Ventilator Basics
advertisement

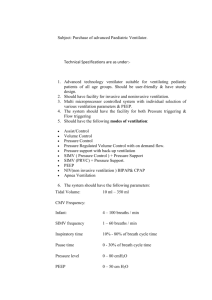
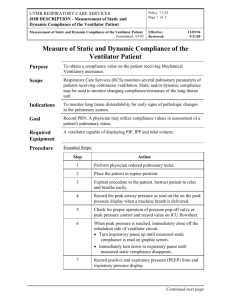
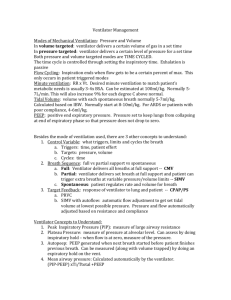
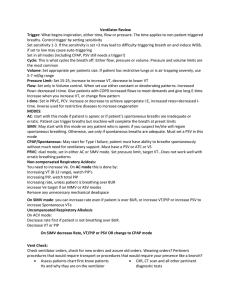
Ventilator Basics. By Fen Moy There are MANY blogs/books/web posts written on ventilators – which will fully educate you! But this is my basic outline of a ventilator & how it works! Human Lungs -> work by creating a negative pressure to allow air flow in. Ie: taking a breath in expands the chest wall, which creates intra-thoracic negative pressure, & air flows from +ve to –ve pressures into the alveoli along the various air conduits. Mechanical Ventilators -> work by positive pressure – blowing a set amount of air into the lungs. This amount can be determined by volume or by the pressure generated. Basic Variables to control on the ventilator Type of ventilation Rate FiO2 Volume or pressure Peak inspiratory pressure PEEP Type of Ventilation: In ED – SIMV is the way to go. Stands for Synchronised Intermittent Mandatory Ventilation. What it means is that the ventilator will give the set number of breaths as programmed, but if the patient initiates a breath which generates enough pressure, the ventilator will allow that breath to be taken. In a paralysed pt – ie our ED pts, the pt will not be taking any spontaneous breaths, and generally if they are – then you’ll either give more paralytics, or you are looking at extubating for end of life cares. (Note: we do NOT extubate pts in ED unless it is for palliative cares.) Rate: Generally 12-16/min is a good start. Adjust according to ABG. ETCO2 tends to underestimate PaCO2. Aim is to maintain normocarbia (35-45mmHg), unless in specific special circumstances of metabolic acidosis in salicylate poisoning (then keeping CO2 low) or in asthma (higher CO2 is accepted to prevent barotrauma) (you should be getting help with these special settings if they ever occur!) CO2 will take a while to normalise if pt has had altered respiratory effort, so as long as serial CO2s are trending down, it’s ok. Don’t try to achieve normality too quickly as you may cause more barotrauma/CVS instability by being too aggressive. FiO2: Start with 100%! Volume or Pressure: Volume control is generally used in ED. It delivers a set amount of volume and we know how much the patient is getting. Only danger is that if the airways have high resistance, then giving a set volume which is TOO HIGH can cause barotrauma, as the ventilator will push the volume through almost regardless of pressure, until the peak inspiratory pressure is reached. Although you won’t get above a set maximum pressure, there are some alveoli which would have received barotrauma at lower pressures because not all alveoli are subject to the same forces or have the same ability to stretch. The volume is also given at a set rate, which generates a sharp increase in pressure that also contributes to barotrauma. Pressure control is more elegant in that you can set the airway pressure and the machine works it so that the rise of airway pressure is not rapid and allows for gentler alveoli expansion. But volumes thus delivered can be variable, and needs a more sophisticated ventilator to be able to deliver this ( ie: not our transport ventilators!) What is a safe volume? Guestimates of 10mL/kg as a tidal volume is a good rule. If pt has high resistance airways & a worry of barotrauma is present, then going down to 6mL/kg is ok. So somewhere between 610ml/kg. Generally speaking 500-700mL is what is dialled on the machine. Peak Inspiratory Pressure (PIP): 40cmH2O (some texts will quote 35cmH2O) is generally what’s set. Just so your lungs don’t pop! PEEP: Positive End Expiratory Pressure. Useful in preventing total collapse of alveoli during expiration. It’s what COPDs do when they expire through pursed lips. It can help improve oxygenation by keeping alveoli and small airways open for longer to facilitate gas exchange –ie: improves O2 sats 5cmH2O is a good starting point and can go up to 10cmH2O. But it can cause hypotension in pts who’re volume deplete or unstable, so don’t use it if they are not stable! BACK UP PLAN: Remember – if all else fails and the ventilator won’t work/won’t stop beeping – revert back to your bag mask ventilation! If that’s not working & the pt is still desaturating, then go back to basics to trouble shoot + AND GET HELP! Ensure O2 connection & O2 is on. Bag mask valve is working. -> Is the pt easy or hard to bag? At the mouth : check ETT is not too deep/shallow. AE equal bilaterally. Is it a pneumothorax? Is the ETT down too far? Is there plugging of the ETT? Has the stomach been decompressed with a NGT? As a guide, the default settings ( a good start!) on our Oxylog 3000 are: VT 500mL RR 10 Pmax 40 FiO2 (%) 100 VC SIMV PEEP 5 Psupp 10 Trigger 3L/min I:E (inspiration:expiration) 1:2 These are set on adult disposable tubing.