1. What are the most likely factors responsible for the elevation of the
advertisement

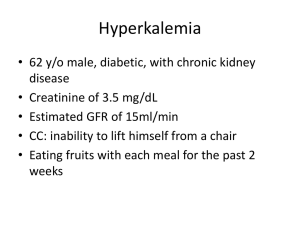
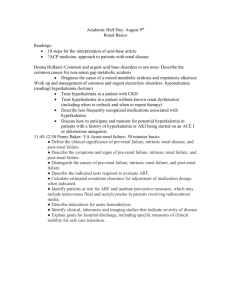
A 62 y/o M diabetic with chronic kidney disease and a creatinine of 3.5 mg/dl and an estimated GFR of 15 ml/min consults due to the inability to lift himself from a chair. He had been eating fruits with each meal for the past two weeks. On PE there is marked proximal weakness and decreased skin turgor. The ECG revealed peaked T waves and widening of the P wave and QRS complex. Salient Features • • • • • • • 62 M CKD Diabetic CC: inability to lift himself from a chair Creatinine of 3.5 mg/dl GFR of 15 ml/min – Low Decreased skin turgor and marked proximal weakness • ECG: Peaked T waves and widening of P wave and QRS complex Laboratory Results Parameters Patient Normal Values Plasma Na 130 meq/L 136-146 meq/L K 8.5 meq/L 3.5-5.0 meq/L Cl 98 meq/L 102-109 meq/L HCO3 17 meq/L 22-30 meq/L Creatinine 2.7 meq/L 0.6-1.2 meq/L 7.32 7.35-7.45 pH Capillary Blood Glucose Serum Acetone 400 mmol/L + 3.9-6.7 mmol not more than 125 mg/dl - 1. What are the most likely factors responsible for the elevation of the plasma potassium? Most likely causes of Hyperkalemia in the patient 1. ) The patient has chronic kidney disease and is in renal failure – GFR 15 ml/min – Compensatory mechanism for increasing distal flow rate and K secretion per nephron is decreased because there is decreased renal mass in chronic renal insufficiency 2.) The patient has diabetes - Insulin deficiency and hypertonicity promote K shift from the ICF to the ECF. 3. Intake of fruits does not necessarily cause hyperkalemia. - Huge amount of parenteral K can elicit hyperkalemia. 4. Acidosis causes shift of potassium from intracellular space into extracellular space. 2. Is this pseudohyperkalemia? Why or why not? PSEUDOHYPERKALEMIA • Artificially elevated plasma K+ concentration due to K + movement out of cells immediately prior to or following venipuncture • Contributing factors: prolonged use of tourniquet with or without repeated fist clenching, hemolysis, and marked leukocytosis or thrombocytosis • marked leukocytosis or thrombocytosis results in an elevated serum K + concentration due to release of intracellular K + following clot formation Harrison’s Principles of Internal Medicine 17th ed. Onyekachi Ifudu, Mariana S. Markell, Eli A. Friedman. Unrecognized Pseudohyperkalemia as a Cause of Elevated Potassium in Patients with Renal Disease PSEUDOHYPERKALEMIA • serum to plasma potassium difference of more than 0.4 mmol/l • occurs when platelets, leukocytes or erythrocytes release intracellular potassium in vitrofalsely elevated serum values. • Observed in: – Myeloproliferative disorders including leukemia – Infectious mononucleosis – Rheumatoid arthritis 2. Is this pseudohyperkalemia? Why or why not? NO… this is not pseudohyperkalemia since there are no enough evidence of blood count differentials as well as no history predisposing the patient to develop such. Also, the presence of ECG abnormalities which require emergency therapy is not a common indication in pseudohyperkalemia 3. What are the clinical manifestations of hyperkalemia in this patient? Explain the pathophysiology. HYPERKALEMIA • Excessive intake – Uncommon cause of hyperkalemia – Most often, hyperkalemia is caused by a relatively high potassium intake in a patient with impaired mechanisms for the intracellular shift of potassium or for renal potassium excretion • Decreased excretion – Most common cause of hyperkalemia • Decreased excretion of potassium, especially coupled with excessive intake – Decreased renal potassium excretion • Renal failure • Ingestion of drugs that interfere with potassium excretion – Potassium-sparing diuretics, angiotensin-convening enzyme inhibitors, nonsteroidal anti-inflammatory drugs • Impaired responsiveness of the distal tubule to aldosterone – Type IV renal tubular acidosis observed with diabetes mellitus, sickle cell disease, or chronic partial urinary tract obstruction • Shift from intracellular to extracellular space – Uncommon cause of hyperkalemia – Exacerbate hyperkalemia produced by a high intake or impaired renal excretion of potassium. – Clinical situations in which this mechanism is the major cause of hyperkalemia includes • • • • Hyperosmolality Rhabdomyolysis Tumor lysis Succinylcholine administration – Depolarizes the cell membrane and thus permits potassium to leave the cells CLINICAL MANIFESTATIONS • Weakness – Prolonged depolarization impairs membrane excitability • Since the resting membrane potential is related to the ratio of the ICF to ECF K+ concentration, hyperkalemia partially depolarizes the cell membrane – It may progress to flaccid paralysis and hypoventilation if the respiratory muscles are involved • Metabolic acidosis – Net acid excretion is impaired • Inhibition of renal ammoniagenesis and reabsorption of NH4+ in the TALH – It may exacerbate the hyperkalemia due to K+ movement out of cells • Cardiac toxicity – Increased T-wave amplitude, or peaked T waves – Prolonged PR interval and QRS duration, atrioventricular conduction delay, and loss of P waves • More severe degrees of hyperkalemia – Sine wave pattern • Progressive widening of the QRS complex and merging with the T wave – The terminal event is usually ventricular fibrillation or asystole How would you manage this case? Management • Most important consequence of Hyper K is altered Cardiac Conductance – With the risk of bradycardia and cardiac arrest • The patient should be treated as an emergency case and warrants emergency treatment – + ECG changes and K > 6.0 mM (Px= 8.5 mM) Urgent Management • • • • 12- lead ECG Admission to the hospital Continuous cardiac monitoring Immediate treatment Treatment • Antagonism of the cardiac effect of hyperkalemia – Stabilize membrane potential • Calcium Therapy 10% Ca gluconate, 10 mL over 10 mins or Calcium chloride 5 mL of 10% sol IV over 2 min • Stop infusion if bradycardia develops • Rapid reduction in K+ by redistribution into cells – Cellular K+ uptake • Insulin 10 U R (CBG= 400 mmol/L) • B2-agonist nebulize albuterol, 10-20 mg in 4mL saline Treatment • Removal of K+ from the body – Furosemide 20-250 mg IV – Kayexalate 30-60 g mixed with 100 mL of 20% sorbitol PO – Hemodialysis (if necessary) • Intractable Acidosis • Uncontrollable Hyperkalemia • Sodium Bicarbonate – 1 mEq/kg slow IV push or continuous IV drip