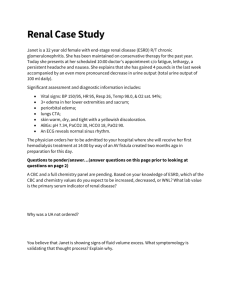
case report malawi by Steere
advertisement

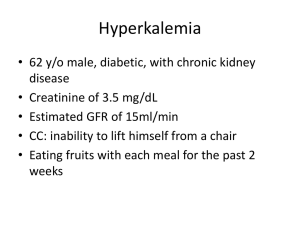
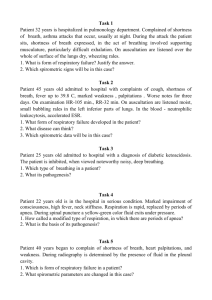
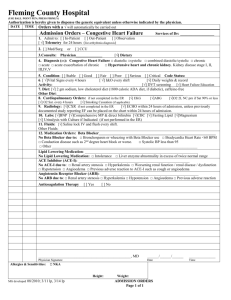
Case Report Severe, refractory hyperkalemia often necessitates treatment with hemodialysis (HD). However, in Malawi there are a limited number of HD machines and a large patient population that requires its use thus requiring careful scrutiny when considering which patients are ultimately placed on therapy. A 38 year old woman with a history of stage 3 CKD and HIV (on ART) presented to the short stay unit with muscle pain/weakness, shortness of breath, and altered mental status. The patient was referred from an outside clinic where her potassium was found to be elevated (exact number unknown). Her creatinine was also found to be elevated above her usual baseline. Her guardian was able to provide a limited history and informed the medical team that she had not been urinating for the past couple days. Her condition deteriorated quickly to the point where the patient had generalized, severe pain, shortness of breath, and was not responding appropriately to the guardian so she was taken to an outside clinic and ultimately transferred to KCH. When the patient arrived at short stay in KCH she was in severe distress and was not responding to questions. The patient was put on cardiac monitor that showed T wave elevations secondary to hyperkalemia. It also showed widespread ST elevation and PR depression thought to be uremic pericarditis from renal failure. Calcium gluconate was pushed peripherally for myocardial stabilization. Oxygen therapy was initiated for the shortness of breath and an insulin/dextrose drip was started to address the hyperkalemia. A foley catheter was placed to assess urinary retention vs renal failure. Once the foley was placed, there was a minimal amount of urine collected. The patient was not responding to therapies addressing her hyperkalemia as shown by the cardiac monitor. A cardiac ultrasound was done given her EKG findings which showed a mild pericardial effusion. At this point, the medical team discussed whether to put the patient on HD which was the only solution given her refractory hyperkalemia, renal failure, and probable uremic pericardial tamponade. However, given the limited resources for HD, criteria have been put in place to help determine which patients will ultimately receive this therapy. The criteria include starting HD before the age 60, social support system in place, good long term prognosis with HD, and exclude patients with heart failure. This patient had a mild pericardial effusion and there was a discussion on whether this excluded her from receiving HD because of the heart failure criterion. However, the final decision was that her heart failure was likely reversible as it was attributed to her renal failure and thus qualified her for receiving therapy. The patient had a temporary femoral hemodialysis catheter placed and she was taken for emergent HD. After HD, the patient stabilized and was in the ICU before being discharged after one week. This case illustrates how health care in Malawi must be seen at both the macro and micro level which is not usually the case in resource heavy countries like the US. Health care must be distributed in a way that maximizes care for the population rather than just the individual because the lack of resources prevents the ability for each individual to have the option of receiving full care. In the US, patients are usually the deciding factor between the medical care they receive after all of the options have been given to them. Many Malawians in need of care simply do not have this choice because resources must be shared. More criteria are being implemented that helps health care workers decide which patients will benefit most from care rather than somewhat arbitrarily choosing. In this case, the patient was very close to death but in the end she was one of the lucky Malawians who were determined to fit criteria for care.