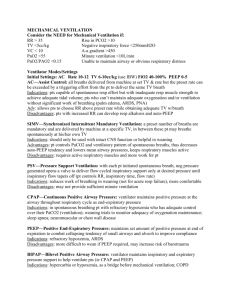
MECHANICAL VENTILATION
advertisement

بسم هللا الرحمن الرحیم نگرشي گذرا بر اصول و مباني كار ونتیالتورها )دستگاههاي تهویه مكانیكي( MECHANICAL VENTILATION Dr.Jarahzadeh Intensivist Mechanical Ventilation This is Positive Pressure Ventilation “Regular” breathing is negative pressure ventilation Airway Pressure If we measure the pressure in the tubing at the end of expiration, it will be barometric pressure. (To make it easier, we call it “zero”) Inhalation generates a negative pressure so that air will flow from “zero” to “negative” Machines generate a postitive pressure so that air will flow from “positive” to “zero” Pressures PEAK INSPIRATORY PRESSURE (PIP) • PIP: Pressure at end of active inspiration necessary to overcome airway resistance (flow resistance) and lung compliance (tissue resistance) • Airway resistance can increase work of breathing • PIP reflects both airway tone and lung stiffness increased by bronchospasm and/or atelectasis Peak Pressure (Ppeak) PPeak = PPlat + PRes Where PRes reflects the resistive element of the respiratory system (ET tube and airway) PLATEAU PRESSURE • Pressure required to overcome tissue resistance and inflate alveoli • Measured via 2 second pause at end inspiration • Gas flow ceases • Static pressure measurement • General measurement of lung stiffness PPlat Measured by occluding the ventilator 3-5 sec at the end of inspiration Should not exceed 30 cmH2O PIP: Pressure compliance resistance volume flow PEEP PEEP time No active breathing Treats lung as single unit PIP resistance flow Pplat end-inspiratory alveolar pressure Flow=0 compliance tidal volume PEEP Respiratory System Compliance Cs = Correct for gas compression Tidal volume PPlat - PEEP Total PEEP Cd=TV/PIP-PEEP Decreased with: • • • • • • congestive heart failure ARDS atelectasis consolidation fibrosis hyperinflation • tension pneumothorax • pleural effusion • abdominal distension • chest wall edema • thoracic deformity normal 80-100 mL/cm H2O Compliance pressure (Pplat) • Represent the static end inspiratory recoil pressure of the respiratory system, lung and chest wall respectively • Measures the static compliance or elastance ΔPeso ≈ ΔPpl Benditt, Respir Care 2005; 50:68 PIP Crs = Ppl (Peso) Ccw = tidal volume Pplat - PEEP tidal volume Peso Palv (Pplat) CL = tidal volume (Pplat – PEEP) - Peso In clinical practice Ccw ignore due to large size Inspiratory Resistance Ri = Increased with: PIP - Pplat flow measure with 60 L/min (1 L/s) constant flow • Secretions • Bronchospasm • Small endotracheal tube Normal: 5 - 10 cm H2O/L/s for intubated ventilated adults flow Auto -PEEP inhalation Flow and RR and Ti/Te time 0 auto-PEEP exhalation History 780 1530 paracelsus pulmator 1907 druger denhart 1945(iron lung) 1981microprocesores (pnumatice chang to electeric & electeronic) Paracelsus (1493-1541) used ‘Fire Bellows’ connected to a tube inserted into patient’s mouth as a device for assisted ventilation. This was the first study (1550) which credited him with the first form of mechanical ventilation. Fire Bellows’ Draeger Pulmotor Alfred f.jones (1864) PPV-NPV گروه بندي کلی ماشینهاي مكانیكي فشار منفي -فشار مثبت An iron lung in use (1960) معایب ونتیالتورهای با فشار منفی - حجم زیاد توجه زیاد به قفسه سینه تا ریه ها کاهش شدید مراقبت های پرستاری القائ فشار منفی روی قلب و عروق عدم رعایت بهداشت کاهش تحرک بیمار زخم بستر و فشاری نا کارامدی در ریه های سخت و فیبروزه Lung Functions Oxygenation Ventilation Neurohormonal DEFINITIONS • Ventilation: Movement of Air Into and Out of the Lung (Breathing) • Respiration: Extraction of Oxygen from Inspired Air and Release of Carbon Dioxide (Gas Exchange) 1.Internal 2.external CLINICAL OBJECTIVES OF MECHANICAL VENTILATION Provides Supplemental Oxygen and remove Waste Product of metabolism ( CO2 ) Unloading ventilatory muscle (Keep WOB reasonable) Recruits Collapsed Alveoli to Support Respiration • Increases Functional Residual Capacity (FRC) Keep lungs adequately inflated Ventilate safely and avoid complications Achieve patient/ventilator synchrony with minimal sedation and no paralysis Mechanical Ventilation ... is a therapy. What are the indications? How do we administer it? How do we assess it? What is the end point? In USA: 1-3 million need MV outside operating room 50/000 ventilator Indications for Mechanical Ventilation Acute Respiratory Failure (66%) Acute Respiratory Distress Syndrome Heart Failure (through pulmonary edema/hypertension) Pneumonia Sepsis Complications of Surgery Trauma Coma (15%) Acute Exacerbation of Chronic Obstructive Pulmonary Dz (13%) Neuromuscular Disease (5%) Esteban A, Anzueto A, Alia I, et al. How is mechanical ventilation employed in the intensive care unit? An international utilitzation review. American Journal of Respiratory Critical Care Medicine 2000; 161: 1450-1458 Discontinuing Mechanical Ventilation Death Weaning Up to 25% of patients have respiratory distress severe enough to require reinstitution of ventilator. Extubation 10 - 20 % of extubated patients who were successfully weaned require reintubation. Brochard L, Rauss A, Benito S, et al. Comparison of three methods of gradual withdrawing from ventilatory support during weaning from mechanical ventilation. American Journal of Respiratory Critical Care Medicine. 1994; 150: 896-903. Esteban A, Frutos F, Tobin MJ, et al. A comparison of four methods of weaning patients from mechanical ventilation. New England Journal of Medicine. 1995; 332: 345-350. Mechanical Ventilation Mechanical Ventilation Tidal breath controlled entirely by the ventilator Or Interactive with patient effort. MODES OF VENTILATION • Classified by the Amount of Work Assumed by the Ventilator • Control or Assist Control • Classified by the Target Used to End Inspiratory Phase of Each Delivered Breath • Volume or flow target :set flow and volume as cycling variable so pressure is dependent • Pressure target :set time or flow as cycling variable so volume or flow dependent VOLUME TARGETED VENTILATION • Set Tidal Volume (TV) • Inspiratory Cycle Ends When TV Delivered • Ventilator Generates Sufficient Pressure to deliver set volume • Independent of Airway Resistance • Independent of Lung Compliance • High-Pressure Limit Alarm • Alveolar Stretch Injury WK505 Effort Volume -Controlled Ventilation Nilsestuen, Respir Care 2005; 50:202-232 PRESSURE TARGETED VENTILATION • Constant Inspiratory Pressure • Tidal Volume Becomes Variable • Affected by Airway Resistance, Lung Compliance, Patient Effort • Causes of Decreased Tidal Volume • Increased Resistance • Decreased Compliance • Decreased Patient Effort • Low minute ventilation alarm Why does the Volume variable with similar pressure? )Transpulmonary Pressure(PTp ( PTp=(PA-PpL گرادیان فشاری بین فشارداخل وخارج ریوی که مسئول باز نگه داشتن راه هوایی میباشد. )Transairway Pressure(PTA PTA=Paw-Palv مسئول حرکت گاز ازخالل راه هوایی می باشد.جزء مقاومت راه هوایی )Transthorasic Pressure(PTT PTT=Palv-Pbs گرادیان فشاری بین فشارالوئولی وفشار سطح بدن فشار الزم برای اتساع وجمع شدن همزمان ریه ها وقفسه سینه یا جزء االستیک )PRESSURE(spont Breathing انتهای دم داخل الوئول داخل پلور 0 cmH2o -10 cmH2o فشار ترانس پولمونار PL=0-(-10 )=10cmH2o انتهای باز دم 0 cmH2o -5 cmH2o PL=0-(-5)=5cmH2o Pressures around the balloon Palv = Ptp + Ppl Palv = 0, the same as the room if no air is flowing into the lung. Ppl is subatmspheric due to the recoil of the lung away from the jar. PPlat = PAlv PPlat = Transpulmonary Pressure + Ppl transpulmonary pressure = 15 cm H2O Ppl =+15 cm H2O Pplat 30 cm H2O Stiff chest wall PPlat = PAlv; PPlat = Transpulmonary Pressure + Ppl -15 cm H2O transpulmonary pressure = 45 cm H2O Pplat 30 cm H2O Active inspiratory effort PPlat Pplat 30 cm H2O, VCV PPlat = PAlv; = Transpulmonary Pressure? Pplat 30 cm H2O, VCV Pplat 30 cm H2O, PCV Active inspiratory effort Volume variable with similar pressure Risk of VILI“ : Transpulmonary Pressure or Pplat Risk of VILI may be different with the same PPlat Ventilator mode Mechanical Ventilation Mode classify by these three variable : Trigger (initiate breath): patient or set machine timer Limit, Factors are operator-specified values (control gas delivery during the breath): flow or inspiratory pressure Cycle (terminates the inspiration) : flow or inspiratory time or volume Pressure is often a backup safety cycle variable Trigger or sensitivity : trigger variableدر واقع عامل شروع كننده و به عبارتي محرك انجام عمل دم توسط ونتیالتور است تغییر مي تواند تغییر فشاري و یا فلو باشد و در پاسخ به آن ، دم آغاز میشود پس یك triggerمي تواند به دو فرم باشد * Flow trigger *pressure trigger ) *NAVA (Neurally Adjusted Ventilatory Assist Trigger or sensitivity pressure triggerرا معموال" روي -./5تا - 2 سانتي متر آب Flow triggerرا معموال" روي 1تا 2لیتردردقیقه : lag time زمان تاخیر از زمان حس كردن و نتیالتور تا شروع دم را lag timeمیگویند اهمیت این زمان در اعمال كار اضافي به سیستم تنفس است . :Trigger عملكرد اصلي آن هماهنگي بین بیمار و دستگاه است محدوده آن بین -./5تا -10سانتي متر آب آنرا بطور معمول -2سانتي متر آب كمتر از فشار انتهاي بازدمي تنظیم مي كنیم یعني اگر peepرا 5گذاشتیم triggerرا -3مي گذاریم تا وقتي فشار در این مدار به این حد رسید Triggerنماید. در مدهایي نظیر SIMVنباید triggerرا بیش از -1تا -2سانتي متر آب گذاشت و حساسیت را باال برد زیرا این افزایش حساسیت سبب افزایش كوشش دمي و خستگي عضالت و افزایش كار عضالني میشود . Trigger The inspiratory effort necessary to trigger a breath has been estimated to be about 17% and about 12% of the total inspiratory effort during pressure and flow triggering, respectively Limit :Limitمتغیري است كه اجازه تخطي در جریان دم را نمي دهد و اغلب همان control varibleاست و سبب ختم دم مي شود ( ولي نه همیشه ) Cycle متغییري است كه سبب ختم دم مي شود كه مي تواند فشار ،حجم ،زمان و یا ( Flowجریان دمي ) باشد . Patient ventilator interaction Initiation of inspiration :Trigger Inspiration :limitation Inspiration to expiration :cycling Expiration Expiration to inspiration :Trigger BEST PEEP عبارت است از ميزان پيپ اعمال شده اي كه سبب بهترين اكسيژناسيون شود ،FRCپذيرش ريه و اكسيژناسيون را افزايش داده و سبب كاهش شانت شود.وهمچنين حداقل اثر برروی هموديناميک. Auto-PEEP or Intrinsic PEEP What is Auto-PEEP? Normally, at end expiration, the lung volume is equal to the FRC When PEEPi occurs, the lung volume at end expiration is greater then the FRC Auto-PEEP or Intrinsic PEEP Why does hyperinflation occur? Airflow limitation because of dynamic collapse or lesions that increase expiratory resistance No time to expire all the lung volume (high RR or Vt) Expiratory muscle activity Auto-PEEP or Intrinsic PEEP Auto-PEEP is measured in a relaxed pt with an end-expiratory hold maneuver Exiratory flow pattern flow Flow Waveform inhalation time 0 auto-PEEP exhalation No active exhalation or inspiratory effort Treats lungs as single compartment PIP pressure PIP auto PEEP set PEEP time Auto-PEEP or Intrinsic PEEP Adverse effects: Predisposes to barotrauma Predisposes hemodynamic compromises Diminishes the efficiency of the force generated by respiratory muscles Augments the work of breathing Augments the effort to trigger the ventilator sensitivity -1 cm H2O auto-PEEP 10 cm H2O trigger effort = 11 cm H2O sensitivity -1 cm H2O auto-PEEP 3 cm H2O trigger effort = 4 cm H2O Auto-PEEP should be measured with set PEEP = 0 (Inspiratory plateau(Pause پالتوي دمي ( )Inspiratory platoبا مسدود كردن دریچه بازدمي در پایان دم ,فشار دمي در حد ثابتي باقي مانده و حفظ مي شود چون این فشار ثابت است به آن فشار مسطح دمي مي گویند . بااعمال این فشار جریان هوا بیشتر به قسمت هاي محیطي انتشار یافته و بنابراین VDیا حجم فضاي مرده كاهش مي یابد بدین وسیله مي توان به وجود نشت در سیستم تنفسي پي برده و كمپلیانس ریه و مقاومت آنرا مانیتوركرد . )Flowیا )Flow Peak اگر حجم جاري یك بیماري 1000سی سی تنظیم شده وزمان دم یك ثانیه باشد فلوي دمي 60لیتردر دقیقه مي شود اكثر ونتیالتورها مي توانند فلوي بیش از 120تا 180لیتر در دقیقه بدهند هر چه میزان Flow Peakبیشتر ،زمان دم كوتاه تر و زمان بازدم طوالني ترو I/E Ratioكمتر مي شود وبنابراین دربیماران COPDمناسب است. باید دانست كه این سرعت باال ایجاد جریان گردابي یا توربوالنت مي كند. سوال Flowبه چه صورت به بيمار تحويل ميشود؟ -1مربعي يا Square در این حالت سرعت جریان دمي بالفاصله به حداكثر رسیده ودر تمامي مدت زمان دم حفظ مي شود و ناگهان قطع مي شود. این روش بیشتر در بیماران بیهوش بكار مي رود زیرا عضالت تنفسي فلج بوده و ریه ها سالم هستند -2سينوسي يا سينوزوئيدال :Sinusoidal در این حال جریان دمي بتدریج به حداكثر رسیده و بتدریج هم كاهش مي یابد كه در تنفس Spontبیشتر دیده مي شود. -3صعودي Acceleratingيا Ascending :Ramp در اين حال جريان دمي بتدزيج به حداكثر خود ميرسد و ناگهان قطع مي شود. -4نزولي Desending rampيا Decelerating در این حال جریان دمي به سرعت به پیك رسیده وسپس بتدریج كاهش مي یابد. در بیماران مبتال به ARDSكاربرد دارد. Flow pattern Fio2 بر اساس Pao2در ABGاست. Pao2باید به گونه اي انتخاب شود كه اشباع هموگلوبین )(Spo2 بیش از %90باشد تا Pao2هم باالتر از 60میلي جیوه شود. اگر در درصد اكسیژن دمي Fio2بیش از 60درصد تنظیم شده و pao2ما همچنان كمتر از 60میلي متر جیوه بود .اولین اقدام : افزایش peepاست و نه درصد اكسیژن دمي در بیمارن مبتال به COPDباید Pao2بین 50تا 55درصد حفظ شود در این بیماران ابتدا Fio2را حدود 30درصد تنظیم میكنیم Fio2بدنبال CPRو پیپ باال در شروع %100باید باشد. Fio2=100 for 12hr Fio2=100 for 24hr Fio2=60 for 36hr :Sigh - sighبه معناي دم عمیق است در حالت نرمال انسان بطور متوسط هر 5تا 10دقیقه یك دم عمیق انجام میدهد . هدف از sighدر انسان جلوگیري از انسداد راههاي هوایي كوچك و بازكردن آلوئولها است. در برخي از ونتیالتورها هم براي مشابه سازي این حالت تنظیم و تعداد sighتعبیه شده است . هر sighبطور متوسط 2.5برابر حجم جاري بوده و بطور متوسط 10بار در ساعت اتفاق مي افتد I:E RATIO Defined: Inspiratory time: expiratory time Normal physiologic I:E Ratio is close to 1:2. (take a regular breath, then exhale…notice it takes longer to passively exhale that same breath than to inhale.) I:E Ratio This ratio is usually changed as follows: With obstructive type disease→ I:E from 1:2 up to 1:2.5 or 1:3. This creates more time for those patients to exhale what is being obstructed by their disease process. Modes of Ventilation Spontaneous Modes Three basic means of providing support for continuous spontaneous breathing during mechanical ventilation Spontaneous breathing CPAP PSV – Pressure Support Ventilation Modes of Ventilation Spontaneous Modes Spontaneous breathing Patients can breathe spontaneously through a ventilator circuit; sometimes called T-Piece Method because it mimics having the patient ET tube connected to a Briggs adapter (T-piece) Advantage Ventilator can monitor the patient’s breathing and activate an alarm if something undesirable occurs Disadvantage May increase patient’s WOB with older ventilators CPAP This is not a true support-mode of ventilation, Each inspiration and charges the circuit to a constant, operator-specified pressure that can range from 0 to 20 cmH2O CPAP is used to assess extubation potential in patients who have been effectively weaned in patients with intact respiratory system function who require an endotracheal tube for airway protection CPAP Independent Variables(Set by User) FIO2 Level of CPAP Dependent Variables(Monitored by User) Tidal volume Rate, flow pattern Airway pressure PaO2, PaCO2, I/E ratio Trigger/Cycle Limit No trigger Pressure limit Advantages Allows assessment of spontaneous function Helps prevent atelectasis Disadvantages No backup Initial Settings FIO2 = 0.5–1.0 CPAP = 5–15 cmH2O CMV – Continuous Manditory Ventilation The Original Mechanical Vent Has since been replaced in most locations in the hospital by fancier settings Still used in the Operating Room CMV Three Variables 1) Respiratory Rate 2) Tidal Volume 3) FIO2 CMV CMV The Tidal Volume with the set FIO2 gets blown into the patient at the set respiratory rate. CMV CMV – RR / Vt / FIO2 CMV 12 / 600 / 30% Minute Ventilation = Respiratory Rate * Tidal Volume 12 / min * 600 cc = 7.2 L/min PAo2 = FIO2 (760 – 47)-Paco2/0.8 30% * 713 = 213.9 mmHg O2 CMV Advantages Easy to set up: need a bellows, a motor, and a timer. Easy to adjust the settings Main Disadvantage If the Patient is breathing spontaneously, the patient will be fighting the ventilator. PCV Time triggered, time cycled, and pressure limited During the inspiratory phase, a given pressure is imposed at the airway opening, and the pressure remains at this user-specified level throughout inspiration tidal volume and inspiratory flow rate are dependent rather than independent variables PCV is the preferred for barotrauma and for postoperative thoracic When PCV is used, minute ventilation and tidal volume must be monitored; PCV Independent Variables(Set by User) FIO2 Inspiratory pressure level Ventilator rate Level of PEEP Pressure limit I/E ratio Dependent Variables(Monitored by User) Tidal volume Flow rate, pattern Minute ventilation PaO2, PaCO2 Trigger/Cycle Limit Timer/patient Timer/pressure limit Advantages System pressures regulated Useful for barotrauma treatment Timer backup Disadvantages Requires heavy sedation Not useful for weaning Initial Settings FIO2 = 1.0 PC = 20–40 cmH2O PEEP = 5–10 cmH2O f = 12–15/min I/E = 0.7/1–4/1 Assist Control Mode Ventilation (ACMV) The patient is spontaneously breathing so we are assisting his VENTILATION. ACMV In inspiratory cycle is initiated either by the patient's inspiratory effort or, if no patient effort is detected within a specified time window, by a timer signal within the ventilator. Every breath delivered, whether patient or timer triggered, consists of the operator-specified tidal volume. Ventilatory rate is determined either by the patient or by the operator-specified backup rate, whichever is of higher frequency( ACMV ACMV is commonly used for initiation of mechanical ventilation because it ensures a backup minute ventilation Allows for synchronization of the ventilator cycle with the patient's inspiratory effort Problems of ACMV When is used in patients with tachypnea due to nonrespiratory or nonmetabolic factors such as anxiety, pain, or airway irritation. Respiratory alkalemia may develop and trigger myoclonus or seizures. Dynamic hyperinflation (so-called auto-PEEP) may occur if the patient's respiratory mechanics are such that inadequate time is available for complete exhalation between inspiratory cycles. ACMV is not effective for weaning patients from mechanical ventilation because it provides full ventilator assistance on each patient-initiated breath ACMV ACMV Independent Variables(Set by User) FIO2 Tidal volume Ventilator rate Level of PEEP Inspiratory flow pattern Peak inspiratory flow Pressure limit Dependent Variables(Monitored by User) Peak airway pressure, PaO2, PaCO2 Mean airway pressure I/E ratio Trigger/Cycle Limit Patient/timer Pressure limit Advantages Timer backup Patient-vent synchrony Patient controls minute ventilation Disadvantages Not useful for weaning Potential for dangerous respiratory alkalosis Initial Settings FIO2 = 1.0 Vt = 10–15 mL/kg f = 12–15/min PEEP = 0–5 cmH2O Inspiratory flow = 60 L/min Modes of Ventilation Intermittent Mandatory Ventilation – IMV Periodic volume or pressure targeted breaths occur at set interval (time triggering) Between mandatory breaths, the patient breathes spontaneously at any desired baseline pressure without receiving a mandatory breath Patient can breathe either from a continuous flow or gas or from a demand valve Modes of Ventilation Intermittent Mandatory Ventilation – IMV Indications Facilitate transition from full ventilatory support to partial support Advantages Maintains respiratory muscle strength by avoiding muscle atrophy Decreases mean airway pressure Facilitates ventilator discontinuation – “weaning” Modes of Ventilation IMV-Intermittent Mandatory Ventilation Complications When used for weaning, may be done too quickly and cause muscle fatigue Mechanical rate and spontaneous rate may asynchronous causing “stacking” May cause barotrauma or volutrauma SIMV The major difference between SIMV and ACMV is that in the former the patient is allowed to breathe spontaneously, i.e., without ventilator assist, between delivered ventilator breaths. However, mandatory breaths are delivered in synchrony with the patient's inspiratory efforts at a frequency determined by the operator. If the patient fails to initiate a breath, the ventilator delivers a fixed-tidal-volume breath and resets the internal timer for the next inspiratory cycle SIMV SIMV allows patients with an intact respiratory drive to exercise inspiratory muscles between assisted breaths, making it useful for both supporting and weaning intubated patients. SIMV SIMV may be difficult to use in patients with tachypnea because they may attempt to exhale during the ventilator-programmed inspiratory cycle. When this occurs, the airway pressure may exceed the inspiratory pressure limit, the ventilator-assisted breath will be aborted, and minute volume may drop below that programmed by the operator. In this setting, if the tachypnea is in response to respiratory or metabolic acidosis, a change to ACMV will increase minute ventilation and help normalize the pH while the underlying process is further evaluated SIMV SIMV Independent Variables(Set by User) FIO2 Tidal volume Ventilator rate Level of PEEP Inspiratory flow pattern Peak inspiratory flow Pressure limit Same as for ACMV Dependent Variables(Monitored by User) Peak airway pressure, PaO2, PaCO2 Mean airway pressure I/E ratio Same as for ACMV Trigger/Cycle Limit Patient/timer Pressure limit Same as for ACMV Advantages Timer backup useful for weaning Disadvantages Potential dysynchrony Initial Settings FIO2 = 1.0 Vt = 10–15 mL/kg f = 12–15/min PEEP = 0–5 cmH2O Inspiratory flow = 60 L/min Same as for ACMV Modes of Ventilation Pressure Support Ventilation – PSV Patient triggered, pressure targeted, flow cycled mode of ventilation Requires a patient with a consistent spontaneous respiratory pattern The ventilator provides a constant pressure during inspiration once it senses that the patient has made an inspiratory effort Modes of Ventilation PSV Modes of Ventilation PSV Indications Spontaneously breathing patients who require additional ventilatory support to help overcome WOB, CL, Raw Respiratory muscle weakness Weaning (either by itself or in combination with SIMV) Modes of Ventilation PSV Advantages Full to partial ventilatory support Augments the patients spontaneous VT Decreases the patient’s spontaneous respiratory rate Decreases patient WOB by overcoming the resistance of the artificial airway, vent circuit and demand valves Allows patient control of TI, I, f and VT Modes of Ventilation PSV Advantages Set peak pressure Prevents respiratory muscle atrophy Facilitates weaning Improves patient comfort and reduces need for sedation May be applied in any mode that allows spontaneous breathing, VC-SIMV, PC-SIMV Modes of Ventilation PSV Disadvantages Requires consistent spontaneous ventilation Patients in stand-alone mode should have back-up ventilation VT variable and dependant on lung characteristics and synchrony Low exhaled Fatigue and tachypnea if PS level is set too low Modes of Ventilation Flow Cycling During PSV Flow cycling occurs when the ventilator detects a decreasing flow, which represents the end of inspiration This point is a percentage of peak flow measured during inspiration PB 7200 – 5 L/min Bear 1000 – 25% of peak flow Servo 300 – 5% of peak flow No single flow-cycle percent is right for all patients Modes of Ventilation PSV during SIMV Spontaneous breaths during SIMV can be supported with PSV (reduces the WOB) PCV – SIMV with PSV Modes of Ventilation PSV during SIMV Spontaneous breaths during SIMV can be supported with PSV VC – SIMV with PSV Modes of Ventilation PSV NOTE: During pressure support ventilation (PSV), inspiration ends if the inspiratory time (TI) exceeds a certain value. This most often occurs with a leak in the circuit. For example, a deflated cuff causes a large leak. The flow through the circuit might never drop to the flow cycle criterion required by the ventilator. Therefore, inspiratory flow, if not stopped would continue indefinitely. For this reason, all ventilators that provide pressure support also have a maximum inspiratory time. Modes of Ventilation PSV Setting the Level of Pressure Support Goal: To provide ventilatory support Spontaneous tidal volume is 10 – 12 mL/Kg of ideal body weight Maintain spontaneous respiratory rate <25/min Goal: To overcome system resistance (ET Tube, circuit, etc.) in the spontaneous or IMV/SIMV mode Set pressure at (PIP – Pplateau) achieved in a volume breath or at 5 – 10 cm H2O Modes of Ventilation PSV Exercise: Using the PIP and the PPlateau from the pressure waveform below, recommend a pressure support setting for this patient (patient is in VC-SIMV mode) 35 25 Answer: 10 cm H2O Modes of Ventilation PSV - The results of your work 35 cm H2O 10 cm H2O Independent Variables(Set by User) FIO2 Inspiratory pressure level PEEP Pressure limit Dependent Variables(Monitored by User) Tidal volume Flow rate, pattern Minute ventilation PaO2, PaCO2 I/E ratio Trigger/Cycle Limit Inspiratory flow Pressure limit Advantages Assures synchrony Good for weaning Disadvantages No timer backup Initial Settings FIO2 = 0.5–1.0 PS = 10–30 cmH2O 5 cmH2O usually the level used PEEP = 3–5 cmH2O Spontaneous Modes VS (Volume support) Modes of Ventilation Spontaneous Modes Bilevel Positive Airway Pressure (BiPAP) Commonly patient triggered but can be time triggered, pressure targeted, flow or time cycled The operator sets two pressure levels IPAP (Inspiratory Positive Airway Pressure) IPAP is always set higher than EPAP Augments VT and improves ventilation EPAP (Expiratory Positive Airway Pressure) Prevents early airway closure and alveolar collapse at the end of expiration by increasing (and normalizing) the functional residual capacity (FRC) of the lungs Facilitates better oxygenation Modes of Ventilation Spontaneous Modes Bilevel Positive Airway Pressure (BiPAP) The operator sets two pressure levels -IPAP -EPAP NOTE: The pressure difference between IPAP and EPAP is pressure support Modes of Ventilation (Mandatory Minute Ventilation) MMV also called minimum minute ventilation Provides a predetermined minute ventilation when the patient’s spontaneous breathing effort becomes inadequate Useful for preventing hypoventilation and respiratory acidosis in the final stages of weaning with SIMV Need to keep watch spontaneous minute volume (distressed pt. may increase RR with lower tidal volume) SVCC Respiratory Care Programs ASV (adaptive support ventilation) Clinician enters pt. data & % support Vent. calculates needed min. vol. & best rate/TV to produces least work. Targeted TV’s given as press. control or press. support breaths Breath is: PC if time triggered, PS if pt. triggered ASV (adapt. sup. vent.) Vent. measures & analyzes data & mechanics each breath for: compliance resistance inspiratory & expiratory time constants actual Ins-time, Exp-time, total F& min. vol. pressures Press. adjusts in +/- 2 cm H2O to achieve TV ASV: Principle mode of ventilation Flow E + + Flow I * * no patient activity: * machine triggered patient is active: * patient triggered + flow cycled Pinsp PEEP + time cycled From Hamilton Medical ASV - Considerations Mandatory breaths = PC, pt. triggered = PS both at same targeted TV and calculated press. vent., mode is PC-SIMV/PS If pt.’s f > “set” by vent., mode is PS If pt.’s f < “set” by is apneic, all breaths are PC Exp minute ventilation(100%-350%)support VAPS: Volume Assured Pressure Support Combines volume ventilation & pressure support (for mech., vol. limited breaths only) Uses TV, peak flow, and pressure sup./control settings Targets PS level with at least set peak flow first Continues until flow decreases to set peak flow, then: If TV not delivered, peak flow maintained until vol. limit If TV or more delivered, breath ends VAPS: (and Pressure Augmentation) Considerations The set TV is the minimum TV the patient will receive The set pressure support is the minimum the patient will receive The set peak flow is the minimum the patient will receive No ventilatory mechanics measured VAPS: Volume Assured Pressure Support Pressure Regulated Volume Control Combines volume ventilation & pressure control (for mech., time-cycl. breaths only) Set TV is “targeted” Ventilator estimates vol./press. relationship each breath Ventilator adjusts level of pressure control breath by breath Pressure Regulated Volume Control First breath = 5-10 cm H2O above PEEP V/P relationship measured Next 3 breaths, pressure increased to 75% needed for set TV Then up to +/- 3 cm H2O changes per breath Time ends inspiration Pressure Regulated Volume Control BiLevel Ventilation: APRV Uses 2 pressure levels for 2 time periods Plow & Phigh, Thigh and Tlow Patient triggering & cycling can change phases PHIGH P PEEPLOW TLOW THIGH Synchronized Transitions T From PB product lit. Synchronized Transitions BiLevel Ventilation: APRV Uses two levels of pressure for two time periods Mandatory breaths at the higher pressure are time cycled Spontaneous breaths can be pressure supported Spontaneous Breaths P Spontaneous Breaths T From PB product lit. BiLevel Ventilation: APRV Pressure support may be applied at both pressures during a spont. breath If PS is set higher than PH, the PS pressure is applied to a spontaneous effort at upper pressure PHi PHi + PS Pressure Support P PEEPL From PB product lit. APRV Airway Pressure Release Ventilation Like BiPAP/BiLevel but time at the lower pressure (“release time”) is usually short, 1-1.5 seconds Spontaneous breathing still allowed throughout low & high pressures APRV Airway Pressure Release Ventilation From Mosby’s R. C. Equip. 6th ed. 1999. APRV(Airway pressure release ventilation) APRV(Airway pressure release ventilation) Proportional Assisted Ventilation(PAV) Pmus=Pres +pel Pmus=(flow /resistance)+(volume/elastance) Pmus+Pappl=(flow/resistance)+(volume/elastance) Proportional Assisted Ventilation PSV Main setting parameter is percent of assist Proportional Assist Ventilation Allows free flow based on patient effort “Targets” portion of patient’s work during “spontaneous” breaths Automatically adjusts flow, volume and pressure needed each breath PAV continued “Vol. assist %” reduces work of elastance “Flow assist%” reduces work of resistance's Pressure adjusts during each breath to control work level Increased patient effort causes increased applied pressure (and flow & volume) PAV continued Other controls useful for PAV High pressure limit High volume limit Back-up ventilation mode Typical alarms etc. PAV - Considerations Consistent level of support per breath Patient controls breathing pattern Patient triggered mode (Unless back-up mode present) Reduced support with Auto-PEEP Cannot compensate for leaks (prototypes) PAV continued From Younes, M: Ch.15, in Tobin, MJ Prin. & Pract. Of Mech. Vent. 1994 McGaw-Hill, Inc. IRV PCV with the use of a prolonged inspiratory time Applied to patients with severe hypoxemic respiratory failure It is thought to work in conjunction with PEEP to open collapsed alveoli and improve oxygenation there are no convincing data to show that IRV improves outcomes. Open lung ventilation (OLV) Any of these specific modes with TV to achieve 5–6 mL/kg, and PEEP achieve maximal alveolar recruitment PEEP > CCP (Critical closing pressure) PC (above peep) <COP (Critical opening pressure) Open lung ventilation (OLV) primary objectives of ventilator support are maintenance of adequate oxygenation and avoidance of cyclic opening and closing of alveolar units by selecting a level of PEEP that allows the majority of units to remain inflated during tidal ventilation. Achievement of eucapnia and normal blood pH through adjustments in ventilator tidal volume and breathing frequency are of lower priority. 1.6 volume above FRC (liters) 1.2 0.8 0.4 normal ARDS upper inflection point 0 lower inflection point 0 10 20 30 airway pressure (cm H2O) 40 Respiratory asidosis+alkalosis Vt(fav) = Paco2(pat) . Vt(pat) / Paco2(fav) Vt=10-12cc/kg F(fav) =Paco2(pat) . F(pat) / paco2(fav) RR=12-16 Different types of patient COPD and Asthma Goals: Diminish dynamic hyperinflation Diminish work of breathing Controlled hypoventilation (permissive hypercapnia) Diminish DHI Why? Diminish DHI How? Diminish minute ventilation Low Vt (6-8 cc/kg) Low RR (8-10 b/min) Maximize expiratory time Diminish work of breathing How: Add PEEP (about 85% of PEEPi) Applicable in COPD and Asthma. Controlled hypercapnia Why? Limit high airway pressures and thus diminish the risk of complications Controlled hypercapnia How? Control the ventilation to keep adequate pressures up to a PH > 7.20 and/or a PaCO2 of 80 mmHg Controlled hypercapnia Contrindication: Head pathologies Severe HTN Severe metabolic acidosis Hypovolemia Severe refractory hypoxia Severe pulmonary HTN Coronary disease ARDS Ventilation with lower tidal volume as compared with traditional volumes for acute lung injury and the ARDS The Acute Respiratory Distress Syndrome Network N Engl J Med 2000;342:1301-08 Methods March 96 – March 99 10 university centers Inclusion: Diminish PaO2 Bilateral infiltrate Wedge < 18 Exclusion Randomized Methods A/C 28d or weaning 2 groups: 1. Traditional Vt (12cc/kg) 2. Low Vt (6cc/kg) End point: 1. Death 2. Days of spontaneous breathing 3. Days without organ failure or barotrauma Results The trails were stopped after 861 pt because of lower mortality in low Vt group Conclusion Type of patient Tidal Volume RR PEEP FIO2 Ins. Flow I:E Normal 10 cc/kg 10 to 12 0 to 5 100%. 60 l/min 1:2. ARDS 6 cc/kg 10 to 12 5 to 15 100%. 60 l/min 1:2. COPD 6 cc/kg 10 to 12 5 100%. Trauma 10 cc/kg 10 to 12 100%. 60 l/min 1:2. Pediatric 8-10 cc/kg Varies age 3 to 5 100%. 60 l/min 1:2. 100 to 120 1:3 to 1:4 Note Note PH>7.2 PCO2 <80 mmhg Trigger to consider Trigger to consider The Wean Step 1 1. Lung injury is stable or resolving 2. Gas exchange is adequate with low PEEP and FIo2 3. Hemodynamics are stable without a need for vasopressors 4. Patient can initiate spontaneous breaths If meeting all four criteria The Wean Step 2 Perform spontaneous breathing trial (SBT) using a T-piece ,CPAP , or 5 cm H2O PS for 30-120 minutes Assessments include: Gas exchange Ventilatory pattern Hemodynamics comfort The Wean Patients passing this trial should immediate ventilator removal Patients failing this trial should return to ventilator for the next 24 hours and then be reassessed The Wean Gradual reduction may be worse than every 24 hour SBT approach RESPIRATORY RATE • Number of Breaths Per Minute (BPM) • Trigger: Factor that begins inspiratory phase • Controlled Breaths • Triggered by Ventilator • Determined by Set Rate • Ten BPM Setting: Breath is Triggered Every 6 Seconds • Assisted Breaths: Triggered by Patient Effort • Ventilator Sensitivity Adjusted • Avoid Insignificant Patient Effort Triggering a Delivered Breath 1.6 volume above FRC (liters) 1.2 0.8 0.4 normal ARDS upper inflection point 0 lower inflection point 0 10 20 30 airway pressure (cm H2O) 40 Monitoring of the patient HYPOXIA: DIFFERENTIAL DIAGNOSIS • Hypoventilation • V/Q Mismatch: • Bronchospasm • Increased Secretions • Alveolar Edema (Hyaline Membranes on Histology • Right to Left Cardiac Shunt • Blood flows past non-ventilated alveoli • Not amenable to increasing inspired oxygen fraction • Atelectasis • Lung Consolidation • Pulmonary Edema SYSTEMATIC RESPONSE TO HYPOXIA • Arterial Blood Gas • Portable CXR • With No Other Proximate Cause, Adjust Ventilator Settings • Maintain 100% FiO2 • Increase Mean Airway Pressure • Increase Inspiratory Time • Chemically paralyze patient Oxygenation What is the number one cause of decreased oxygenation? V-Q Mismatch Oxygenation What is the number one cause of V-Q Mismatch? Atelectasis Oxygenation How do we fix V-Q mismatch caused by atelectasis? Recruit the unused alveoli increase “V” to Oxygenation How do we recruit alveoli? PEEP Positive end expiratory pressure Decreases the expiratory gradient Causes air trapping Trapped air tries to distribute evenly and leads to opening of all airways. Oxygenation What about decreasing the expiratory time relative to the inspiratory time? This leads to air trapping. Since it behaves like peep, we call it: AUTO-PEEP Oxygenation All patients on a ventilator have some amount of atelectasis When a patient is oxygenating poorly, we can try to improve VQ matching by fixing that atelectasis with PEEP or AUTO-PEEP Oxygenation CMV 12 / 700 / 30% / +5 A-C 12 / 700 / 30% / +5 A-C 12 / 700 / 30% / I:E 2:1 SIMV 12 / 700 / 30% / PS12 / +5 PS 12 / +5 Oxygenation Disadvantages to PEEP PEEP increases mean intrathoracic pressure and can seriously drop the Cardiac Output PEEP can hyperinflate alveoli and cause VOLUTRAUMA Disadvantages to autoPEEP Doesn’t work well with rapid RR Doesn’t work well in COPDers Driving Oxygenation Increase and Decrease FIO2 as needed. When FIO2 gets over 50%, start thinking about PEEP / auto-PEEP When FIO2 requirements are falling, think about losing PEEP INCREASE PO2 • Increase Fio2 • Increase Mean Airway Pressure (Paw) • Paw: Average Pressure Created Within the Lung Over One Minute • Paw Increased By • Increases in PEEP • Increases Inspiratory time SYSTEMATIC RESPONSE TO HYPOXIA • • • • • • • Turn FiO2 to 100% Take Patient OFF Ventilator Bag the Patient on FiO2 100% Rapid Assessment ABC From “Patient to Wall” Endotracheal Tube: Position, Patency Auscultate: Rule Out Tension Pneumothorax Ventilator: Circuit, Functional State, Oxygen CHANGE PCO2 Alter Minute Ventilation • Respiratory rate • Tidal volume Permissive Hypercapnia • Used In Non-Compliant Lungs (ARDS) • Non-Heterogeneous Process • Avoidance of Barotrauma and Volutrauma to Unaffected Regions • Maintain pH > 7.25 • Proper Physiologic Milieu • HCO3 if necessary Different types of patient COPD and Asthma Goals: Diminish dynamic hyperinflation Diminish work of breathing Controlled hypoventilation (permissive hypercapnia) Diminish DHI Why? Diminish DHI How? Diminish minute ventilation Low Vt (6-8 cc/kg) Low RR (8-10 b/min) Maximize expiratory time Diminish work of breathing How: Add PEEP (about 85% of PEEPi) Applicable in COPD and Asthma. Controlled hypercapnia Why? Limit high airway pressures and thus diminish the risk of complications Controlled hypercapnia How? Control the ventilation to keep adequate pressures up to a PH > 7.20 and/or a PaCO2 of 80 mmHg Controlled hypercapnia Contrindication: Head pathologies Severe HTN Severe metabolic acidosis Hypovolemia Severe refractory hypoxia Severe pulmonary HTN Coronary disease Trouble Shooting Trouble Shooting Doctor, doctor, his pressures are going up!!! What is your next step? Trouble Shooting Ask which pressure is going up Trouble Shooting Ppeak is up Look at your Pplat Trouble Shooting If your Pplat is high, you are faced with a COMPLIANCE problem If your Pplat is N, you are faced with a RESISTIVE problem DD? Trouble Shooting Trouble Shooting Doctor, doctor, my patient is very agitated! What is your next step? Trouble Shooting Look at your pt! Trouble Shooting At the time of intubation, fighting is largely due to anxiety But what do you do if pt is stable and then becomes agitated? Trouble Shooting 1. 2. 3. 4. 5. 6. Remove pt from ventilator Initiate manual ventilation Perform P/E and assess monitoring indices Check patency of airway If death is imminent, consider and treat most likely causes Once pt is stabilized, undertake more detailed assessement and management Trouble Shooting THE END