3.2.4 Distal convoluted tubule & collecting duct
advertisement

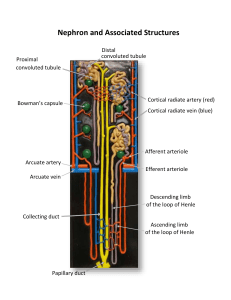
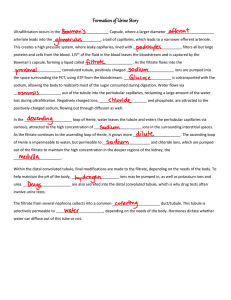
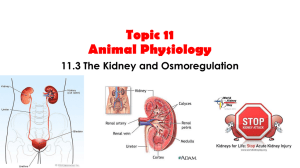
Kidney 1. Functions: • • • • removal of metabolic waste products regulation of the water content of body fluids regulation of pH of body fluids regulation of chemical composition of body fluids 2. Structure of Kidney • • • • • Outer part – renal cortex covered by tough fibrous connective tissue Contain glomeruli, renal corpuscle, PCT,DCT Inner part – renal medulla Contain tubular part of nephron, blood vessels 2.1 Nephron • Basic unit of structure & function • Composed of diff. regions • Renal corpuscle/malpighian capsule [bowman’s capsule & glomerulus] • Proximal convoluted tubule • Descending limb of loop of Henle • • • • Thin segment Ascending limb loop of Henle Distal convoluted tubule Collecting duct 3. Formation of Urine • The two kidneys in the body receive between 1100 – 2000 liters (1160 – 2100 quarts or 500 gallons) of blood per day – about the volume of a car! • Because the body has only about 5.6 liters of blood, our blood runs through the kidneys to be cleaned about once every four minutes. 3.1 Ultrafiltration of blood • Occurs at the renal capsule • Filtration takes place due to high blood pressure • Thin perforated endothelium tissue • Podocytes of renal capsule have slit pores • Except large molecules like proteis, red blood cells and platelets gets filtered [glomerular filtrate]. 3.2 Selective Reabsorption 3.2.1 Proximal convoluted tubule • • • • • • 80% of glomerular filtrate reabsorption occurs Specialized for reasorption Numerous microvilli & basal channels Numerous mitochondria Closeness of blood capillaries Contain carrier protein • Glucose, amino acids and ions actively transported by carrier protein • Diffuse into the blood capillaries and are carried away • Water moves along with these substances 3.2.2 The Loop of Henle • Conserve water and produce concentrated urine • Loop of Henle with vasa recta and collecting duct create and maintain osmotic gradient in medulla • Glomerular filtrate flows in opposite directions in the two limbs of Henle's loop [counter current mechanism] 3.2.3 Descending loop of Henle • Has thin wall • Highly permeable to water and permeable to other solutes 3.2.4 Ascending loop of Henle • • • • Thick & impermeable to water Sodium & other ions are actively reasorbed Interstitial fluid becomes more concentrated Water from descending limb & collecting duct are drawn • The water quickly enters the vasa recta and is being carried away. • This maintains a high concentration of solutes in the interstitial fluid • Filtrate in the ascending limb becomes dilute as it is impermeable to water 3.2.4 Distal convoluted tubule & collecting duct • Fine control of precise amounts of water & salts reasorbed takes place • Water diffuses from the collecting duct into the tissue fluid of medulla • Urine becomes concentrated 3.3 Secretion • Release of unwanted substances from the blood into the nephron which are not present in glomerular filtrate. • Occurs in the convoluted tubules • Aminohippuric acid, K+, H+, Creatinine, Phosphate and antibiotics 4 Hormonal Regulation of Kidney 4.1 Control of blood solute level • The solute potential of blood is controlled by anti-diuretic hormone [ADH]. • Osmoreceptors in Hypothalamus detect change in blood concentration. • Stimulate posterior pituitary gland • Pituitary gland release ADH • ADH travels through blood to Kidney • Increase the permeability of distal convoluted tubule and collecting duct to water. • Less and concentrated urine is produced • Once normal blood concentration is achieved, production of ADH stops • High intake of water inhibits release of ADH • More and dilute urine is produced. • Insufficient release of ADH leads to diabetes insupidus. 4.2 Control of blood sodium level [The renin• • • • angiotensin system] Steady maintenance of blood sodium is brought by Aldosterone. It also influence water reasorption Secreted by adrenal cortex Decrease in blood sodium leads to a decrease in blood volume • Decrease in blood volume reduces blood pressure • Decrease blood pressure and volume stimulates group of secretory cells [macula densa &juxtaglomerular- juxtaglomerular complex] located between DCT & Afferent arteriole • It releases an enzyme – Renin • Renin activates inactive hormone angiotensin present in blood plasma to active form. • Active angiotensin performs tow functions: • it brings about vasoconstriction raising the arterial pressure • it activates adrenal cortex to release aldosterone. • Aldosterone stimulate sodium absorption in the gut and reduce loss in sweat • Sodium absorption increases the reabsorption of water. • Thus it maintains arterial pressure, overall fluid and electrolyte balance.