Electrolyte and Metabolic Disturbances
advertisement

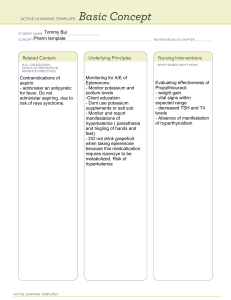
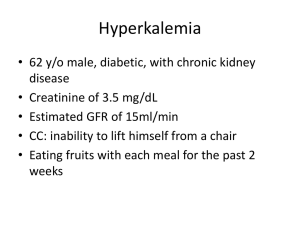
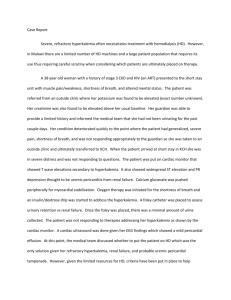
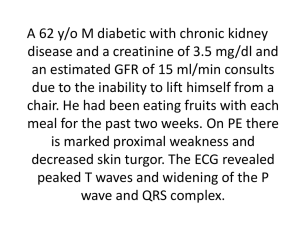
Objectives Review causes and clinical manifestations of severe electrolyte disturbances Outline emergent management of electrolyte disturbances Recognize acute adrenal insufficiency and appropriate treatment Describe management of severe hyperglycemic syndromes Principles of Electrolyte Disturbances Implies an underlying disease process Treat the electrolyte change, but seek the cause Clinical manifestations usually not specific to a particular electrolyte change, e.g., seizures, arrhythmias Principles of Electrolyte Disturbances Clinical manifestations determine urgency of treatment, not laboratory values Speed and magnitude of correction dependent on clinical circumstances Frequent reassessment of electrolytes required Hypokalemia Neuromuscular manifestations (weakness, fatigue, paralysis, respiratory dysfunction) GI (constipation, ileus) Nephrogenic DI ECG changes (U waves, flattened T waves) Arrhythmias Hypokalemia Spurious hypokalemia Marked leukocytosis A dose of insulin right before the blood draw Redistribution hypokalemia Alkalosis (K decreases .3 for every .1 increase in pH) Increased Beta2 adrenergic activity Theophylline toxicity Familial Hypokalemia Extrarenal depletion diarrhea laxative abuse sweat losses fasting or inadequate intake Hypokalemia Renal potassium depletion urine potassium > 20 mEq/24 hrs spot urine with > 20 mEq K/gram creatinine classified whether they occur with a metabolic alkalosis vomiting/NG suction diuretic tx Mineralocorticoid excess syndromes Hypokalemia Renal losses metabolic acidosis RTA Type I and II DKA Carbonic anhydrase inhibitor therapy Ureterosigmoidostomy No acid-base disorder Mg deficiency Drugs Hyperkalemia Severe hyperkalemia is a medical emergency Neuromuscular signs (weakness, ascending paralysis, respiratory failure) Progressive ECG changes (peaked T waves, flattened P waves, prolonged PR interval, idioventricular rhythm and widened QRS complex, “sine wave” pattern, V fib) Hyperkalemia Etiology – renal failure, transcellular shifts, cell death, drugs, pseudohyperkalemia Manifestations – cardiac, neuromuscular Hyperkalemia Impaired potassium secretion Aldosterone deficiency adrenal failure Syndrome of hyporeninemic hypoaldosteronism (SHH) tubular unresponsiveness Renal failure GFR < 10 -20% of normal Hyperkalemia Treatment Stop potassium! Get and ECG Hyperkalemia with ECG changes is a medical emergency Hyperkalemia Treatment First phase is emergency treatment to counteract the effects of hyperkalemia IV Calcium Temporizing treatment to drive the potassium into the cells glucose plus insulin Beta2 agonist NaHCO3 Hyperkalemia Treatment Therapy directed at actual removal of potassium from the body sodium polystyrene sulfonate (Kayexalate) dialysis Determine and correct the underlying cause Body Fluid Distribution ECF Vascular Interstitial ICF Intracellular TOTAL Water (L) [Na] (mmol/L) [K] (mmol/L) 3 16 140 140 5 5 23 10 150 42