F214 4-2 Excretion - Please Select a Course
advertisement
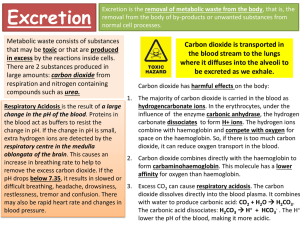
E.F. ACADEMY OCR Biology A2 F214 Communication, Homeostasis and Energy 4.2 Excretion JWh 8/8/2014 1 4.2.1 Define the term excretion; The process of excretion is the removal of waste from metabolic reactions from the body. As this is the unwanted waste products of metabolic reactions they must have been formed within the cell. Excretion must not be confused with egestion, which is the removal of undigested food or chemicals which have never been part of a cellular reaction (e.g. faeces). The main two compounds which are produced are carbon dioxide and urea Explain the importance of removing metabolic wastes, including carbon dioxide and nitrogenous waste, from the body; The need to excrete carbon dioxide is shown by looking at a condition associated with high blood CO2 concentration. CO2 is an acid gas and build- up of H+ decreases the pH of the body causing Respiratory Acidosis. There are three methods of transporting carbon dioxide around the body for removal, outlined below: 1. As Hydrogen Carbonate ions – a process which also produces H+ within Red Blood Cells. 2. Carried around directly dissolved in the blood in solution. 3. Combining directly with Haemoglobin to form Carbaminohaemoglobin Haemoglobin has a higher affinity to carbon dioxide than it does for oxygen, so formation of carbaminohaemoglobin reduces the efficiency of 2 oxygen carriage around the blood. When one haem group has taken up a molecule of carbon dioxide it cannot take on a molecule of oxygen. Hydrogen ions, which are produced alongside hydrogen carbonate ions alter the blood pH level too, which means that enzyme action is slowed. Failure to excrete carbon dioxide from the blood appropriately will result in respiratory acidosis. Symptoms of respiratory acidosis includes: an increased urge to breathe, or hyperventilation. If this occurs for a prolonged period, there can be permanent damage to organs, in particular the brain Urea is produced by oxidising excess amino acids in the liver in a process called deamination. 3 The ammonium ions produced are combined with CO2 in the Ornithene Cycle to produce urea. The urea which is produced there is then transported, to the kidneys, where it will be excreted through urine. The urine is produced in the kidneys and temporarily stored in the bladder. 4 Describe, with the aid of diagrams and photographs, the histology and gross structure of the liver; Hepatocytes (liver cells) carry out many metabolic functions. It is essential that the organ has a rich blood supply to as many cells as possible, and the liver has many secure connections to the blood system. The liver receives oxygenated blood from the hepatic artery and deoxygenated blood from the digestive system through the hepatic portal vein. This blood supplied is rich in the products of digestion, and may contain toxic substances that have been absorbed in the intestine. Blood leaves the liver through the hepatic vein which rejoins the vena cava and returns to systemic circulation. There is also the bile duct leaving the liver, where bile is secreted. This has both digestive and excretory functions. The bile duct runs from the liver to the gall bladder, where bile is stored until needed for digestion. 5 The arrangement of cells within the liver has been adapted so that each cell has a rich blood supply from adjacent blood vessels. The liver is divided into lobes which are further divided into small lobules. The vessels of the hepatic portal vein and hepatic artery, both of which supply the liver with blood, split into smaller vessels, and run alongside other vessels called inter-lobular vessels The Hepatic Artery, Hepatic Portal Vein and Bile duct form a TRIAD around each lobule. 6 Describe the formation of urea in the liver, including an outline of the ornithine cycle; The body needs proteins to function Excess amino acids from proteins which we do not need cannot be stored, because their amine groups make them toxic. The molecule is modified under two processes so that the amine component can be excreted alone. Deamination This is the removal of the amine group from an amino acid. Deamination produces the compound ammonia, which is very toxic and so must not be allowed to accumulate. Another by-product of the process is keto acid, an organic compound which directly enters the mitochondrion and is respired aerobically. The ornithine cycle. Ammonia is very soluble and very toxic, so it needs to be converted into a less harmful substance. The ammonia is combined with carbon dioxide to produce urea in the ornithine cycle. 7 8 Describe the roles of the liver in detoxification; Detoxification of alcohol The liver is able to detoxify many harmful substances Alcohol and drugs can be detoxified in the liver. Hepatocytes contain enzymes which have detoxification functions, such as catalase, which converts hydrogen peroxide (very toxic) into water and oxygen. Alcohol (ethanol) is broken down in the liver using the enzyme ethanol dehydrogenase to produce ethanal, which is broken down using ethanal dehydrogenase into ethanoic acid. This end product combines with coenzyme-A to produce acetyl coenzymeA which can be directly respired The hydrogen atoms released in this reaction can also combine with a molecule of NAD to produce reduced NAD. 9 Describe, with the aid of diagrams and photographs, the histology and gross structure of the kidney; 10 The human body has two kidneys. The urinary system consists of four major parts: 1. the two kidneys 2. the ureters which transport urine from the kidney to the bladder 3. the bladder temporarily stores urine 4. the urethra to take urine to the outside world There are approximately one million tubules within a kidney called nephrons. A nephron exists through each section of the kidney: the outer cortex, the medulla in the middle, and the innermost pelvis The nephron A single nephron consists of the: a. Bowman’s Capsule in which there is a network of capillaries called the Glomerulus - ultrafiltration b. Proximal (first) Convoluted Tubule which runs from the capsule to the loop of Henle – absorption of useful material. c. Loop of Henle, creates the conditions for water reabsorption. d. Distal Convoluted Tubule – ion exchange. e. Collecting Duct which connects to many nephrons and ultimately ending up in the pelvis region – water absorption. 11 Describe, with the aid of diagrams and photographs, the detailed structure of a nephron and its associated blood vessels; Bowman’s Capsule – as blood enters the Bowman’s Capsule, under high pressure, it passes through tree layers as it moves from the blood vessel in the Glomerulus to the Nephron proper. Endothelial cells The endothelial cells lining the glomerular capillaries are thin and flat with a large nucleus. The cells contain pores, which allow plasma components to cross the vessel wall, but not blood cells, platelets or large proteins. 12 Basement membrane The basement membrane is a continuous layer of connective tissue and glycoproteins. It is a non-cellular structure that prevents any large molecules from being filtered. It is the only real barrier to molecules being forced out of the blood Epithelial lining The epithelial lining of Bowman’s capsule consists of a single layer of cells; podocytes, which rest on the basement membrane. The podocytes have large extensions which extend out from the cell body and are embedded in the basement membrane surrounding a capillary. This leads to the formation of slit pores, which control the movement of substances through the final layer of the filter. The podocytes have a well-developed Golgi apparatus, used to produce and maintain the glomerular basement membrane. 13 Describe and explain the production of urine, with reference to the processes of ultrafiltration and selective reabsorption; Ultrafiltration The kidney is concerned with filtering out waste products from the blood plasma, which are to be excreted in the urine. It is important that useful substances are kept. All molecules from the blood plasma below a certain size are passed through the filtration membrane, and those materials which need to be kept are selectively reabsorbed later on. The afferent arteriole which supplies the glomerulus has a much larger width than the efferent arteriole leading away from the glomerulus. This means that there is an increased pressure inside the glomerular capillaries than in most capillaries. This forces fluid from the blood through from the blood capillaries into the renal capsule. This process is called ultrafiltration. The pressure forces molecules within the blood with a relative molecular mass (RMM) of below 69,000 through the glomerular capillaries and into the Bowman’s capsule. This pressure is called filtration pressure. Molecules of water, glucose, urea, amino acids and ions are all removed 14 from the blood plasma and filtered into the nephron. Proteins are too big to fit through the gaps in the basement membrane, and so remain in the blood. Similarly, all blood cells do not enter the glomerular filtrate Selective reabsorption The filtrate which results in the Bowman’s capsule flows along the nephron, and it is at the proximal convoluted tubule that the majority of substances are reabsorbed. This process is known as selective reabsorption. All of the glucose and amino acids are reabsorbed back into the blood. 80% of the Sodium ions (and Cl-), as well as 80% of the water are reaborbed. Selective reabsorption occurs in a several staged process: 1. On the cell surface membrane closest to the blood capillary, there are sodium-potassium pumps which actively transport sodium ions out of the cell. 2. As sodium ions are pumped out of the cell, the concentration of sodium ions inside the cell drops 3. This allows the transport of sodium ions back into the cell from the surface membrane in contact with the proximal convoluted tubule – the ions flow in through co-transporter proteins which couple the movement of sodium ions into the cell with the movement of glucose and amino acids (this is facilitated diffusion) 4. As sodium moves into the cell, taking glucose and amino acids in with it, the concentration of glucose and amino acids within the cell lining the convoluted tubule increases, and so these substances are pumped out of the cell and into the blood capillary via active transport, using carrier proteins. 15 16 5. The movement of ions, glucose and amino acids from the convoluted tubule into the cells leads to an increased water potential (Ψ) inside the convoluted tubule, and so water moves, by osmosis, into the cells lining the tubule and so into the blood capillary 6. The cells lining the proximal tubule have many microvilli on their surface to increase the surface area for absorption, contain many mitochondria and carrier proteins. It is the role of the loop of Henle to establish a low water potential, to ensure that even more of the remaining water can be reabsorbed from the fluid in the collecting duct. The loop of Henle consists of two sections: The descending limb and the ascending limb. The way that the loop of Henle is arranged allows sodium and chloride ions to be pumped out of the ascending limb and into the descending limb. This creates a high concentration gradient of salts (the sodium and chloride ions) in the tubule fluid (the fluid inside the loop of Henle), which causes the salts to move out of the ascending limb and into the surrounding tissue, of the medulla, which of course decreases the water potential. The descending limb is the only limb to not actively pump sodium and chloride ions into the medullary fluid. 1. The descending limb is highly permeable to water, and so water is lost to the surrounding medullary fluid by osmosis as the fluid flows down the limb. 2. The water which is lost is reabsorbed back into the blood by surrounding capillaries 3. This descending limb does not actively lose any sodium or chloride ions 4. At the bottom section and the ascending limb, Chloride ions (followed by Sodium ions) are actively pumped out of the limb into the medullary interstitial fluid, lowering the solute concentration of the filtrate and 17 adding to the solute concentration of the surrounding fluid 5. Near the top of the ascending limb, more sodium chloride is actively transported out into the medullary fluid. 6. The walls of the ascending limb are impermeable to water. 7. Some of these salts may diffuse back into the top of the descending limb, as this is where the concentration of salts is highest in the medullary fluid 8. As the tubule fluid moves along the loop of Henle, the transport of sodium chloride out of the ascending limb, coupled with the osmosis of water out of the descending limb, establishes an osmotic concentration in the medullary interstitial fluid which becomes increasingly hypertonic as the loop drops in towards the medulla. A Counter Current Multiplier System has been set up. 18 19 Explain, using water potential terminology, the control of the water content of the blood, with reference to the roles of the kidney, osmoreceptors in the hypothalamus and the posterior pituitary gland; ADH and the brain There is a water potential gradient down the collecting duct to the medullary tissue of the kidney. This causes water to move out of the collecting duct by osmosis. Water reabsorption in the collecting duct like this is controlled by the levels of ADH (antidiuretic hormone) in the blood vessels in contact with the walls of the collecting duct. ADH is a hormone which in larger amounts will cause molecules called Aquaporins to bind to the cell membrane of the collecting duct. Water passes through the aquaporins more easily and so more water is absorbed, and so urine is more concentrated and less urine is released. The water potential of the blood is detected by sensory cells called osmoreceptors in a region of the brain called the hypothalamus. Normal osmosis rules apply to these cells, as in when the water potential of the blood is low, water will move out of osmoreceptors by osmosis causing the cells to shrivel – and so more ADH is released . 20 When the osmoreceptors shrink due to a lower water potential, they stimulate neurosecretory cells in the hypothalamus to release ADH. When ADH is released it travels down the axon of the cell in which it is made and is stored in the posterior pituitary gland until needed. When the neurosecretory cells have been stimulated, the ADH is released into the bloodstream by the posterior pituitary gland Renal capsule (glomerular filtrate) glucose Proximal convoluted tubule amino acids proteins water urea ions Loop of Henle Distal convoluted tubule reabsorbed Collecting duct not present in filtrate reabsorbed (only small proteins) not present in filtrate not present in filtrate 60% reabsorbed much reabsorption more reabsorbed possible further reabsorption partially reabsorbed Urine mostly reabsorbed final reabsorption (small amounts) not present in filtrate 21 Outline the problems that arise from kidney failure and discuss the use of renal dialysis and transplants for the treatment of kidney failure Kidney failure does not arise from one sole cause. The most common factors which can cause kidney failure are diabetes, hypertension and infection. When kidneys fail, the body is left unable to remove waste substances and excess water from the blood, which of course includes urea, which is harmful. This will ultimately lead to death, and will not take too long. Treatment with dialysis The most common form of treatment for someone with kidney failure is dialysis, which performs the same function as a kidney by passing the blood over a dialysis membrane to remove excess fluids, wastes and salts. The membrane keeps the blood and dialysis fluid separate, but allows for exchange of materials between them. The dialysis fluid contains optimal concentrations of substances, and diffusion across concentrations in the artificial the blood: membrane anything in restores excess flows the correct across the membrane to the fluid, and anything in the blood with too low a concentration flows from the fluid to the blood over the membrane. Haemodialysis is the most common form where blood from a vein is passed over a dialysis membrane in an external machine. 22 The polysaccharide heparin is added to prevent clotting of the blood, and all bubbles are removed before the blood is returned to the body. Haemodialysis is a big burden on someone’s life and prevents them from doing many things they would otherwise be able to do. It must be undergone in a clinic at least three times a week, although many patients buy their own machines and learn how to perform it at home. In peritoneal dialysis, the dialysis is done internally, not via an external machine. A permanent catheter is inserted into the abdomen. In this form of dialysis the filter is the patient’s own abdominal membrane, the peritoneum. Dialysis fluid is inserted through the catheter into the space between the abdominal wall and surrounding organs. The same substance exchange as with haemodialysis occurs here. After a couple of hours, the fluid is drained from the abdomen, and this process must be performed in several consecutive sessions daily. An advantage of peritoneal dialysis is that it has less of an impact on the patient’s life, as they are able to walk around whilst the exchange occurs. However, this must begin with surgery in order to permanently implant the catheter into the abdomen 23 Describe how urine samples can be used to test for pregnancy and detect misuse of anabolic steroids Pregnancy testing A women’s urine can be used to test for pregnancy, using commercially prepared testing strips. The number of coloured bands which appear on a strip are used to categorise as either pregnant or not pregnant. It is the hormone human chorionic gonadotrophin (hCG) which is pivotal here. hCG is produced by the developing placenta, and has important roles during pregnancy. However, some of it is lost to the urine, which is why it can be detected. Women who are not pregnant do not product hCG. An hCG test strip can detect even low levels of the hormone when present in the urine. Urine is drawn along the testing strip across three ‘bands’. These represent three zones, which are often known as the reaction zone, the testing zone and the control zone 1. The reaction zone contains a type of antibody which recognises a single molecular feature of the hCG molecule. These are called monoclonal antibodies and only will bind to hCG. These antibodies have blue beads attached to them, which always remain on the antibodies. The blue beads will later become visible, which will give an indication of pregnancy or no pregnancy 2. The testing zone contains a group of antibodies called polyclonal antibodies which can bind to numerous molecular parts of hCG. 3. The control zone contains antibodies which can recognise and bind to the antibodies which are currently in the reaction zone By this method, when there is hCG present in the urine (i.e. in pregnant women), there will be two blue strips. However, when the woman is not pregnant there is no hCG so the monoclonal antibodies will not attach to the hormone and therefore will not bind to the testing zone, so there is only one blue strip (the 24 control zone at the end) Testing for anabolic steroids Urinary testing can also be used to test for anabolic steroids which can be used to enhance physical performance. This is done using gaseous chromatography. This is a method which separates different gases, so that various substances can be identified within the urine sample. 25