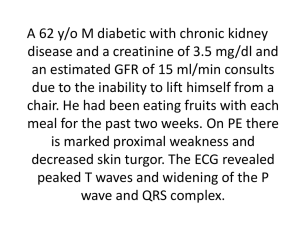
Hyperkalemia
Hyperkalemia is defined as a [K+] higher than 5.0 mmol/liter. If levels exceed 6 mmol/liter, perturbations
in the resting cell membrane potential occur and normal depolarization and repolarization are impaired.
The most common cause of hyperkalemia is renal failure in hospitalized patients. The transport of
potassium is passive, but the transport of sodium requires energy. This difference across the cell is
maintained by Na+,K+-ATPase activity, which requires energy. The energy is in the form of cellular ATP;
its levels are highly variable in different stages of shock when nutrients are not available (whether
carbohydrates or oxygen). When cellular ATP levels fall, the sodium pump is impaired. If sodium or
potassium levels are severely high or low, the membrane potential will be affected. Eventually, without
energy, cell death occurs, and the Na+-K+ gradient cannot be maintained; the sodium gradient is needed
to maintain the membrane potential.
The primary clinical problem is cardiac arrhythmia, which can be lethal. Hyperkalemia is associated with
peaked T waves; dangerous hyperkalemia (6 to 7 mmol/liter) is indicated by T waves higher than R
waves (Fig. 5-23).
FIGURE 5-23 Electrocardiographic changes. A, Indicating hyperkalemia. The T wave is tall, narrow, and
symmetrical. B, Indicating acute myocardial infarction. The T wave is tall but broad-based and asymmetrical.
(From Somers MP, Brady WJ, Perron AD, et al: The prominent T wave:
Electrocardiographic differential diagnosis. Am J Emerg Med 20:243–251, 2002.)
The most common cause of hyperkalemia is acute onset of renal dysfunction or failure. Cellular injury
(e.g., sepsis or ischemia reperfusion) can also release potassium from its intracellular source, which can
overwhelm the kidneys’ ability to clear potassium. At least 20% of normal renal function is required to
respond to ADH and maintain normal potassium levels. The reperfusion of ischemic tissues resulting in
rhabdomyolysis causes high potassium levels; to prevent cardiac arrest, a bolus of IV sodium bicarbonate
may be of some benefit. The bicarbonate shifts potassium intracellularly. Note that impaired aldosterone
levels (as with infarction of bilateral adrenal glands) can activate other renal mechanisms and stimulate
potassium excretion, resulting in moderate levels of hyperkalemia.
Drugs can have a direct effect on the renal tubules and on potassium excretion, such as triamterene,
spironolactone, beta blockers, cyclosporine, and tacrolimus. They are usually a contributing factor but not
a primary cause. Succinylcholine, a depolarizing paralytic agent, is used in patients with muscle atrophy
from disuse, prolonged bed rest, neurologic denervation syndromes, severe burns, direct muscle trauma,
or rhabdomyolysis; it can cause severe hyperkalemia, resulting in cardiac arrest. When drawing blood
samples from patients, clinicians must recognize that sample hemolysis can release potassium, so
laboratory test results could be spurious. If the sample or test results are suspect, another sample should
be taken before drastic efforts are made to treat hyperkalemia.
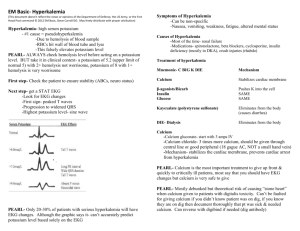
Treatment of Hyperkalemia
In patients at risk of developing cardiac arrhythmia from hyperkalemia, several interventions are useful. IV
calcium can immediately reduce the risk of arrhythmia by antagonizing the depolarization effect of
elevated [K+]. Sodium bicarbonate infusion buffers extracellular protons and allows for the net transfer of
cytosolic protons across the cell membrane via carbonic acid. The shift of protons out of the cell is
associated with a shift of potassium into the cells. Bicarbonate therapy is most effective in hyperkalemic
patients with metabolic acidemia. Insulin and glucose infusions prompt an increase in Na+,K+-ATPase
activity and decline in extracellular water potassium concentration as the extracellular water potassium is
pumped into the cell.
In patients with aldosterone deficiency and hyperkalemia, a mineralocorticoid drug such as 9αfludrocortisone will increase the renal excretion of potassium. In patients with acute renal failure,
hemodialysis is the most reliable method to control hyperkalemia. Continuous filtration methods clear
K+ at a slower rate than hemodialysis. Chronic hyperkalemia associated with renal dysfunction can be
managed by oral or rectal administration of sodium polystyrene sulfonate, a cation exchange resin that
binds potassium in the gut lumen. Rectally administered binding resins are particularly effective because
the colonic mucosa can excrete mucus with large amounts of potassium. Surgeons should clearly
establish a process for managing hyperkalemia, because rapidly escalating potassium levels pose an
immediate threat and require rapidly delivered effective therapy (Box 5-6). Dysfunctional renal handling of
potassium from mineralocorticoid deficiency or resistance leads to hyperkalemia. Renal failure is
commonly associated with tubular defects and potassium management problems, along with
hyperaldosteronism. However, in patients with normal renal function, assessing levels of aldosterone,
renin, and cortisol can help differentiate between mineralocorticoid deficiency and resistance. In patients
with aldosterone deficiency, fludrocortisone is useful.
Box 5-6
Guidelines for Treatment of Adult Patients With Hyperkalemia
First: Stop all infusion of potassium.
Electrocardiographic Evidence of Pending Arrest
Loss of P wave and broad slurring of QRS; immediate effective therapy indicated
1
IV infusion of calcium salts:
10 mL of 10% calcium chloride over 10-minute period
or
10 mL of 10% calcium gluconate over 3- to 5-minute period
2
IV infusion of sodium bicarbonate: 50-100 mEq over 10- to 20-minute period;
benefit proportional to extent of pretherapy acidemia
Electrocardiographic Evidence of Potassium Effect
Peaked T waves; prompt therapy needed
1
Glucose and insulin infusion: IV infusion of 50 mL of D50W and 10 units of
regular insulin; monitor glucose
2
Immediate hemodialysis
Biochemical Evidence of Hyperkalemia and No Electrocardiographic Changes
Effective therapy needed within hours
1 Potassium-binding resins into the gastrointestinal tract, with 20% sorbitol
2 Promotion of renal kaliuresis by loop diuretic
D50W, 50% dextrose in water.
Copyright © 2013 Elsevier Inc. All rights reserved. Read our Terms and Conditions of Use and
our Privacy Policy.
For problems or suggestions concerning this service, please contact: online.help@elsevier.com