Reimbursement, demystified - American College of Radiology
advertisement

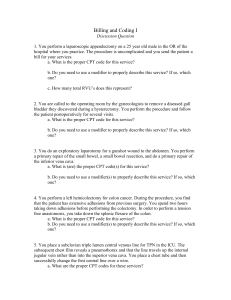
Reimbursement, demystified. Charles William Bowkley, III MD 2007-8 James Moorefield Fellow, ACR Brown University – Warren Alpert Medical School 3rd PP ACR Patient Care Radiologist CMS 3rd PP RUMC Radiologist CMS P4P Industry It’s really not that bad… I promise Introduction CMS defines rate at which you are paid Very complicated . . . You negotiate with 3rd PP What you get paid for (Procedure, E/M) How much you get paid A complex series of events determines the final outcome… Let’s address the basics… Medicare Part A – Hospital insurance • Inpt, SNF, Home Health, Hospice • Payroll taxes (FICA), Self Employed tax, RRA Part B – Medical insurance (Physician Fees) • Otpt Hospital / Physician Office, ASC, “Health prac.”, Lab/Dx services, etc. • Enrollee pymt, Fed. Revenues, Interest on B fund Part C – Medicare Advantage (MA) • Entitled to A, enrolled in B, reside in area of MA • Capitated “HMO/PPO” insurance for qualified Part D – Prescription Drug Plan Medicaid Federal financing for low income • Stringent requirements • May require co-pay • $$ paid to state health care provider, not patient Let’s walk through a simple patient encounter… 46 yo male with CC of Dyspnea HPI: 36 ppd with new onset of SOB, cough, and hemoptysis. PMH: None PSH: Appy, CCY Meds: MVI ALL: NKDA In-office CXR “nl”, CBC nl A/P: 46 yo smoker w/ hemoptysis, cough, and dyspnea. ? PNA ? CA - CT Chest I+ Follow the paper trail . . . ICD-9 International Classification of Diseases, 9thed BBA 1997 physician ordering test MUST have signs, symptoms, and possibly diagnosis 786 (Cannot specify diagnosis) Symptoms involving respiratory system and other chest symptoms 786.2 Cough 786.3 Hemoptysis CPT 99203 Detailed history, office/outpt visit Primary care physician billing 71260 CT Chest I+ Radiologist billing Gray Shield - RI C.A. 71260 CPT Current Procedural Terminology Codes and modifiers used to report services performed by healthcare providers Chosen as national standard code set Maintained by AMA CPT Editorial Panel http://www.ama-assn.org/ama/pub/category/3882.html CPT Category I Widespread use. Peer reviewed literature. Advisor support. Referred to AMA-RUC for valuation* Category II Optional, Performance measurement Decreased need to manually audit charts None created to date No payment Category III Limited dissemination Literature suggests future growth and utility. Primarily for tracking new procedures. NOT referred to AMA-RUC for valuation. • Carrier priced if covered. http://www.ama-assn.org/ama/pub/category/3882.html CPT Editorial Panel Chair: William T. Thorwarth Jr., M.D., (Former president of the ACR and former chair of the ACR Economics Commission) 18 Members 11 nominations by AMA 2 Vice-Chairmen and representative of Health Care Professionals Advisory Committee (HCPAC) 1 Blue Cross Blue Shield Association 1 Health Insurance Association of America 1 CMS 1 American Hospital Association 1 Performance Measures http://www.ama-assn.org/ama/pub/category/3882.html CPT Editorial Panel RUC Panel Advisory Committee Advisory Committee Code Application Staff Review Panel has already addressed the issue New Issue or Significant New Information Received Specialty Advisors Advisor(s) Agree No New Code or Revision Needed Staff Letter to Requestor Informing Him/Her of Correct Coding Interpretation or Action Taken by the Panel Table for Further Study March 22, 2016 Advisors Say Give Consideration Or 2 Specialty Advisors Disagree on Code Assignment or Nomenclature Editorial Panel Reject Proposal Change Add New Code/Delete Existing Code/or Revise Current Terminology 18 RUC 29 members 23 appointed by special societies Chair American Medical Association Representative CPT Editorial Panel Representative American Osteopathic Association Representative Health Care Professionals Advisory Committee Representative Practice Expense Review Committee Representative RUC Cycle Coordinated with CPT Editorial Panel schedule Required to Survey at least 30 practicing physicians **(Essential)** Recommendations presented to RUC RUC may adopt or modify before submitting to CMS RUC recommendations forwarded to CMS in May CMS meets with Carrier Medical Directors (MAC) to review recommendations Medicare Physician Fee Schedule (includes CMS’s review of RUC Recommendations) published late Fall. Valued codes from May submission reflected January 1 following year. CPT Editorial Panel RUC Panel Advisory Committee Advisory Committee Specialty Society Advisors Review New and Revised CPT Codes CPT Editorial Panel Adopts Coding Changes Codes Do Not Require New Values RVS Update Committee No Comment Comment on Other Societies’ Proposals Survey Physicians Recommended Values Specialty Society RVS Committee CMS Medicare Payment Schedule March 22, 2016 21 What is relative value ? RBRVS RBRVS: resource based relative value scale • Pressure to change Part B expenditure Phased in January 1, 1996 “Customary, Prevailing, Reasonable” • • • • Specialty specific C: Median of individual charges for a specified time P: 90th %ile of all peers in a defined area R: Lowest of the Actual, Customary, Prevailing fee RVS1 California 1956 • Based on median charges reported by C. BS Harvard RBRVS, third iteration 1985 • W. C. Hsiao, MD & P. Braum, MD • Phase I » 18 medical specialties • Phase II » 15 additional specialties • Phase III / IV » Include remaining services coded by CPT 2 RVS Include 3 main variables 1. Relative Physician Work (52%) 2. Practice Expenses (44%) 3. Professional Liability Insurance Costs (4%) Modifiers 1. Adjust for geographic locale 2. Different specialty, same service = same payment 3. “Budget Neutral” conversion factor (CF) (Would not change Medicare spending -/+) 4. Include process for annual update in CF 5. Limits on Balance billing 6. Medicare Volume Performance Standard (SGR) ICD-9 CPT PC/TC 786.2 71260 786.3 Black Box 55.36 / 263.79 PAYMENT (Physician Component) Total RVU = Conversion Factor * (_____) CF * Work: (Work RVU x Work GPCI) + PE: (PE RVU x PE GPCI) + PLI: (PLI RVU x PLI GPCI) + CF * [(Work RVU * Work GPCI) + (PE RVU * PE GPCI) + (PLI RVU * PLI GPCI)] Technical Component MPFS (RVU PE *GPCI(PE) + RVU PLI *GPCI(PLI)) * CF HOPPS (APC) Payment Rate * Wage Index (Regionally Calculated like the GPCI) How did we arrive at these calculations? “Lawmakers See Red Over Meat Packaging” “…warn consumers to discard any product with an unpleasant odor, slime, or a bulging package.” - USA Today, 10/31/2007 Pretty Good Advice!!! MPFS RVU CPT WORK PE PLI Global Billing Professional Component “Attempt to devise the best payment system” Technical Component HOPPS APC PAYMENT RATE Physician Work Time to perform service Technical skill and effort Mental effort and judgment Psychological stress of iatrogenesis Currently Based on: ACR Socioeconomic Supplemental Survey Data Historically Based on: Harvard RBRVS study 1992 RVS Refinement Process AMA/Specialty Society RVS Update Process Physician Expense What it costs the “Practice” to run: Rent, Wages, Equip. / Supplies Practice Expense Advisory Committee (PEAC) ACR Socioeconomic Monitoring System Supplemental Survey Data Clinical Practice Expert Panels (MD’s) • Data for constructing cost estimates • In/Direct cost elements for a service • Estimates extended to related codes in CPT family CPEP Technical Expert Group • Monitor data collection process AMA Socioeconomic Monitoring System Data Common service provided only by X (Avg. Medicare 1991 payment $100), the percentage of PE cost for the given specialty X (Y%), multiply that number by the $100 cost and you get Y (Initial Dollar) RVU’s. Equipment Utilization and Interest Rate (Technical Component (Included in Physician Expense RVU) ) [1/(minutes per year * 50% usage)) * Price * ((11% interest rate/1) (1/(1+ 11% interest rate) * life of equipment)) + 5% maintenance] Courtesy of Pam Kassing Physician Liability Insurance Initially: Omnibus Budget Reconciliation Act 1989 Now.. • • • • • Calc. average professional liability premium Calc. risk factor based on specialty Mult. % of service (CPT based) by risk factor Mult. By Work RVU Rescale for budget neutrality ( x Fudge Factor) GPCI “Gypsie” Geographic practice cost indexes AMA SMS 1987 survey Must be updated Q 3 years Changes phased in over a two year period Cost of living: 1990 census college grads, 2000 professional organizations, updates since…. Inputs to medical practice varied by geographic locale Premiums for policy 1 mil/ 3 mil Conversion Factor Updated yearly based on BBA 1997 CFx = CFx-1 * MEIx * UAFx * LCx * BNx MEI: Medical Economic Index Measures average price change for medical goods/services with respect to inflation UAF: Update Adjustment Factor Comparison of actual and target Medicare expenditure. Designed to prevent unsustainable increases in Medicare expenditures. LC: Legislation Change BN: Budget Neutrality So, how does it all add up? Example: CT Chest I+ 712602008 [(Work RVU x Work GPCI) + (PE RVU x PE GPCI) + (PLI RVU x PLI x GPCI)] x CF Work ((1.24) x Budget Neutrality Adjuster (0.8816)) , PE(0.44), PLI (0.05), CF(34.0682) RI = (((1.24 x 1.045 x 0.8816) + ((0.44 x 0.991)) + ((0.05 x 0.895)) x (34.0682)) = $ 55.36 Ca (SF) = (((1.24 x 1.060 x 0.8816)) + ((0.44 x 1.546)) + ((0.05 x 0.640)) x (34.0682)) = $ 63.71 Technical Component MPFS (RVU PE *GPCI(PE) + RVU PLI *GPCI(PLI)) * CF RI: (7.48 (0.991) + 0.37(0.895)) * 34.0682 * = 263.79 CA(SF): (7.48 (1.546) + 0.37(0.640)) * 34.0682 * = 402.00 HOPPS (APC 0283): Payment Rate * Wage Index(2006) RI: 289.71 * 1.0954 = 317.35 CA(SF): 289.71 * 1.4974 = 433.81 MPFS RVU CPT WORK PE PLI Global Billing Professional Component Technical Component HOPPS APC PAYMENT RATE OK, now I understand… But what is the big picture? Adapted from Woody, I. O. JACR 2005; 2(2):139-150 Courtesy of CMS and H. Forman, MD Courtesy of CMS and H. Forman, MD What can we do… Well, all politics is local . . . Local Medicare Carriers W A Noridian MT h OR Noridian BC/BS of MT National Heritage ND WY Noridian WI WPS SD CIGNA National Heritage Insurance Company VT NM Empire NH NY MA BC/BS of Group Western NY Health CT RI (BC/BS WPS Noridian ID MI WPS Noridian NV NE BC/BS of KS Noridian UT In National Heritage Insurance Company Noridian Noridian CO KS BC/BS of KS CA Noridian AK AZ BC/BS of AR OK NM BC/BS of AR IA Noridian IL WPS BC MO / BS BC/BS of of AR KS Trailblazer AK IN AdminaStar KY Trailblazer AdminaStar BC/BS of AL Cahaba (Cahaba Gov. Ben. Gov. Ben. LA Admin Admin) BC/BS of AR AL MS of AR) PA HGSA of PA OH Palmetto Gov. Ben. Admin. WV Trailblazer TN CIGNA AR BC/BS of AR TX Noridian ME MN NJ Empire DE Trailblazer MD DC VA NC CIGNA Palmetto Gov. Ben. Admin. GA SC Cahaba Gov. Ben. Admin FL First Coast Service Options HI First Coast Service Options Noridian July 6, 2006 MAC All politics is local….. >90 % Of Coverage And Payment Decisions Occur At The Local Level Each MAC is required by CMS to have a physician Contractor Medical Director (CMD), who must follow the Coverage Issues Manual, Program Memoranda and other transmittals from CMS defining the CMS national policy for Medicare reimbursement ACR involvement helps prevent the spread of reimbursement policy damaging to radiology between contractors CMS gives authority to the local contractors to determine under what conditions a service is considered medically necessary and claims may be denied if not appropriate. In most states the CMD has the ultimate authority to determine medical necessity Adapted from John Patti, MD CMS Radiologist State MAC (MD) CAC Rep CPT RUC ACR Local Coverage Determination LCDs are produced by CMDs to inform providers of the local Medicare reimbursement rules and the medically necessary reasons for an examination or procedure LCDs are created for certain CPT codes or a group of CPT codes (with associated ICD-9 codes and established diagnoses) required when submitting a Medicare claim Procedure Description, Reasons For Denial, and Coding Guidelines are omitted from LCDs and published in separate supporting articles by the Contractor New LCDs and supporting articles must be posted for public comment prior to integration; this period is 45 days Traditionally contractors have been receptive to comment on both the LCDs and supporting articles Adapted from of John Patti, MD Lines of communication Managed Care Committee / Network 3rd Party Payer Courtesy of Bibb Allen, MD Carrier Advisory Committee Network Diagnostic Radiology, Radiation Oncology, Nuclear Medicine, SIR CAC, RBMA CAC Network Link between Medicare Carrier and general membership by ensuring that local policies appropriately represent practice of radiology CPT III Codes specifically ** Staff assist CAC representative in evaluating Local Coverage Determinations (LCDs) Why all the doom and gloom? The Perfect Storm 1. DRA 2. Contiguous Body Part Imaging 3. 5 Year Review 4. The calm _____________ the storm….. Deficit Reduction Act of 2005: Section 5102(b) limits TC payment for imaging in physician offices or imaging centers on/after January 1, 2007. TC capped at the lesser of the Medicare physician fee schedule payment rate or the Ambulatory Payment Category (APC) rate under the hospital outpatient prospective payment system (“HOPPS”). Includes X-ray, ultrasound (including echocardiography), nuclear medicine (including PET), MRI, CT, and fluoroscopy, Excludes diagnostic and screening mammography Professional Component is not affected Congressional Budget Office (CBO): $2.8B savings over the next 5 years ACR staff: $1.2 B savings in first year alone CBO new score at $13B over 10 years Deficit Reduction Act The imaging provisions are a public policy disaster FALSE: Wide variance of payment between hospital outpatient based imaging services and imaging provided in physicians offices/imaging centers TRUTH: Study done by The Moran Company shows a variance across all imaging modalities of 3% Provisions written without input from the imaging community, without Congressional hearing, without accountability to its authors No one takes responsibility for authorship Eliminates RBRVS and takes lower of payment between the MPFS and HOPPS DRA Impact Financial Impact Breakdown By Procedure Percent Reduction MRI 35 % US 30% Nuc Med 16% CT 9% MRA 25% CTA 37% Lost Imaging Revenue 490 M 300 M 136 M 69 M 24 M 10 M DRA Impact Biggest Hits by Lost Revenue MRI Brain MRI Spine Myocardial Perfusion SPECT Carotid Artery Duplex Echocardiography Color Doppler PET and PET/CT $162 M $90 M $132 M $87 M $83 M ?? Multiple Procedure Discount For Contiguous Body Parts CMS Regulation Continues the reduction for the second and subsequent examinations at 25% in 2007 At the urging of ACR, CMS did not increase the reduction to 50% – Any savings from multiple examinations goes back to the federal fund – Application of the reductions to the HOPPS rate would result in 75% reductions for the second procedure in some cases CMS will apply the 25% reduction to the MFS payment rate and if that payment is higher than the HOPPS payment, the HOPPS payment is paid The Third 5 Year Review Budget Neutrality Section 1848 (c) (2) (B) (ii) (II) of the Social Security Act requires that adjustments in RVUs may not cause total Medicare Physician Fee Schedule payments to differ by more than $20 million When this tolerance is exceeded CMS must make a budget neutral adjustment The Third 5 Year Review Mandated process for Medicare to review overvalued and undervalued CPT codes (Via evaluation of RVU’s). Over 160 high utilization codes were reviewed, 40 pertaining to radiology Major change was 20% increase in E/M value, resulting in greater than $4 billion budget neutral effect Incidentally, Anesthesia work value inc. 32% - this is reflected in the Budget Neutrality Adjustment in 2008 Final Rule The Third 5 Year Review Budget Neutrality Adjustment For Physician Work RVUS Vigorously opposed by the ACR Vigorously opposed by the RUC and almost all medical specialties Reasons For ACR Opposition Major impact on hospital based physicians This is a historical precedent for changing the CF The Third 5 Year Review Enter the Budget Neutrality Adjustment… Professional Component (PC) Payment (RVUxGPCI) +(RVUxGPCI) + (RVU+GPCI) * CF (RVUxGPCIx.8816) +(RVUxGPCI) + (RVU+GPCI) * CF CMS has finalized its 32% increase for anesthesiology physician work values as part of the third 5 year review. The physician work adjustor will cause the 10.1% cut in physician work values for 2007 (with a work adjustor of .89896) to be increased to a 11.94% cut (changing the work adjustor to .8816) to all physician work values in the physician fee schedule for 2008. Conversion Factor Calculated each year based on a statutory formula that centers around the Sustainable Growth Rate - a.k.a. SGR SGR components Medical economic index - a.k.a. MEI Volume of services in prior years Target volume of services based on the Medicare population Gross domestic product SGR now demanding decreases in the conversion to achieve the target rates Five years of fixes leaves a large amount to repay to the system We are at the cliff and if the SGR formula is not changed double digit reductions in the CF will occur Decreases 10.1% for 2008 to $34.0682 ACR Policy Priorities Co-founder of Access to Medical Imaging Coalition (AMIC), ACR will urge AMIC to support Accreditation as a means to address rapid growth in utilization http://www.imagingaccess.org/ ACR will support participation in Accreditation programs BY ANY PHYSICIAN SPECIALTY who commits to quality and appropriate use of imaging studies and further, the ACR will support Medicare development of Accreditation requirements/Appropriateness criteria based on private sector/physician specialty societies programs AMA and medical community pushing for comprehensive legislation to fix or replace the SGR focusing on those changes not adversely affecting radiology Because the increase in imaging utilization by ~14% is seen as a driver of SGR spending, radiology remains in the crosshairs Extensive congressional lobbying with bipartisan co-sponsors re: DRA moratorium bills filed in 2006 and 2007 Advocacy to CMS on contiguous imaging reduction – prevented a 50% cut for 2007, continue to defend TC from attack Advocacy to CMS on need for valid survey data on equipment utilization rate – CMS proposed to hold rate steady for 2008 Final Rule for 2008 Conversion Factor for HOPPS payments will increase by 3.3% CMS is proposing not to pay separately for the hospital TC of codes that they describe as dependent items and services HOPPS All imaging guidance, supervision, and interpretation (S&I) codes would be bundled into the procedure codes and, also Intraoperative services such as ultrasound would be bundled into the procedure code Image processing services – 3-D post processing would not be paid separately Contrast material and radiopharmaceutical cost will not be paid separately Conversion Factor for MPFS payments will decrease by 10.1% MPFS Anti-Markup Language – if you bill Medicare $50, they will ONLY pay you $50…. Under Arrangements – no joint venture participation by hospitals and referring MD’s ACR lobbied heavily for the Radiology Practice Expense / Hour increase to $204.86 MPFS Final Rule for 2008 Practice Expense Methodology Practice expense per hour (PE/hr) is amount it costs radiology practices in indirect/overhead to run an office or imaging center per hour. One of only a few specialties to conduct an alternate survey to re-calculate PE/hr – original CMS Socioeconomic Monitoring Survey assigned $54/hr to radiology ACR survey to replace SMS survey was miscalculated by CMS contractor (Lewin) at $174 PE/hr ACR vigorously challenged Lewin – CMS agreed In 2008 CMS will correct the radiology PE/hr to $204 – $100m shift to radiology Will partially balance the DRA effects and CF changes Courtesy of Pam Kassing Future • Equipment Utilization • Interest rate for equipment debt • Practice Expense • CF • P4P • Radiology Utilization Management Companies – “Steerage”, Pre-Auth. • Assume no DRA moratorium • Comparative Effectiveness Future • Leasing Arrangements • Resolve Reimbursement Issues for use of RA’s • More self-referral regulations and Stark III • Fixing the SGR formula and how the conversion factor is calculated • Continue to work with private payers to address similar issues Courtesy of Pam Kassing Special Thanks and Attributes to… John Patti, MD Bibb Allen, MD Howard Forman, MD Pam Kassing Maurine Spillman-Dennis Diane Hayek Anita Pennington Kathryn Keysor Helen Olkaba Evelyn GIlbert Thank You ! Thoughts, Questions, Concerns. . . Cbowkley@gmail.com