******* 1
advertisement

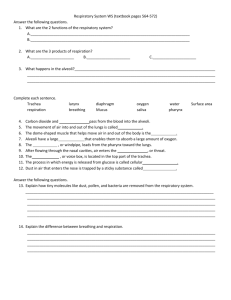
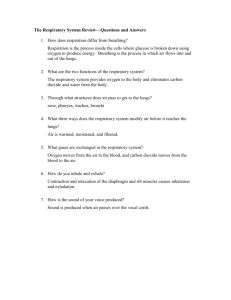
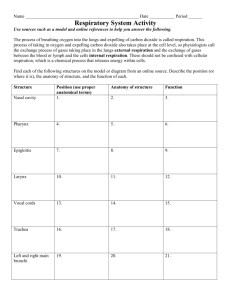
Respiratory System • The major function of the respiratory system is to supply the body with oxygen and dispose of carbon dioxide. To accomplish this function, at least four processes, collectively called respiration, must happen: • 1. Pulmonary ventilation: movement of air into and out of the lungs so that the gases there are continuously changed and refreshed (commonly called breathing). • 2. External respiration: movement of oxygen from the lungs to the blood and of carbon dioxide from the blood to the lungs. • 3. Transport of respiratory gases: transport of oxygen from the lungs to the tissue cells of the body, and of carbon dioxide from the tissue cells to the lungs. This is accomplished by the cardiovascular system using blood as the transporting fluid. • 4. Internal respiration: movement of oxygen from blood to the tissue cells and of carbon dioxide from tissue cells to blood. The respiratory system Respiration is much more than the simple mechanical actions of breathing. Breathing consists of: -Inhalation provides the body with the oxygen that is necessary for the production of ATP in the process of cell respiration. -Exhalation removes the CO2 that is a product of cell respiration. -Breathing also regulates the level of CO2 within the body, and this contributes to the maintenance of the acid–base balance of body fluids. Functional Anatomy of the Respiratory System Functionally, the Respiratory System consists of two zones. The respiratory zone, the actual site of gas exchange, is composed of the respiratory bronchioles, alveolar ducts, and alveoli, (all microscopic structures). The conducting zone includes all other respiratory passageways, which provide fairly rigid canals for air to reach the gas exchange sites. The conducting zone organs also cleanse, humidify, and warm incoming air. Thus, air reaching the lungs has fewer irritants (dust, bacteria, etc.) than when it entered the system, and it is warm and damp. • The respiratory system moves air into and out of the lungs, which are the site of exchange for O2 and CO2 between the air and the blood. • The functioning of the respiratory system depends directly on the proper functioning of the circulatory system. • The respiratory tract consists of two parts 1. The upper respiratory tract consists of those parts outside the chest cavity. 2. The lower respiratory tract consists of those parts within the chest cavity. The nose 1-provides an airway for respiration; 2- warms(many capillaries in submucosa), moistens, and cleanses incoming air; and 3- houses the olfactory receptors that respond to vapors in inhaled air. -The external nose is shaped by bone and cartilage plates. -The nasal cavity, which opens to the exterior, is divided by the nasal septum. -Paranasal sinuses and nasolacrimal ducts drain into the nasal cavities. - The roof of the nasal cavity is formed by the ethmoid and sphenoid bones of the skull. -The floor is formed by the palate, which separates the nasal cavity from the oral cavity below. Anteriorly, where the palate is supported by the maxillary processes and palatine bones, it is called the hard palate. The unsupported posterior portion is the muscular soft palate. -Hairs inside the nostrils block the entry of dust. -Nasal mucosa is ciliated epithelium with goblet cells; surface area is increased by the conchae. - Nasal mucosa warms and moistens the incoming air; dust and microorganisms are trapped on mucus and swept by the cilia to the pharynx. -Paranasal sinuses in the maxillae , frontal , sphenoid, and ethmoid bones open into the nasal cavities: functions are to lighten the skull and provide resonance for the voice. • HOMEOSTATIC IMBALANCE Cold viruses, streptococcal bacteria, and various allergens can cause rhinitis (rini′tis), inflammation of the nasal mucosa accompanied by excessive mucus production, nasal congestion, and postnasal drip. • The nasal mucosa is continuous with that of the rest of the respiratory tract, explaining the typical nose to throat to chest progression of colds. Because the mucosa extends tentacle-like into the nasolacrimal (tear) ducts and paranasal sinuses, nasal cavity infections often spread to those regions, causing sinusitis (inflamed sinuses). • When the passageways connecting the sinuses to the nasal cavity are blocked with mucus or infectious material, the air in the sinus cavities is absorbed. The result is a partial vacuum and a sinus headache localized over the inflamed areas. Pharynx—posterior to nasal and oral cavities 1. Nasopharynx—above the level of the soft palate, which blocks it during swallowing; a passageway for air only. The eustachian tubes from the middle ears open into it. The adenoid is a lymph nodule on the posterior wall. 2. Oropharynx—behind the mouth; a passageway for both air and food. Palatine tonsils are on the lateral walls. Two kinds of tonsils lie embedded in the oropharyngeal mucosa. The paired palatine tonsils and the lingual tonsil . 3. Laryngopharynx—a passageway for both air and food; opens anteriorly into the larynx and posteriorly into the esophagus. HOMEOSTATIC IMBALANCE High on its posterior wall is the pharyngeal tonsil (or adenoids), which traps and destroys pathogens entering the nasopharynx in air. Infected and swollen adenoids block air passage in the nasopharynx, making it necessary to breathe through the mouth. As a result, the air is not properly moistened, warmed, or filtered before reaching the lungs. When the adenoids are chronically enlarged, both speech and sleep may be disturbed. Larynx—the voice box and the airway between the pharynx and trachea 1. Made of nine cartilages; the thyroid cartilage is the largest and most anterior. 2. The epiglottis is the uppermost cartilage; covers the larynx during swallowing. 3. The vocal cords are lateral to the glottis, the opening for air . 4. During speaking, the vocal cords are pulled across the glottis and vibrated by exhaled air, producing sounds that may be turned into speech. 5. The cranial nerves for speaking are the vagus and accessory. -HOMEOSTATIC IMBALANCE Inflammation of the vocal folds, or laryngitis, causes the vocal folds to swell, interfering with their vibration. This produces hoarseness, or in severe cases inability to speak above a whisper. Laryngitis is also caused by overuse of the voice, very dry air, bacterial infections, tumors on the vocal folds, and inhalation of irritating chemicals. -Sphincter Functions of the Larynx *Under certain conditions, the vocal folds act as a sphincter that prevents air passage. During abdominal straining associated with defecation, the glottis closes to prevent exhalation and the abdominal muscles contract, causing the intra-abdominal pressure to rise. These events, collectively known as Valsalva’s maneuver, help empty the rectum and can also splint (stabilize) the body trunk when one lifts a heavy load. Trachea—extends from the larynx to the primary bronchi 1. Sixteen to 20 C-shaped cartilages in the tracheal wall keep the trachea open. 2. Mucosa is ciliated epithelium with goblet cells; cilia sweep mucus, trapped dust, and microorganisms upward to the pharynx. Bronchial Tree—extends from the trachea to the alveoli 1. The right and left primary bronchi are branches of the trachea; one to each lung; same structure as the trachea. 2. Secondary bronchi: to the lobes of each lung (three right, two left) 3. Bronchioles—no cartilage in their walls. HOMEOSTATIC IMBALANCE Smoking inhibits and ultimately destroys cilia, after which coughing is the only means of preventing mucus from accumulating in the lungs. For this reason, smokers with respiratory congestion should avoid medications that prevents cough. HOMEOSTATIC IMBALANCE Many people have suffocated after choking on a piece of food that suddenly closed off their trachea. The Heimlich maneuver, a procedure in which air in the victim’s lungs is used to “pop out,” or expel, an obstructing piece of food, has saved many people. The maneuver is simple ,but cracked ribs are a distinct possibility when it is done incorrectly . The Lungs -The paired lungs occupy all of the thoracic cavity except the mediastinum, which houses the heart, great blood vessels, bronchi, esophagus, and other organs . -The anterior, lateral, and posterior lung surfaces lie in close contact with the ribs and form the continuously curving costal surface. - Just deep to the clavicle is the apex, the narrow superior tip of the lung. The concave, inferior surface that rests on the diaphragm is the base. -On the mediastinal surface of each lung is an indentation, the hilum, through which pulmonary and systemic blood vessels enter and leave the lungs. All conducting and respiratory passageways distal to the main bronchi are found in the lungs. The alveoli—the sites of gas exchange in the lungs -Made of simple squamous epithelium(Alveolar type I); thin to permit diffusion of gases. -Surrounded by pulmonary capillaries, which are also made of simple squamous epithelium -Elastic connective tissue between alveoli is important for normal exhalation. -A thin layer of tissue fluid lines each alveolus . - Alveolar type II cells produce pulmonary surfactant that mixes with the tissue fluid lining to decrease surface tension to permit inflation of the alveoli. -Have efficient alveolar macrophages crawl freely along the internal alveolar surfaces. -Although the number of microorganisms is huge, alveolar surfaces are usually sterile. Most macrophages simply get swept up by the ciliary current of superior regions and carried passively to the pharynx. In this manner, we clear and swallow over 2 million alveolar macrophages per hour! The Respiratory Membrane The walls of the alveoli are composed of a single layer of squamous epithelial cells on a basement membrane. A sheet of tissue paper is much thicker. -The external surfaces of the alveoli are densely covered with a pulmonary capillaries . -Together, the alveolar and capillary walls and their fused basement membranes form the respiratory membrane, a 5-µm-thick air-blood barrier that has gas on one side and blood flowing past on the other -Gas exchanges occur readily by simple diffusion across the respiratory membrane— O2 passes from the alveolus into the blood, and CO2 leaves the blood to enter the gas-filled alveolus. Pleural Membranes( Pleurae) are serous membranes of the thoracic cavity 1. Parietal pleura lines the chest wall. 2. Visceral pleura covers the lungs. Serous fluid between the two layers prevents friction and keeps the membranes together during breathing. • HOMEOSTATIC IMBALANCE -Pleurisy (ploo′rĭ-se), inflammation of the pleurae, results in friction and stabbing pain with each breath. As the disease progresses, the pleurae may produce an excessive amount of fluid that may exert pressure on the lungs and hinder breathing movements. -Other fluids that may accumulate in the pleural cavity include blood (leakage from damaged blood vessels) and blood filtrate (the watery fluid that oozes from the lung capillaries when right-sided heart failure occurs). -The general term for fluid accumulation in the pleural cavity is pleural effusion. Mechanism of Breathing 1. Ventilation is the movement of air into and out of the lungs: inhalation and exhalation. Gases travel from an area of higher pressure to an area of lower pressure. 2. Respiratory centers are in the medulla and pons. 3. Respiratory muscles are the diaphragm and external and internal intercostal muscles . Pressures in the Thoracic Cavity 1-Intrapulmonary pressure is the pressure within the bronchial tree and alveoli; fluctuates during breathing. 2-Intrapleural pressure is the pressure within the pleural cavity; it is always negative (slightly below)relative to intrapulmonary pressures. 3- Atmospheric pressure is air pressure:760 mmHg at sea level. • HOMEOSTATIC IMBALANCE Atelectasis (at″ĕ-lik′tah-sis), or lung collapse, occurs when a bronchiole becomes plugged (as may follow pneumonia). Its associated alveoli then absorb all of their air and collapse. Atelectasis can also occur when air enters the pleural cavity either through a chest wound, or due to rupture of the visceral pleura, which allows air to enter the pleural cavity from the respiratory tract. Pneumothorax ,the presence of air in the intrapleural space .Drawing air out of the intrapleural space with chest tubes, allows the lung to reinflate and resume its normal function. Note that because the lungs are in separate cavities, one lung can collapse without interfering with the function of the other Inhalation (inspiration) 1. Motor impulses from medulla travel along phrenic nerves to diaphragm, which contracts and moves down. Impulses are sent along intercostal nerves to external intercostal muscles, which pull ribs up and out. 2. The chest cavity is expanded and expands the parietal pleura. 3. The visceral pleura adheres to the parietal pleura and is also expanded and in turn expands the lungs. 4. Intrapulmonic pressure decreases, and air rushes into the lungs. Exhalation (expiration) 1. Motor impulses from the medulla decrease, and the diaphragm and external intercostal muscles relax. 2. The chest cavity becomes smaller and compresses the lungs. 3. The elastic lungs recoil and further compress the alveoli. 4. Intrapulmonic pressure increases, and air is forced out of the lungs. Normal exhalation is passive. 5. Forced exhalation: contraction of the internal intercostal muscles pulls the ribs down and in; contraction of the abdominal muscles forces the diaphragm upward. Pulmonary Volumes Measured by Respirometer 1. Tidal volume—the amount of air in one normal inhalation and exhalation. 2. Minute respiratory volume—the amount of air inhaled and exhaled in 1 minute. 3. Inspiratory reserve—the amount of air beyond tidal in a maximal inhalation. 4. Expiratory reserve—the amount of air beyond tidal in the most forceful exhalation. 5. Vital capacity—the sum of tidal volume, inspiratory and expiratory reserves. 6. Residual volume—the amount of air that remains in the lungs after the most forceful exhalation; provides for continuous exchange of gases. • Anatomic dead space—air still in the respiratory passages at the end of inhalation (is normal). Alveolar Surface Tension Surface tension: (1) draws the liquid molecules closer together and (2) resists any force that tends to increase the surface area of the liquid. Because water is the major component of the liquid film that coats the alveolar walls, it is always acting to reduce the alveoli to their smallest possible size. If the film was pure water, the alveoli would collapse between breaths. But the alveolar film contains surfactant (ser-fak′tant), a complex of lipids and proteins produced by the type II alveolar cells. Surfactant decreases the surface tension of alveolar fluid, and discourage alveolar collapse. HOMEOSTATIC IMBALANCE When too little surfactant is present, surface tension forces can collapse the alveoli. Once this happens, the alveoli must be completely reinflated during each inspiration, an effort that uses tremendous amounts of energy. This is the problem faced by newborns with infant respiratory distress syndrome (IRDS), a condition peculiar to premature babies. Since inadequate pulmonary surfactant is produced until the last two months of fetal development, babies born prematurely often are unable to keep their alveoli inflated between breaths. IRDS is treated with positive-pressure respirators that force air into the alveoli, keeping them open between breaths. Spraying natural or synthetic surfactant into the newborn’s respiratory passageways also helps. Nonrespiratory Air Movements Exchange of Gases 1. External respiration is the exchange of gases between the air in the alveoli and the blood in the pulmonary capillaries. 2. Internal respiration is the exchange of gases between blood in the systemic capillaries and tissue fluid (cells). 3. Inhaled air (atmosphere) is 21% O2 and 0.04% CO2. Exhaled air is 16% O2 and 4.5% CO2. 4. Diffusion of O2 and CO2 in the body occurs because of pressure gradients , gas will diffuse from an area of higher partial pressure to an area of lower partial pressure. 5. External respiration: PO2 in the alveoli is high, and PO2in the pulmonary capillaries is low, so O2 diffuses from the air to the blood. PCO2 in the alveoli is low, and PCO2 in the pulmonary capillaries is high, so CO2 diffuses from the blood to the air and is exhaled . 6. Internal respiration: PO2 in the systemic capillaries is high, and PO2 in the tissue fluid is low, so O2 diffuses from the blood to the tissue fluid and cells. PCO2 in the systemic capillaries is low, and PCO2 in the tissue fluid is high, so CO2 diffuses from the tissue fluid to the blood . Transport of Oxygen in the Blood 1. Oxygen is carried by the iron of hemoglobin (Hb) in the RBCs. The O2–Hb bond is formed in the lungs where the PO2 is high. 2. In tissues, Hb releases much of its O2; the important factors are low PO2 in tissues, high PCO2 in tissues, and a high temperature in tissues. 3. Oxygen saturation of hemoglobin (SaO2) is 95% to 97% in systemic arteries and averages 70% to 75% in systemic veins. • Oxygen is carried in blood in two ways: 1-bound to hemoglobin within red cells(main way) and 2-dissolved in plasma • Because the iron atoms bind oxygen, each hemoglobin molecule can combine with four molecules of O2, and oxygen loading is rapid and reversible. • The hemoglobin-oxygen combination, called oxyhemoglobin (ok″sĭ-he″mo-glo′bin), is written HbO2. Hemoglobin that has released oxygen is called reduced hemoglobin, or deoxyhemoglobin, and is written HHb. Loading and unloading of O2 can be indicated by a single reversible equation: Carbon Dioxide Transport Normally active body cells produce about 200 ml of CO2 each minute—exactly the amount excreted by the lungs. Blood transports CO2 from the tissue cells to the lungs in three forms : • 1. Dissolved in plasma (7–10%). The smallest amount of CO2 is transported simply dissolved in plasma. • 2. Chemically bound to hemoglobin (just over 20%). In this form, CO2 is carried in the RBCs as carbamino- hemoglobin . • Because carbon dioxide binds directly to the amino acids of globin (and not to the heme), carbon dioxide transport in RBCs does not compete with the oxyhemoglobin transport mechanism. • CO2 loading and unloading to and from Hb are directly influenced by the PCO2. - Carbon dioxide rapidly dissociates from hemoglobin in the lungs, where the PCO2 of alveolar air is lower than that in blood. - Carbon dioxide is loaded in the tissues, where the PCO2 is higher than that in the blood. 3. As bicarbonate ion in plasma (about 70%). Most carbon dioxide molecules entering the plasma quickly enter the RBCs, where it combines with water, forming carbonic acid (H2CO3). H2CO3 is unstable and quickly dissociates into hydrogen ions and bicarbonate ions which is carried in plasma: Nervous Regulation of Respiration 1. The medulla contains the inspiration center and expiration center. 2. Impulses from the inspiration center to the respiratory muscles cause their contraction; the chest cavity is expanded. 3. Baroreceptors in lung tissue detect stretching and send impulses to the medulla to depress the inspiration center. This prevents overinflation of the lungs. 4. In the pons: the apneustic center and the pneumotaxic center work with the inspiration center in the medulla to produce a normal breathing rhythm. 5- The cerebral cortex permits voluntary changes in breathing. 6. The hypothalamus influences changes in breathing in emotional situations. 7. Coughing and sneezing remove irritants from the upper respiratory tract; the centers for these reflexes are in the medulla. Chemical Regulation of Respiration 1. Decreased blood O2 is detected by chemoreceptors in the carotid body and aortic body leading to increased respiration to take more air into the lungs. 2. Increased blood CO2 level is detected by chemoreceptors in the medulla leading to increased respiration to exhale more CO2. 3. Increased CO2 (low pH)is the major regulator of respiration 4. Oxygen becomes a major regulator of respiration when blood level is very low, as may occur with severe, chronic pulmonary disease. Respiration and Acid–Base Balance 1. Respiratory acidosis: a decrease in the rate or efficiency of respiration permits excess CO2 to accumulate in body fluids, resulting in the formation of excess H+ ions, which lower pH. Occurs in severe pulmonary disease. 2. Respiratory alkalosis: an increase in the rate of respiration increases the CO2 exhaled, which decreases the formation of H+ ions and raises pH. Occurs during hyperventilation or when first at a high altitude. 3. Respiratory compensation for metabolic acidosis: increased respiration to exhale CO2 to decrease H+ ion formation to raise pH to normal. 4. Respiratory compensation for metabolic alkalosis: decreased respiration to retain CO2 to increase H+ ion formation to lower pH to normal. Related Clinical Terms • Adenoidectomy (adenotonsillectomy): Surgical removal of an infected pharyngeal tonsil (adenoids). • Aspiration: (1) The act of inhaling or drawing something into the lungs or respiratory passages. Pathological aspiration in which vomit or excessive mucus is drawn into the lungs may occur when a person is unconscious or anesthetized; turning the head to one side is preventive. (2) Withdrawal of fluid by suction (use of an aspirator); done during surgery to keep an area free of blood or other body fluids; mucus is aspirated from the trachea of tracheotomy patients. • Bronchoscopy: (scopy = viewing) Use of a viewing tube inserted through the nose or mouth to examine the internal surface of the main bronchi in the lung. Forceps attached to the tip of the tube can remove trapped objects or take samples of mucus for examination. • Epistaxis: (epistazo = to bleed at the nose) Nosebleed; commonly follows trauma to the nose or excessive nose blowing. Most nasal bleeding is from the highly vascularized anterior septum and can be stopped by pinching the nostrils closed or packing them with cotton. • Cheyne-Stokes breathing: Abnormal breathing pattern sometimes seen just before death and in people with combined neurological and cardiac disorders. It consists of bursts of tidal volume breaths (increasing and then decreasing in depth) alternating with periods of apnea. • Deviated septum Condition in which the nasal septum takes a more lateral course than usual and may obstruct breathing; often manifests in old age or from nose trauma. • Endotracheal tube: A thin plastic tube threaded into the trachea through the nose or mouth; used to deliver oxygen to patients who are breathing inadequately, in a coma, or under anesthesia. • Orthopnea: (ortho = straight, upright) Inability to breathe in the horizontal (lying down) position. • Otorhinolaryngology: (oto = ear; rhino = nose) Branch of medicine that deals with diagnosis and treatment of diseases of the ears, nose, and throat. • Pneumonia: Infectious inflammation of the lungs, in which fluid accumulates in the alveoli; the seventh most common cause of death in the United States. Most of the more than 50 different varieties of pneumonia are viral or bacterial. • Pulmonary embolism: Obstruction of the pulmonary artery or one of its branches by an embolus (most often a blood clot that has been carried from the lower limbs and through the right side of the heart into the pulmonary circulation). Symptoms are chest pain, productive bloody cough, tachycardia, and rapid, shallow breathing. Can cause sudden death unless treated quickly . • Stuttering A problem of voice production in which the first syllable of words is repeated in “machinegun” fashion. Primarily a problem with neural control of the larynx and other voice-producing structures. • Sudden infant death syndrome (SIDS): Unexpected death of an apparently healthy infant during sleep. Commonly called crib death, SIDS is one of the most frequent causes of death in infants under 1 year old. Believed to be a problem of immaturity of the respiratory control centers. Most cases occur in infants placed in a prone position (on their abdomen) to sleep—a position which may result in hypoxia and hypercapnia due to rebreathing exhaled (CO2-rich) air. • Tracheotomy: Surgical opening of the trachea; done to provide an alternate route for air to reach the lungs when more superior respiratory passageways are obstructed (as by food or a crushed larynx).