AUA Course
advertisement

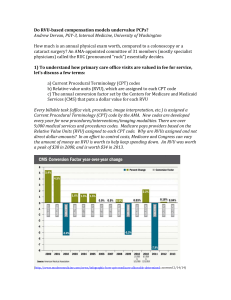
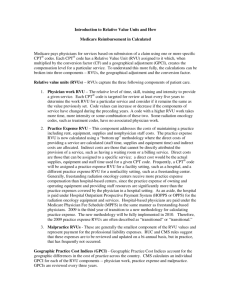
AUA Health Policy Basics Course National Health Policy Organizations • The RUC meeting, convened by the AMA, evaluated 4 new CPT 1 codes to determine their RVU. CMS approved the panel recommendations; however stated that the GPCI and the PLI portion of the RVU will be modified. The CY 2012 CF was calculated at $24.67. • Studies by the AHRQ and IOM were included in a MEDPAC report to Congress. A key quality issue related to Medicare part B was identified. The AUA, AACU, and LUGPA discussed. The AUA QIPS committee worked with the SQA and the ACS through the PCPI to develop a new measure. The measure was approved by the NQF. Overview • Government Health Insurance – Structure and Reimbursement Process • Quality Improvement Initiatives and Organizations • Physician Organizations Government Health Insurance Structure and Reimbursement Process Medicare • Health Insurance for the Aged Act – Johnson Administration 1965 • Health insurance for Seniors – Nixon Administration 1972 • Patients with renal failure and chronic disability – Includes 17% of all beneficiaries in 2011 – Seniors qualify for benefits by paying at least 10 years (40 quarters) of payroll taxes • Premium required for non-qualifiers Medicare • Part A – Hospital Insurance program • Acute inpatient stays, skilled nursing facilities, hospice, home health services • Funded by mandatory payroll taxes (workers and employers) – Eligible Medicare beneficiaries automatically enrolled • No co-pay but annual deductible • Part B – Supplementary Insurance Program • Physician services, supplies, outpatient and ambulatory care, durable medical equipment, and laboratory services • Voluntary program – Premium and deductible Medicare • Part C – Medicare Advantage (MMA 2003) • Private insurance distributes Medicare Part A, Part B, and an equivalent to Part D with option of “advantage” – HMO, PPO, PFFS plans • Part D – Subsidized prescription medication coverage • Voluntary – Variable co-insurance rate drug costs > $310 annually • “Doughnut hole” Medicaid • Title XIX Amendment to Social Security Act 1965 • Means tested health care benefits – Primarily state managed • Federal fund distribution based on state needs assessment and compliance with federal oversight • Inpatient, outpatient, nursing home, drug benefit • Special Considerations – Dual eligible (Medicare and Medicaid eligible) – Children • SCHIP or CHIP (Children’s Health Insurance Program) Medicare Payment Advisory Commission (MEDPAC) • Balanced Budget Act of 1997 • Advisory group to Congress on payment and quality of the Medicare program; makes nonbinding recommendations – 17 members with staggered three year terms • 2 practicing physicians • Broad oversight and mandate – Access, quality, payments to private insurance, GME payment recommendations Center for Medicare and Medicaid (CMS) • Previously known as HCFA (Health Care Financing Administration) – Changed name to CMS in 2001 • Head of CMS is a presidential appointee • Administration, coordination, and oversight of Medicare and Medicaid – Interprets and implements Congressionally passed health care law through issuance of regulation for both programs in the federal register Common Procedural Terminology (CPT) • Descriptive terms and identifying codes for reporting of provider services and procedures – Adopted by CMS in 1983 as official Healthcare Common Procedure Coding System (HCPCS) • Five digit numeric or alpha numeric codes – CPT 1 • Well established service or procedure • Reimbursed for this service or procedure – CPT 2 • Data collection, measure performance – CPT 3 • Temporary codes used to assess emerging technology Common Procedural Terminology (CPT) • Evaluation and Management (E&M) codes – Patient encounters • Office, hospital, consults (new or established) • Codes 99201 – 99499 • Procedure codes – Diagnostic and treatment codes • Surgical, anesthesia, radiology, laboratory • Urology specific codes 50010 – 55899 – Cystectomy (51596), Cystoscopy (52000) • Modifiers – E&M and Procedure codes • Lengthy discussion (E&M) • Two surgeons, need for assistant surgeon (procedure) • Global period International Classification of Disease (ICD) • First developed by World Health Organization in 1948 – Official use in the United States started in 1989 – ICD – 9 CM (9th revision) (Clinical modification) • 10th revision planned October 2014 • Codes represent signs, symptoms, complaints, diagnosis – Justify medical necessity for the patient encounter • Code specificity – Three to five digits • Bladder neck obstruction 596 • Renal mass 593.9 • Urinary frequency 788.41 Relative Value Scale (RVS) • Links monetary value to a CPT 1 code for provider reimbursement – Government reimbursement system • Resource based relative value scale (RBRVS) – Developed by statistician William Hsiao (1985) • Medicare adopted in 1992 – Private insurers begin to use 1995 – Modified RBRVS • Process where relative value unit (RVU) are updated and adjusted CMS Payments Surgery vs. Office Visits 1990-2011* *US Bureau of Labor Statistics $1.00 in 1990 = $1.68 in 2011 Procedure 1990 2011 1990 Inflated to 2011 TUR Med BT 52235 $ 689 $ 299 $ 1,158 - 74% TUR Prostate 52601 $ 949 $ 864 $ 1,594 - 46% ESWL 50590 $ 967 $ 584 $ 1,625 - 64% Inf. P. Prosthesis 54405 $ 1,871 $ 838 $ 3,143 - 73% Radical Neph 50230 $ 1,901 $ 1,325 $ 3,194 - 59% Rad Ret Prost 55845 $ 2,331 $ 1,695 $ 3,916 - 57% Rad Cyst/loop 51595 $ 2,882 $ 2,267 $ 4,841 - 53% E&M New Pt 99203 $ $ $ + 23% 50 103 84 2011 % Change from Infl 1990 Medicare Physician Payment Scale • Work RVU component (52%) – Time, skill, stress, intensity, risks • Practice expense RVU component (44%) • Staff, supplies, rent • Malpractice RVU component (4%) – Professional liability insurance (PLI) • Multiply total RVU by a conversion factor (CF) for monetary value Medicare Physician Payment Scale RVU Work x Geographic Practice Cost Index (GPCI) + RVU Practice Expense x PE GPCI + RVU Malpractice x PLI GPCI Total RVU Dollar amount for service: Total RVU x CF for CY 2012 ($24.6712) = Payment Relative Value Scale Update Committee (RUC) • Peer review group convened by the AMA – Payment for service determined by this committee • Multispecialty representation – 31 seats • CMS triggers for RUC review – New technology – Volume (billed > 500,000 per year) – Billed 75% of the time with another code (bundle) – CMS specific request (fast growing) Relative Value Scale Update Committee (RUC) • Specialty survey data acquisition from membership – Compile data into a case to retain reimbursement • Determine physician work and practice expense component of the RVU • Specialty presents proposed RVU of the service to the RUC • CMS involved in the peer review process Recovery Audit Contractor (RAC) • Medicare Modernization Act of 2003 – Recover improper Medicare payment claims • Initial demonstration program involving five states recovered nearly 700 million dollars • Private contractors hired by CMS to “audit” physician offices or practices – Medicare Part A and B billing • Award up to 12.5% of dollars corrected • FY 2010 - 92.3 million dollars discovered in improper payments – 82% overpayment and 18% underpayment Recovery Audit Contractor (RAC) • CMS must approve potential issue raised by RAC – CMS oversight of process through RAC data warehouse • Review process – Automated review • Analytics used to review claims – Complex review • Review medical records on site • If overpayment is determined a “demand letter” is sent to the institution – Appeals process Quality Improvement Initiatives and Organizations Physician Consortium for Performance Improvement (PCPI) • National physician led effort to improve health care quality, patient safety, efficiency – Over 70 medical specialties involved • Convened and staffed by the American Medical Association – Evidence based physician level measure development • Identify areas of quality improvement with specialty collaboration • Vote on proposed measures National Quality Forum (NQF) • Formed in accordance with National Technology Transfer and Advancement Act of 1995 – Voluntary, consensus-based organization, formed to endorse existing measures after expert panel and member review – Health care stakeholders • Eight councils over 300 members – Professionals, public health, consumers, purchasers, industry • NQF approved measures “special status” – PCPI vetted measures Institute of Medicine (IOM) • Health arm of National Academy of Sciences – Independent not for profit organization – Mission is to “serve as an advisor to the nation to improve health” • Provide evidence based “unbiased and authoritative advice” for private and public health care sector • Quality related tasks commissioned and sponsored by government, industry, independent foundations • Volunteer members – Peer review system Agency for Healthcare Research and Quality (AHRQ) • Agency within the Department of Health and Human Services – FY 2010 budget 372 million dollars • 80% of budget supports research grants and contracts towards improving health care • Mission is to improve health care quality, improve safety and outcomes, reduce cost – Portal for consumer / clinician information – Health information technology research • Mandated role to support the US Preventative Services Task Force United States Preventative Services Task Force (USPSTF) • Independent panel of primary care experts in evidence based medicine – Family practice, pediatricians, nurses, behavior specialists • Review evidence of effectiveness and develop recommendation statements – Grades A through D and I • Recommendations provided for consumption by physicians, health care systems, and health insurance – Affordable Care Act 2010 • PSA screening is now a “D” – Discourage the use of this service Quality Alliances • Surgical Quality Alliance (SQA) – Alliance of surgical specialties and anesthesia • Quality measurement and improvement initiatives • Ambulatory Care Quality Alliance (AQA) – AAFP funded by America’s Health Insurance Plans • Collaborative of physician groups, health insurance plans, consumers, AHRQ • Hospital Quality Alliance (HQA) – Collaborative of public and private stakeholders • Data acquisition and reporting, measure development Physician Organizations Physician Organizations • American Medical Association (AMA) – “Promote the art and science of medicine” • Political advocacy organization – Steward organization for the CPT,RUC,PCPI – Membership • < 18% of US physicians currently members – 30% of members are students or residents • American College of Surgeons (ACS) – Largest surgical specialty organization • > 77,000 members (2600 fellows) – Cancer and trauma care, CME, data registry, SQA steward – Political advocacy organization Urology Organizations • American Urological Association (AUA) – Founded in 1902 • FY 2010 budget 30 million dollars – Three entities with one board (2001) • AUA Education and Research 501(c)(3), AUA Inc. 501(c)(6), AUA Foundation 501(c)(3) – Eight geographical sections • American Board of Urology (ABU) – “Mission is to act on the behalf of the public to ensure high quality, safe and efficient practice of Urology” Urology Organizations • American Association of Clinical Urologists (AACU) – Goal is to protect the professional autonomy of urologists • Inform members of issues and create ability to organize • Work with state societies and specialty coalitions to protect interests of urology • Large Urology Group Practice Association (LUGPA) – Association of groups with > 10 practicing urologists – Business operations, clinical outcomes benchmarking, clinical trials, educational programs • Political advocacy Urology Organizations • UROPAC (Urology Political Action Committee) – Organized in 1992 and since 2003 jointly sponsored by AUA and AACU – Support key lawmakers in health policy and advocates for Urology specific issues – 2010 election cycle raised over one million dollars