File
advertisement

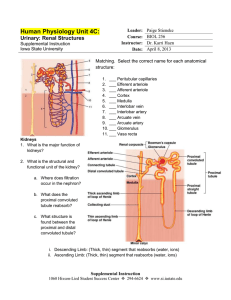
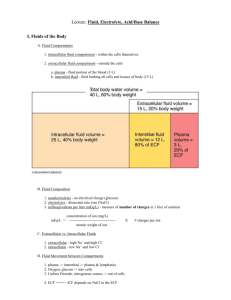
Excretion Excretion is the removal of metabolic waste from the body, that is, the removal from the body of by-products or unwanted substances from normal cell processes. Metabolic waste consists of substances that may be toxic or that are produced in excess by the reactions inside cells. There are 2 substances produced in large amounts: carbon dioxide from respiration and nitrogen containing compounds such as urea. Carbon dioxide is transported in the blood stream to the lungs where it diffuses into the alveoli to be excreted as we exhale. Carbon dioxide has harmful effects on the body: 1. The majority of carbon dioxide is carried in the blood as hydrogencarbonate ions. In the erythrocytes, under the Respiratory Acidosis is the result of a large influence of the enzyme carbonic anhydrase, the hydrogen change in the pH of the blood. Proteins in carbonate dissociates to form H+ ions. The hydrogen ions the blood act as buffers to resist the combine with haemoglobin and compete with oxygen for change in pH. If the change in pH is small, space on the haemoglobin. So, if there is too much carbon extra hydrogen ions are detected by the dioxide, it can reduce oxygen transport in the blood. respiratory centre in the medulla oblongata of the brain. This causes an 2. Carbon dioxide combines directly with the haemoglobin to increase in breathing rate to help to form carbaminohaemoglobin. This molecule has a lower remove the excess carbon dioxide. If the affinity for oxygen than haemoglobin. pH drops below 7.35, it results in slowed or 3. Excess CO2 can cause respiratory acidosis. The carbon difficult breathing, headache, drowsiness, dioxide dissolves directly into the blood plasma. It combines restlessness, tremor and confusion. There with water to produce carbonic acid: CO2 + H2O H2CO3. may also be rapid heart rate and changes in The carbonic acid dissociates: H2CO3 H+ + HCO3- . The H+ blood pressure. lower the pH of the blood, making it more acidic. The Liver Hepatic vein: Blood leaves the liver and re-joins the Vena Cava and blood returns to normal circulation. The bile duct carries bile from the liver to the gall bladder where it is stored until required to help with the digestion of fats in the small intestine. Bile travels in the canaliculi. Hepatic Artery: oxygenated blood from the heart travels from the aorta via the hepatic artery into the liver. Hepatic Portal Vein: deoxygenated blood from the digestive system enters the liver via the hepatic portal vein. The blood is rich in products of digestion. Histology of the Liver The sinusoid is lined by liver cells. As blood flows along the sinusoid, it is in very close contact with the liver cells which can exchange substances with the blood. The sinusoids then empty into the intra-lobule vessel, a branch of the hepatic vein. The hepatic veins from different lobules join together to form the hepatic vein which drains the blood from the liver. The cells, blood vessels and chambers inside of the liver are arranged to ensure the best possible contact between the blood and the liver cells. The hepatic artery (bringing blood from the aorta) and the hepatic portal vein (bringing deoxygenated blood rich in products of digestion from the intestine) enter the liver and split into smaller and smaller vessels. These vessels run between and parallel to the lobules – known as interlobular vessels. Branches from the hepatic artery and hepatic portal vein enter the lobule and the blood is mixed in a chamber called a sinusoid. The sinusoids are lined with specialised macrophages known as Kupffer Cells. They move about within the sinusoids and are involved in the breakdown and recycling of old red blood cells. One of the products of haemoglobin breakdown is bilirubin, which is excreted as part of the bile and in faeces. The liver is very metabolically active. Its functions include: •Control of blood glucose levels, amino acid levels, lipid levels •Synthesis of red blood cells in the fetus, bile, plasma proteins and cholesterol •Storage of vitamins A, D, B12, iron and glycogen •Detoxification of alcohol and drugs •Breakdown of hormones •Destruction of red blood cells Dealing with Proteins… Functions of the Liver Excess amino acids cannot be stored because the amine group makes them toxic. It would however be a waste to excrete the whole molecule, as they contain lots of energy. It therefore undergoes ‘treatment’ in the liver before the amino acid component is excreted. Amino Acid Ammonia + Keto Acid Urea Dealing with Proteins: Deamination Deamination produces ammonia which is very soluble and highly toxic. Keto acid The organic compound that remains is a keto acid. This can be metabolised – used in respiration to release its energy. NH3 Ornithine Cycle Ammonia must be converted to a less toxic substance quickly. The ammonia is combined with carbon dioxide to produce urea – this occurs in the Ornithine cycle. 2NH3 + CO2 Urea is less soluble and less toxic than ammonia. It can be passed into the blood stream transported to the kidneys. In the kidneys, the urea is filtered out of the blood and concentrated in the urine. CO(NH2)2 + H2O Detoxification is the conversion of toxic molecules to less toxic or non toxic molecules. Alcohol is broken down by hepatocytes. Ethanol is dehydrogenated to ethanal by the enzymes ethanol dehydrogenase. The ethanal is further dehydrogenated by ethanal dehydrogenase to form acetate. Ethanol Reduced NAD NAD Ethanol dehydrogenase Ethanal (acetaldehyde) Reduced NAD NAD Ethanal dehydrogenase Ethanoate (acetate) Enters Krebs Cycle to make ATP The coenzyme NAD accepts the hydrogens produced in this reaction. If the liver has got too much alcohol to detoxify, it has insufficient NAD to deal with the fatty acids. These fatty acids are then converted back to lipids and stored in the hepatocytes, causing the liver to become enlarged. This is a condition called ‘fatty liver’ which can lead to alcohol related hepatitis or to cirrhosis. Combines with Coenzyme A to form acetyl CoA which enters respiration. The Kidney The bulk of each kidney consists of tiny tubules called nephrons. There are about 1 million nephrons in each kidney which are closely associated with blood capillaries. Each nephron starts in the cortex. In the cortex, the capillaries form a knot called the glomerulus. This is surrounded by a cup shaped structure called the Bowman’s Capsule. Fluid from the blood is pushed into the bowman’s capsule by ultrafiltration. The capsule leads into the nephron which is then divided into 4 parts: proximal convoluted tubule, loop of Henle, distal convoluted tubule, collecting duct. Formation of Urine 1. Ultrafiltration in the renal capsule [Hydrostatic pressure in the glomerulus] 3. Loop of Henle: Water reabsorption [Descending limb permeable to H2O; Ascending limb permeable to Na+/Cl-] 2. Proximal Convoluted Tubule: Selective Reabsorption 4. Collecting Duct: Osmoregulation Bowman’s Capsule: Ultrafiltration Fluid from the glomerulus is forced into the bowman’s capsule by hydrostatic pressure. The fluid is known as the glomerular filtrate. The blood arrives at the glomerulus through a wide afferent arteriole and leaves through a narrow efferent arteriole. The difference in the diameters ensures that the blood pressure in the glomerulus is higher than in the bowman’s capsule. The pressure difference pushes fluid from the blood into the bowman’s capsule that surrounds the glomerulus. There is a 3 1. Endothelium of the capillaries have narrow gaps between the Squamous epithelial cells, through which blood plasma and the substances dissolved in layered it can pass. barrier that exists 2. Basement membrane consists of a fine mesh of collagen fibres and between glycoproteins. These act as a filter to prevent the passage of molecules with the blood in a molecular mass greater than 69000 – this means that most proteins and all the capillary blood cells are held in the capillaries of the glomerulus. and the 3. The epithelial cells in the bowman’s capsule – called podocytes – have a very lumen of specialised shape. They have many finger-like projections called major the processes. These ensure that there are gaps between cells. Fluid from the bowman’s blood in the glomerulus can pass between those cells into the lumen of the capsule. Bowman’s Capsule. Selective Reabsorption 2. Sodium ions are actively transported out of the cells lining the proximal convoluted tubule. This lowers the concentration of Na+ inside the cells. 4. As glucose and amino acid concentrations build up inside the cell, these substances are able to diffuse out of the opposite side into the tissue fluid. From the tissue fluid, these substances diffuse into the blood and are carried away. 1. Glomerular Filtrate containing water, sodium, amino acids and glucose. 3. Sodium ions, glucose and amino acids are transported down the concentration gradient from the glomerular filtrate into the cells by facilitated diffusion. 5. The reabsorption of salts, glucose and amino acids reduces the water potential inside the cells and increases the water potential of the tubule fluid. Water will therefore enter the cells and then be reabsorbed into the blood by osmosis. Water reabsorption in the Loop of Henle 2. In the descending limb, the fluid from the proximal convoluted tubule passes through tissue into which Na+ and Cl- ions have been pumped. There is therefore a water potential gradient, and water will move from the descending limb into the tissue by osmosis. This arrangement is known as a hairpin counter current multiplier system. 1. In the upper part of the ascending limb, sodium and chloride ions are actively transported out of the nephron and into the surrounding tissues. This increases the water potential of the fluid inside the nephron and decreases the water potential outside of it. 3. When the fluid gets to the base of the descending limb, it is very concentrated – the concentration of the ions is very large. As it goes around to the ascending limb, the Na+ and Cl- ions diffuse out of the tubule. By the time that the fluid reaches the top of the ascending limb in the cortex, its water potential becomes higher. This is because at the base of the tubule, Na+ and Cl- have diffused out of the tubule; higher up, the sodium and chloride ions are being actively pumped out of the tubule; water cannot leave (as the ascending limb is impermeable to water) and so the fluid is losing salts but not water. The longer the loop of Henle the greater the concentration of solutes that can be built up at the bottom of the loop. The very low water potential in the medulla helps water to be conserved and not lost in urine – the water potential gets lower as you go deeper into the medulla. If the tissue surrounding the descending limb has a very high solute concentration, it will have a low water potential. Water will therefore move out of the descending limb and into the capillaries by osmosis. This is advantageous for animals that live in arid conditions, like the desert kangaroo rat, because it minimises the amount of water lost in urine. Explaining Concentration Changes … Glucose: a large drop in concentration as all of the glucose is reabsorbed in the proximal convoluted tubule. Urea: concentration of urea increases as water is reabsorbed. Sodium: in the proximal convoluted tube, what little reabsorption there is is balanced by that of water. The concentration increases in the descending limb as water is lost. The concentration decreases in the ascending limb as Na+ ions are actively pumped out. In the distal convoluted tubule and collecting duct, concentration increases as water is lost. Potassium: the same as for sodium, except in distal convoluted tubule, K+ ions are actively transported in, increasing the concentration. Osmoregulation The control of the water potential of the blood and body fluids. Water is gained by food, drink and respiration. Water is lost in urine, sweat, faeces and water vapour in exhaled air. When less water needs to be conserved, walls of the collecting duct are less permeable: less water is reabsorbed so more urine is produced. When more water needs to be conserved, collecting duct wall become more permeable. More water is reabsorbed and so less urine is produced. If it is a cool day and you have drunk lots of fluid, you will produce large volumes of dilute urine. If it is a hot day and you have drunk little, you will produce small volumes of concentrated urine. The walls of the collecting duct respond to anti-diuretic hormone Cells in the walls of the collecting duct have membrane bound receptors for ADH. The ADH binds to these receptors and causes a chain of enzyme controlled reactions to occur inside the cell. Vesicles containing water permeable channels, aquaporins, fuse with the membranes of the collecting duct cells. This makes the collecting duct walls more permeable to water. If more ADH is released, the walls become more permeable, so more water is reabsorbed by osmosis into the blood. Less urine, with a lower water potential, passes out of the body. If less ADH is released, the cell surface membrane folds inwards to create new vesicles that remove water permeable channels from the membrane. The walls are made less permeable, less water is reabsorbed and more water with a higher water potential passes out of the body. Controlling ADH levels The water potential of the blood is monitored by osmoreceptors ion the hypothalamus of the brain. When the water potential of the blood is low, osmoreceptors lose water by osmosis. This causes them to shrink and stimulates neurosecretory cells in the hypothalamus. Neurosecretory cells are specialised neurones that produce and release ADH. The ADH is manufactured in the cell body of the cells, which lies in the hypothalamus. ADH flows down the axon to the terminal bulb in the posterior pituitary gland. It is sored in the posterior pituitary gland until needed. When the neurosecretory cells are stimulated, they send action potentials down their axons causing the release of ADH into the blood capillaries running through the posterior pituitary gland. It travels in the blood stream around the body and acts on the collecting duct wall cells – these are its target cells. Once the water potential of the blood rises again, less ADH is released. Increase in water potential of blood Detected by osmoreceptors in hypothalamus Decrease in ADH output from posterior pituitary Permeability of collecting duct decreases Less water reabsorbed into bloodstream Increased volume of dilute urine produced Reduced volume of concentrated urine produced More water reabsorbed into bloodstream Permeability of collecting duct increases Increase in ADH output from posterior pituitary Detected by osmoreceptors in hypothalamus Decrease in water potential of blood Kidney Failure The most common causes of kidney failure are diabetes mellitus, hypertension and infection. Dialysis is a process in which blood passes over a partially permeable dialysis membrane. This allows the exchange of substances between blood and dialysis fluid. The fluid contains the correct concentrations of salts, urea, water and other substances in blood plasma. Substances in excess in the blood will diffuse across the membrane and into the dialysis fluid. Haemodialysis: blood form a vein is passed into a machine that contains an artificial dialysis membrane. Dialysis fluid on the other side of the membrane passes in the opposite direction: the fluid has the water potential and contains the concentrations of ions and glucose that the blood should contain if the kidneys were working properly. Heparin is added to avoid clotting and any bubbles are removed before returning to the body. Peritoneal Dialysis: a surgeon implants a catheter into the patient’s abdomen. The peritoneum is the layer of tissue that lines the abdominal cavity. The cavity is filled with dialysis fluid, left there for some time and then drained off. Kidney Transplants: kidney donated by a healthy person who is a close tissue match or a dead donor. Treatment Advantages Disadvantages Haemodialysis More efficient at removing substances Several hours several times a week; between treatments, diet must be managed carefully Peritoneal Dialysis Frees patient from immovable dialysis Higher risk of infection; has to be done machine; continuous process so no large more often swings in blood volume or content Transplant Best life extending treatment; freedom from dialysis; better quality of life Testing Urine Samples Pregnancy Testing Once a foetus is implanted, it releases human chorionic gonadotrophin. This hormone passes through the mother’s nephrons and into the urine. Pregnancy tests use monoclonal antibodies which are tagged with a blue head marker. The antibodies will bind with the HCG and this will form a blue line if the woman is pregnant. Need immunosuppressant drugs for life; major surgery under general anaesthetic; risk of infection and bleeding; side effects of anti-rejection drugs. Anabolic Steroid Testing Gas chromatography or mass spectrometry is used. Gas chromatography involves vaporising the sample in the present of a solvent. It is then passed down a long tube lined by an absorption agent. Each substance stays in the tube for a specific amount of time – the retention time. Once all of the substances have come out of the gas and are absorbed onto the lining, this is analysed to create a chromatogram which can be compared to known standard samples.