Business Concepts in Radiology - Where does the money come
advertisement

Where does the money come from
in Radiology?
An Application of Relative Value Units (RVUs)
A Special Thank You to:
Dr. David M. Yousem, M.D., M.B.A. Professor, Department of
Radiology Vice Chairman of Program Development Director of
Neuroradiology Johns Hopkins Hospital
for allowing the use of his material/content in this presentation
Dr. Yousem’s online lecture series can be viewed at:
http://webcast.jhu.edu/mediasite/Catalog/pages/catalog.aspx?catalogId
=7e18b7d5-9c63-487e-aaf1-77a86f83b011
Dr. Yousem’s project was funded through an RSNA Educational Grant
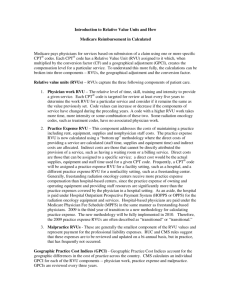
Relative Value Units and the RBRVS – A Brief Review
• RVUs are assigned to specific CPT codes
• The total radiology bill has two components
– Technical Fee
• Paid to the facility (owner/operator of the equipment)
– Professional Fee
• Physician Work, Practice Expense, and Malpractice Expense
• RVUs do not translate directly into money
– Modified by geographic and budgetary multipliers
– Money Paid = (RVU x GPCI) x Conversion Factor
Medicare – There are (usually) two bills for every study
•
•
•
•
Medicare Part A
– Submitted by the “facility” performing the study
– Technical component
Medicare Part B
– Submitted by the interpreting physician
– Professional component
Patient pays 20% of both bills, Medicare covers 80% of both
– The patient may have supplemental insurance to cover their 20%
Global Reimbursement
– For the freestanding entity that may bill for both the technical and
professional components of the CMS Physician Fee Schedule under
Medicare Part B
Follow the Money
• Over the next few slides we will create a simplified example of
the reimbursement process
• Certain assumptions will be made to facilitate understanding the
numbers on a fundamental level
• As always, reality is much more complicated
• To start, we will try to answer the following question:
– How many studies do I have to read each day to make
$300,000 in a year?
Follow the Money – Assumptions
• Net payment per RVU of $30
– This allows for incomplete collections in a mixed payer population
– Calculated across all departments within a practice
• Goal personal income of $300,000
– Benefits amount to 25% of salary
– Malpractice costs are $25,000 (high end of the scale)
– Cash allowance of $10,000 (meetings and travel)
– Practice Expenses of 35%
• Based on survey data from the ACR and median reported
expenses per FTE radiologist
Follow the Money – Assumptions continued
• Work Days
– 250 workable weekdays a year
– 50 days for vacation and/or meetings
– 5 weekends of coverage
– Total of 220 work days
• CMS Physician Fee Schedule RVU files for 2010
• Geographic Practice Cost Index (2010)
– GPCI (physician work) in North Carolina is 1.0
• Conversion Factor (2010)
– $36.0846
Follow the Money – The Challenge
• Our hypothetical radiologist must produce $515,000 in a year
– This covers his salary, group benefits, and expenses
– Stated another way
• $2,341 a day
Follow the Money – The Details
•
Using the CMS formula for reimbursement
$ = RVUprofessional x GPCI x CF
•
We break it down into parts
– In our case, the payment per RVU reflects the GPCI and CF modifiers
$510,000 = Payment per RVU x RVUtotal
RVUtotal = Sum of {RVUstudy x Number of each type of study}
•
To break it down further into the workload required in a single day
$510,000 / 220 days = $2,341/day
Number of studies = $2,341 / (RVUstudy x Payment per RVU)
Follow the Money – The Details
• The previously described equations are calculated to show how
many of one specific study (e.g. Chest Radiographs) must be
read in a single day to meet the goal income
• Calculating a mix of studies is simple, but less illustrative
Follow the Money – The Work
•
•
Using only the professional
component of reimbursement,
these are the numbers of each
type of study you would have to
read in a single day to produce
$2,341 of income for your
practice
Specifically, if you are a
neuroradiologist, and only read
noncontrast Head CTs, you
would have to interpret, and be
reimbursed, for 68 exams to
meet your goal
Exam
RVU
(prof)
Number /
Day
CXR (2 view)
0.3
260
CT Head wo
1.14
68
CT A w/wo
1.89
41
MR Head w/wo
3.18
25
MR Knee wo
1.86
42
Xray Hand
0.24
325
US Abd Complete
1.09
72
NM HIDA
1.11
70
Follow the Money – Own the Equipment
•
•
•
The aforementioned examples
are for reimbursements with only
the professional component
The technical component of
reimbursement reflects 85% of
the global bill compared to the
professional component’s 15%
Here are the numbers again
when receiving the global
reimbursement (e.g. if all
imaging was performed at your
outpatient imaging center)
Exam
RVU (prof)
# / Day
RVU (global)
# / Day
CXR (2 view)
260
103
CT Head wo
68
22
CT A w/wo
41
10
MR Head w/wo
25
6
MR Knee wo
42
9
Xray Hand
325
96
US Abd Complete
72
22
NM HIDA
70
10
Conclusions
• Study volume is important to produce revenue
• So are your payer mix and contracts
– Medicare vs. Medicaid vs. Private Insurance
• Efficiency in Billing and Collections is essential to actually receiving
the revenue you have “earned”
– Accounts Receivable is an critical asset (see Accounting)
• Owning the equipment is crucial
– This is the basis of turf wars between radiology and some other
clinical subspecialties
– ACR has ongoing legislative efforts at closing Stark law
loopholes
The Big Picture
•
•
Managing a practice with multiple radiologists exponentially increases
the complexity of generating and measuring income
– Referral Base influences the RVU calculations and billing
• Inpatient vs. Outpatient and Medicare vs. Private Insurance
• Hospital vs. Imaging center vs. Physician Office
– Productivity Measurement and other Metrics
As well, there are many facets to both Accounting and Expenses
• Capital Purchases
• Marketing
• Technology
• Medicolegal and Legislative Issues