC account for 40-54% of the total blood volume - males 38-47% females Number and size of red blood cells affect the hematocrit measurement. o Normocytes – Normal-sized red blood cells with a diameter of 7.5 mm o Microcytes – Smaller than normal (6 µm or less diameter) o Macrocytes – Larger than normal (9 µm or greater diameter) WBC Count Measures the total number of white blood cells in the blood. 5000-10,000 white blood cells are present in each microliter of blood. o Leukopenia – lower than normal WBC resulting from depression or destruction of the red marrow. o Leukocytosis – abnormally high WBC Differential WBC • Determines the percentage of each of the five kinds of white blood cells • Neutrophils – 60-70% • Lymphocytes – 20-30% • Monocytes – 2-8% • Eosinophils – 1-4% • Basophils – 0.5-1% Platelet Count Normal: 250,000-400,000 platelets per microliter of blood Thrombocytopenia – platelet count is greatly reduced chronic bleeding through small vessels and capillaries. Bleeding time Assessment of platelet function In vivo measure of primary hemostasis o Duke Method o Ivy Method Clotting Blood's ability to clot can be assessed by the platelet count and the prothrombin time measurement. Prothrombin time measurement Expresses how long it takes for the blood to start clotting. Normal: 9-12 seconds Blood Chemistry Analyzed the composition of materials dissolved or suspended in the plasma. Function Assessment of many body's systems • Blood glucose • Blood Urea Nitrogen • Bilirubin • Cholesterol