Introduction to Orthopaedics
advertisement

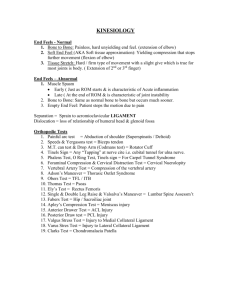
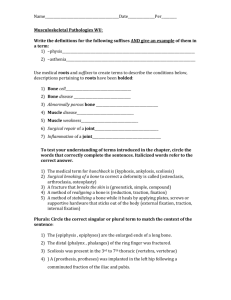
Introduction to Orthopaedics Test Yourself • List the bones of the body. (More pts more bones!) • Bone forming cells are called ______. • Local stress stimulates bone formation. T or F? • The knee is a/an _______joint. What do you know from the slides? Which is the hand of the elderly adult? A B How old do you think the individual is on slide A? Bone Structure: Nursing Implications • • • • • • Periosteum Diaphysis Epiphysis Periosteum Endosteum Epiphyseal plates; bone growth, injury What is the significance of the epiphyseal plate? Bone Formation and Maintenance • Types • Bone = cells, protein matrix, mineral deposits • Types of bone cells • Function of each type bone cell • Protein matrix: 98% collagen, 2% other • Mineral salts: insoluble Ca/Phos = hydroxyapitite + • Process of ossification Factors Influencing Bone Growth and Formation • PTH • Estrogen – What effect of low Ca? • Glucocorticoids • Calcitonin – What effect on bones – Effect on Ca? – Source? • Thyroxin with long term use of glucocorticoids? • Vit C & D Types of Joints: Identification • Amphiarthrosis • Synarthrosis • Diarthrosis Diarthroidal Joint Significance of Diarthrotic Joint • Joint Capsule surrounded by ligaments • Synovial Membrane: secretes synovial fluid; lines tendon and muscle sheaths • Bursea: painful, but protective! Othropaedic Terminology Descriptive Orthopaedic Terms • Valgus: part of body distal to joint directed away from midline • Varus: Part of body distal to joint directed toward midline • • • • • • Hallus Genu varus Genu valgus pes varus metatarus valgus metatarus varus Which foot has a valgus deformity? Hallus valgus How do you describe this foot deformity? Stressors of the Musculoskeletal System Trauma Infection Altered Metabolism For the person with a musculoskeletal condition: • List effects on PERSON • • List “most “ frequent nursing diagnosis • Peripheral neurovascular dysfunction • Pain (acute, chronic) • Impaired skin integrity • Infection, high risk for • Disuse syndrome • Activity intolerance • Trauma. high risk for • Knowledge deficit • Impaired adjustment • Fear, anxiety How has orthopedic injury affected this PERSON? Components of Assessment • Chief Complaint – Why seeking care – Acute and chronic problem •Pain • History taking; its significance • Pain characteristics – location – character – what effects • Associated conditions Complications! How will you handle this situation? • Mr J. reports to the nurse at the lealth clinic that he can no longer walk because “it justs hurts too much!” • What questions will you asks? • How will you conduct the physical assessment? Principles of Assessment • Normal first • Bilateral comparision • Test your skills – Changes with age • Inspect then gentle – Nurtitional status palpation – shape, size , contour – signs inflammation, ecchymosis – muscle condition – deformity – Skin integrity – Rashes – Color changes, esp with cold; arterial vs. venous – Character of joints – Bruises, swelling Specific Sites....... • Hand, extremities – Herberden’ nodes, Bouchard’s nodes – Subcutaneous nodules – Bursal swelling – Synovial cysts – Tophaceous cysts Deformities • Ulnar drifts • valgus and varus deformities • atrophy • hypertrophy • general hygiene Subcutaneous nodules (Rheumatoid arthritis) Urate cystals in kidney (gout) Tophaceous cysts (gout) Structural changes with osteoarthritis Herberden’s nodes Describe this deformity. What disease does this person most likely have? Assessment of the Knee • Fluid in the Knee – Bulge sign: medial aspect knee, displace fluid upward, tap lateral patellar margin and note fluid return – Ballottment:force fluid into joint space; displace patella Ballottment:force fluid into joint space; displace patella Knee Stability • Anterior cruciate ligament: limits anterior motion • Posterior cruciate ligament: limits posterior motion • Lateral collateral ligament: limits adduction • Medial collateral ligament: limits abduction • Meniscal injury: McMurray’s sign Knee Support and Stability Anterior and posterior cruciate ligaments connect the inner surfaces of the head of the femur with the head of the tibia. They cross each other, anterior ligament extend from the inside of the lateral condyle of the femur to the medial side of the tibial head, and posterior ligament extend from the inside of the medial condyle of the femur to the lateral side of the tibial head. Anterior Drawer test McMurray’s sign Diagnostic Tests • CT Scan • Bone Scan • MRI • Dual-Photon Absorptiometry • Arthrography • Arthrocenthesis • Arthroscopy Diagnostic Tests • Arthrography – Radiographic exam, use air or contrast medium:; 90-95% accuracy – Teaching – Complications: infection, allergy – Post-op: Rest joint 612 hrs, use ice • Arthrocenthesis – Aspiration synovial fluid; reduce pain; dx; treatment – Analysis joint fluid: usual clear, high viscosity, scant fluid – Teaching: no restrictions; consent form; slight pain – Post-op: RICE Arthroscopy • Therapeutic /diagnostic • Visual recording; surgical removal of meniscus, foreign bodies, etc • Rare complications; depends on procedure, operative length, use of tourniquet • Teaching • Post-op care Orthopaedic Interventions! • • • • • • Traction Casts External Fixators Pin, plates and screws CPM Crutch-walking Assistive Devices • Traction – Definition – Uses – Types • Counter traction is provided by: – – – – a. body weight b. pulleys c. traction weight d. splints • Crutch-walking – – – – – Two-point Three-point Four-point Swing-through swing-to • Safety in crutchwalking • Cane CPM • Purpose • Guidelines for Use • Teaching Bone Stimulators • Indications • Electronegativity • Bone Remodeling – Internal – Percutaneous – External External Bone Stimulator Autologous Blood Transfusions • Indications for • Criteria for Use • Ortho Cell Savers Cell Savers Autologous Blood Surgical /Medical Interventions • Tissue Allographs • Abductor Pillow, Carter Pillow • Hot Ice Machines that Aren’t! • Bone Paste! Tissue allografts, synthetic grafts Pins, plates, screws ORIF (open reduction, internal fixation) For more information on casts, traction and external fixators, return to C Morse’s Home Page Casts, Casting! • Purposes • Casting Material – Plaster – Fiberglass Casts External Fixator Application of Cast • Principles – – – – Skin Assessment Skin Protection Heat Generated Time to Dry •Cast Types • Sugar Tong/Splint • Spica Type – Body Cast – Hip spica – Gauntlet – Cast-Brace • Body Cast Care – Cast Syndrome • Hip Spica – Turning – Cast Drying Nursing Interventions • Amy, a 24 yr old is discharged from the ER with a long arm cast. – What INITIAL care? • What discharge teaching should you do? • Can you delegate this? External Fixators • How They Work • Principles of Care • The Iliazarov External Fixator