to find the lecture notes for lecture 18 Urinary system click here
advertisement

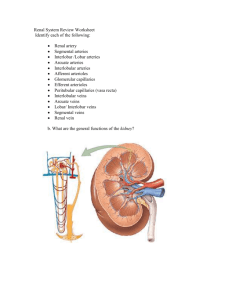
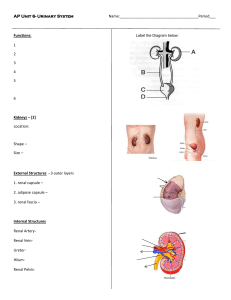
Urinary System Kidneys: formation of urine -contains the functional unit for filtration = Nephron -production of urine, absorption of water and salts Ureters: transfer of urine from kidneys to bladder Urethra: transfer of urine from bladder to outside - longer into the male (20 cm vs. 4 cm in the female) Kidneys • • 10-12 cm retroperitoneal – behind the peritoneum – not part of the abdominal cavity • surrounded by three layers of tissue – 1. deepest layer = renal capsule – transparent sheet of dense irregular connective tissue • continuous with the outer coat of the ureter – 2. middle layer = adipose capsule • amass of fatty tissue surrounding the renal capsule – 3. outer layer = renal fascia • thin layer of dense irregular connective tissue that anchors the kidney to the abdominal wall • divided internally into an outer cortex and an inner medulla – medulla consists of 8 to 18 cone-shaped regions called renal pyramids – the wider base faces towards the cortex, the narrow region (renal papilla) projects down into a cup-like structure called a minor calyx – renal cortex is divided into an outer cortical zone and a deeper juxtamedullary zone – the cortex also extends down in between the pyramids to form the renal columns – renal lobe = renal pyramid + the overlying renal cortex + ½ the adjacent renal colum Blood supply • • • • • • • • • • • • supplied by a renal artery and drained by a renal vein(s) kidney receives 20-25% of the resting cardiac output through the renal arteries (1200mL per minute) renal artery divides into segmental arteries – supply segments of the kidney the segmental arteries give off branches that pass through the renal columns – interlobar arteries at the base on the renal pyramids – between the medulla and cortex – they are called arcuate arteries divisions from the arcuate are called the interlobular arteries (pass between the renal lobes) the afferent arterioles are derived from the interlobular arteries afferent arteriole supplies one nephron and forms the glomerulus (capillary network) drainage of the glomerulus is via the efferent arteriole efferent arteriole forms the peritubular capillary network which surround the upper portions of the nephron an extension of this network covers the lower portion of the nephron (loop of henle) – vasa recta the peritubular capillaires form the interlobular veins – arcuate veins – interlobar veins – renal vein The Nephron -about one million nephrons -kidneys filter 180 L fluid per day!!!! -each nephron is a renal corpuscle + renal tubules -renal corpuscle: filtering unit consisting of a tangled cluster of capillaries -> glomerulus + Bowman’s capsule -tubules: for reabsorption of water and ions leading to final urine volume and composition -PCT +Loop of Henle + DCT Cortical Nephron • 80-85% of nephrons are cortical nephrons • Renal corpuscles are in outer cortex and loops of Henle lie mainly in cortex Juxtamedullary Nephron • 15-20% of nephrons are juxtamedullary nephrons • Renal corpuscles close to medulla and long loops of Henle extend into deepest medulla enabling excretion of dilute or concentrated urine Urinary System Function 1. Excretion of Metabolic Wastes: nitrogenous wastes -Urea: by-product of amino acid metabolism -produced when ammonia + carbon dioxide -Creatinine: produced by breakdown of creatine phosphate (high energy molecule reserve of muscles) -Uric acid: by-product of nucleotide breakdown -insoluble and ppts in the blood, concentrates in joints 2. Water-Salt balance of blood: reabsorption into blood from the descending Loop of Henle, from collecting duct -reclaim salt from the ascending portion of Loop of Henle -reclaim urea from bottom section of collecting duct -release of anti-diuretic hormone by pituitary: increase reabsorption of water 3. Acid-Base balance of blood: reabsorption of bicarbonate ions from urine in the nephron decreases levels in blood (decreases carbonic acid levels) -movement of hydrogen ions from blood into the nephron, combines with ammonia to form ammonium (NH4+) 4. Secretion of hormones: release of renin by kidneys which leads to release of aldosterone by adrenal glands (reabsorption of salts by kidneys) -release of erythropoietin by kidneys (stimulates RBC production) -activation of vitamin D produced by the skin Water Balance -extracellular fluids: blood plasma, interstitial fluid, CSF, etc…. -intracellular fluids: cytosol -unique distribution of ions in ECF and ICF e.g. -intracellular fluids: higher potassium, phosphate, magnesium - lower sodium, chloride and bicarb ions than in extracellular fluid -of the 40 liters of water in the average male - 37% is ECF and 63% is ICF -so the kidney’s ability to modulate the composition of blood plasma can determine the composition of interstitial fluid and therefore ICF Water Intake -average intake - 2.5 L (60% from drinking water, 30% from moist foods, 10% byproduct of metabolism) -regulation of intake - thirst center within the hypothalamus e.g. as body loses water - osmoreceptors within the thirst center detect increase in osmotic pressure within the ECF (increase as little as 1%) -drinking distends the stomach which inhibits signalling from the thirst center Water output -loses through urine, feces and sweat plus respiration and skin evaporatio -2.5 L of water must be lost for water balance -60% lost in urine, 6% in feces, 6% in sweat, 28% evaporation from skin and lungs -primary means of controlling output is through urine production -dehydration: ECF becomes concentrated - increase osmotic pressure - pressure increase detected by osmoreceptors in hypothalamus -posterior pituitary gland releases anti-diuretic hormone (ADH) -ADH causes distal convoluted tubule and collecting duct to increase water reabsorption -excess water intake: ECF less concentrated - decrease in O.P -osmoreceptors signal to the post. pituitary -P.P decreases ADH release -kidney/nephrons decrease water reabsorption Renal physiology • comprised of filtration at the capsule (1) • reabsorption through the tubules (2) • direct secretion by the cells lining these tubules (3) • • • glomerulus: capillary tangle derived from afferent arterioles (into) and lead into efferent arterioles (out) surrounded by a glomerular capsule (Bowman’s capsule) – single layer of epithelial cells glomerular capsule: site of initial filtration and the first step in the formation of urine – consists of visceral and parietal layers – visceral layer consists of modified epithelial cells = podocytes – the podocytes wrap around the endothelial cells of the glomerular capillaries and forms the filtration membrane together with the endothelial cell wall • slits are covered with a slit membrane that permits the passage of small molecules such as water, vitamins, amino acids, wastes and small plasma proteins – space between the visceral and parietal layers = glomerular capsule – between the union of the afferent and efferent arterioles are mesangial cells that help regulate the rate of glomerular filtration • 1. Glomerular filtration Renal Physiology – depends on three main pressures • 1. glomerular blood pressure (GBP) – BP in the glomerular capillaries (55 mmHg) – promotes filtration by forcing water and solutes through the filtration membrane • 2. caspsular hydrostatic pressure (CHP) – hydrostatic pressure exerted against the filtration membrane by fluid already in the bowman’s capsule – opposes filtration from the blood – 15 mm Hg • 3. blood collioid osmotic pressure (BCOP) – due to the presence of plasma proteins in the blood – opposes filtration from the blood – 30 mmHg • net filtration pressure (NFP) = GBP – CHP – BCOP = 10 mm Hg • loss of plasma proteins in the urine can cause edema (increased interstitial fluid) – damage to the glomerular capillaries can increase their permeabilty – loss of the larger plasma proteins – this increases the BCOP which draws larger amounts of water out of the blood and into the urine – but the BCOP decreases because we are losing these plasma proteins in the urine – the overall drop in BCOP causes water to leave the blood and enter the tissues systemically Glomerular filtration rate • glomerular filtration rate (GFR) – amount of filtrate formed per minute (125 mL/min) – affected dramatically by NFP – adjusted by regulating: 1) blood flow into and out of the glomerulus and 2) the glomerular capillary surface area available for reabsorption – three mechanisms control GFR GFR • 1. renal autoregulation – two mechanisms – myogenic mechanism and tubuloglomerular feedback – myogenic mechanism – increased blood volume can increased GFR • by the stretching of the afferent arterioles triggers the contraction of the smooth muscle lining these arterioles – tubulogomerular mechanism – feedback provided to the glomerulus from the renal tubules • increase in the fluid through the PCT, LH and DCT – less time to reabsorb materials • cells in these tubules induce vasoconstriction in the afferent arterioles • if GFR drops below normal – these cells stimulate the release of NO from the juxtaglomerular cells – vasodilation which increases blood flow and GFR • 2. neural regulation – sympathetic ANS fibers release norepinephrine which causes vasoconstriction of the smooth muscle in the afferent arteriole • 3. hormonal regulation – release of angiotensin II reduces GFR by inducing vasoconstriction – also release of atrial natriureic peptide (ANP – from the cardiac cells) increases GFP by increasing the surface area of the glomerulus PCT and Loop of Henle • proximal convoluted tubule: first area of reabsorption into blood -> Loop of Henle -> distal convoluted tubule -> collecting duct -> union of ducts into ureter • cells of these tubules are also single epithelial layers – vary as either cuboidal (PCT and DCT, descending) or squamous (ascending LH) • PCT and DCT surrounded by the peritubular network of capillaries for reabsorption back into the blood, LH is covered with the vasa recta • PCT is the site of water reabsorption (PASSIVE) - associated with the ACTIVE reabsorption of sodium and potassium ions – active Na+ and K+ uptake by the blood from the PCT is by sodium pumps - sodium pumped from the PCT and chloride, bicarbonate and phosphate ions follow it - salt reabsorption – the active transport of ions into the blood plasma increases osmotic pressure within the blood – therefore water moves out of the PCT into the capillaries PASSIVELY! • PCT reabsorbs about 70% of filtered Na+, ions and water – the apical surface of the PCT epithelium forms microvilli which increases the surface area of this region Loop of Henle • active transport of Na+ continues through the loop of Henle and DCT • descending loop of Henle is quite permeable to water but impermeable to solute movement – urine becomes hypertonic (increased ions within the urine, decreased water) • ascending loop is the opposite – permeable to salt (salt pumped out of the urine back • into the blood plasma) • the wall of the arterioles alongside the ascending portion of the LH contain modified smooth muscle cells = juxtaglomerular cells – regulate blood pressure within the kidneys DCT and Collecting Duct • two types of cells found in the DCT and CD – principal cells – receptors for ADH and aldosterone – intercalated cells – play a role in the homeostasis of blood pH • DCT and collecting duct are impermeable to water !!!! • the DCT and CD become permeable upon action of hormones Renal Physiology • Tubular reabsorption – tubule cells reabsorb about 99% of the filtered water and many of the solutes – principal materials reabsorbed – glucose, aminao acids, urea, Na+, K+, Ca+, Cl-, HCO3- and HPO4– return to the blood through reabsorption into the peritubular capillary network and vasa recta – reabsorption = return to the blood – absorption = entrance of new materials into the blood (e.g. via digestive absorption) – reabsorption routes – one of two routes before re-entering the blood Reabsorption Routes • Paracellular reabsorption • between adjacent tubule cells into the blood – 50% of reabsorbed material moves between cells by diffusion in some parts of tubule • Transcellular reabsorption – material moves through both the apical and basal membranes of the tubule cell by active transport Renal Physiology • Tubular secretion – tubular cells also secrete other materials – wastes, drugs, excess ions into the urine – this also removes these materials from the blood Reabsorption in the PCT Reabsorption of Nutrients • Na+ symporters help reabsorb materials from the tubular filtrate • Glucose, amino acids, lactic acid, water-soluble vitamins and other nutrients are completely reabsorbed in the first half of the proximal convoluted tubule • Intracellular sodium levels are kept low due to Na+/K+ pump Reabsorption of Bicarbonate, Na+ & H+ Ions • Na+ antiporters reabsorb Na+ and secrete H+ – PCT cells produce the H+ & release bicarbonate ion to the peritubular capillaries – important buffering system • For every H+ secreted into the tubular fluid, one filtered bicarbonate eventually returns to the blood Passive Reabsorption in the 2nd Half of PCT • Electrochemical gradients produced by symporters & antiporters causes passive reabsorption of other solutes • Cl-, K+, Ca+2, Mg+2 and urea passively diffuse into the peritubular capillaries • Promotes osmosis in PCT (especially permeable due to aquaporin-1 channels Secretion of NH3 & NH4+ in PCT • Ammonia (NH3) is a poisonous waste product of protein deamination in the liver – most is converted to urea which is less toxic • Both ammonia & urea are filtered at the glomerus & secreted in the PCT – PCT cells deaminate glutamine in a process that generates both NH3 and new bicarbonate ion. • Bicarbonate diffuses into the bloodstream – during acidosis more bicarbonate is generated Reabsorption in the Loop of Henle • Tubular fluid – PCT has reabsorbed 65% of the filtered water so chemical composition of tubular fluid in the loop of Henle is quite different from plasma – since many nutrients were reabsorbed as well, osmolarity of tubular fluid is close to that of blood Countercurrent Mechanism: Reabsorption at Loop of Henle Symporters in the Loop of Henle • Thick limb of loop of Henle has Na+ K- Clsymporters that reabsorb these ions • K+ leaks through K+ channels back into the tubular fluid leaving the interstitial fluid and blood with a negative charge • Cations passively move to the vasa recta Reabsorption in the DCT • Removal of Na+ and Cl- continues in the DCT by means of Na+ Cl- symporters • Na+ and Cl- then reabsorbed into peritubular capillaries • DCT is major site where parathyroid hormone stimulates reabsorption of Ca+2 – DCT is not very permeable to water so it is not reabsorbed with little accompanying water Reabsorption & Secretion in the Collecting Duct • By end of DCT, 95% of solutes & water have been reabsorbed and returned to the bloodstream • Cells in the collecting duct make the final adjustments – principal cells reabsorb Na+ and secrete K+ – intercalated cells reabsorb K+ & bicarbonate ions and secrete H+ Actions of the Principal Cells • Na+ enters principal cells through leakage channels • Na+ pumps keep the concentration of Na+ in the cytosol low • Cells secrete variable amounts of K+, to adjust for dietary changes in K+ intake – down concentration gradient due to Na+/K+ pump • Aldosterone increases this Na+ reabsorption (and passive water reabsorption) & K+ secretion by principal cells by stimulating the synthesis of new pumps and channels. Secretion of H+ and Absorption of Bicarbonate by Intercalated Cells • Proton pumps (H+ATPases) secrete H+ into tubular fluid – can secrete against a concentration gradient so urine can be 1000 times more acidic than blood • Cl-/HCO3- antiporters move bicarbonate ions into the blood – intercalated cells help regulate pH of body fluids • Urine is buffered by HPO4 2- and ammonia (secreted by cells of PCT), both of which combine irreversibly with H+ and are excreted Production of Dilute or Concentrated Urine • Homeostasis of body fluids despite variable fluid intake • Kidneys regulate water loss in urine • ADH controls whether dilute or concentrated urine is formed – if lacking, urine contains high ratio of water to solutes – dilute urine – reabsorption of ions is unchanged (normal) but ADH decreases reabsorption of water Summary • H2O Reabsorption – – – – PCT---65% loop---15% DCT----10-15% collecting duct--5-10% with ADH Renin-Angiotensin-Aldosterone • when blood volume and BP drop – the walls of the afferent arterioles are stretched less – juxtaglomerular cells secrete renin into the blood (also stimulated by sympathetic stimulation) • in the blood renin cleaves angiotensinogen (made by hepatocytes) to form angiotensin I • the enzyme ACE (in the lung) – cleaves this even more to form angiotensin II – 1. decreases GFR by causing vasoconstriction of afferent arterioles – 2. enhances reabsorption of Na+, Cl+ and water in the PCT by stimulating the Na/H antiporter – 3. stimulates the release of aldosterone by the adrenal cortex – stimulates the principal cells of the DCT collecting ducts to reabsorb more Na and Cl and secrete more K into the blood • osmotic consequence of this causes an increased reabsorption of water ADH and ANP • ADH – released by the posterior pituitary – regulated water reabsorption by increasing the permeability of the principal cells in the DCT to water – in the absence of ADH the principal cells of the DCT and CT have low permeability to water – within the principal cells are vesicles containing a protein called aquaporin-2 • ADH stimulates the insertion of aquaporin-2 into the apical membrane • water permeability increases • when the OP of the blood plasma increases (decreased water concentration ) via increased filtration – osmoreceptors in the hypothalamus detect this drop and stimulate the release of ADH • increased permability to water reintroduces water back into the blood and lower the OP of the blood plasma • ANP – inhibits the reabsorption of Na and water in the PCT and the collecting duct – also suppresses the secretion of aldosterone and ADH • increases the excretion of Na in the urine (natriuresis) and increase urine output (diuresis) which decreases blood volume and BP and inhibits its further release