Glycogen Storage Diet
advertisement

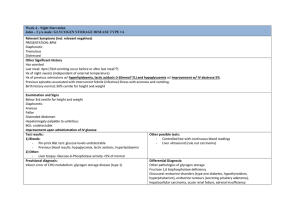
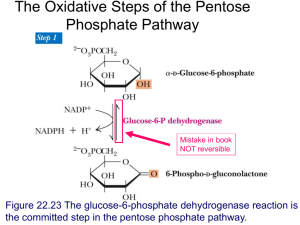
Diet Instruction- Glycogen Storage Disease What is Glycogen Storage Disease/Etiology? o Type I Glycogen Storage Disease accounts for about 25% of all cases of GSD diagnosed in the USA and in Europe and has an estimated incidence of about 1 in 100,000 live births o Considered a metabolic disorder and are genetically linked o All types of GSD cause the body to either not be able to make enough glucose, or not be able to use glucose as a form of energy which results in an enlargement of the liver o Individuals with Type I Glycogen Storage Disease are unable to release glucose from glycogen mainly in the liver o They cannot maintain their blood glucose (sugar) levels and within a few hours after eating they will develop hypoglycemia (low blood sugar) The low levels of glucose in the blood of these individuals often result in chronic hunger, fatigue, and irritability. These symptoms are especially noticeable in infants. Symptoms of hypoglycemia often appear when the time between feedings increases and the infant sleeps through the night o Since people with Type I GSD are able to store glucose as glycogen but not able to release it normally, with time the stores of glycogen build up in the liver causing the liver to swell (hepatomegaly) o This is much like being able to place groceries from the store into your kitchen cabinets, but not being able to get the food out of the cabinets when needed o Levels of hormones, lactic acid, triglycerides, lipids (fats), uric acid and other by-products of metabolism increase in the blood as the body tries to raise blood sugar o Fats get stored in the liver along with the glycogen, which leads to the enlargement of the liver o The liver does its many other functions normally, and there is not usually any evidence of liver failure o The kidneys are also enlarged due to increased glycogen storage. Diagnostic Measures Based on clinical presentation, abnormal blood/plasma concentrations of glucose, lactate, uric acid, triglycerides, and lipids, genetic testing, and a liver biopsy to measure glucose-6-phosphatase enzyme activity. The lack of glucose-6-phosphate translocase activity in the liver leads to inadequate conversion of glucose-6-phosphate into glucose through normal glycogenolysis and gluconeogenesis, resulting in the following: o Hypoglycemia. Fasting blood glucose concentration lower than 60 mg/dL (reference range: 70-120 mg/dL) o Lactic acidosis. Blood lactate higher than 2.5 mmol/L (reference range: 0.5-2.2 mmol/L) o Hyperuricemia. Blood uric acid higher than 5.0 mg/dL (reference range: 2.0-5.0 mg/dL) o Hyperlipidemia Triglycerides higher than 250 mg/dL (reference range: 150-200 mg/dL). Hypertriglyceridemia causes the plasma to appear "milky." Cholesterol higher than 200 mg/dL (reference range: 100-200 mg/dL) Glucose-6-phosphatase (G6Pase) catalytic activity. The normal G6Pase enzyme activity level in liver is 3.50±0.8 µmol/min/g tissue: o In most individuals with GSDIa, the G6Pase enzyme activity is lower than 10% of normal. Mutations in G6PC account for approximately 80% of GSDI. Mutations in SLC37A4 account for approximately 20% of GSDI. Treatment o Dietary modifications are the preferred method of management o TPN through continuous nasogastric infusions of glucose to correct metabolic abnormalities will be needed with frequent daytime oral feedings to correct metabolic abnormalities due to recent fasting state o Frequent glucose feedings will need to maintained for life o Things to remember: o Frequent, oral feedings throughout the day Need to maintain blood glucose above 70 mg/dL Two thirds of calories should be given during the daytime to allow for even distribution of carbohydrate over a 24 hour period Calories should be mostly from carbohydrate (60-70%) One third of calories should be given over night, primarily from a carbohydrate source, such as corn starch or tube feeding Foods that contain high amount of cornstarch should be eaten between meals to keep blood glucose level and can be used as the glucose source over night as she gets older If food is not eaten for two to four hours, blood glucose levels drop to a low level, leading to serious health problems such as seizures, poor growth, enlarged liver, high levels of some fats circulating in the blood, and high levels of uric and lactic acids in the blood. o High in complex carbohydrates Restriction of simple sugars translates to no fruit, juice, table sugar, cake, pie, syrup, jelly, honey, and candy; and limited amounts of dairy foods including milk, yogurt and cheese Prognosis o Most patients diagnosed at an early age and that maintain good dietary control reach adulthood o Long term complications include nephropathy, hepatic adenomas, hepatocellular carcinoma, osteoporosis, anemia, pulmonary hypertension, acute pancreatitis, and polycystic ovaries. o Liver transplant is the only cure, but the likely-hood of the procedure and the magnitude of the procedure make this prognosis rare. References Glycogen Storage Disease Type I - GeneReviews - NCBI Bookshelf. (2006, April 19). National Center for Biotechnology Information. Retrieved February 5, 2012, from http://www.ncbi.nlm.nih.gov/books/NBK1312/ Nelms, M. N. (2011). Nutrition therapy and pathophysiology (2nd ed.). Belmont, CA: Wadsworth, Cengage Learning. Type I: von Gierke. (2006, October 1). The Association for Glycogen Storage Disease. Retrieved February 4, 2012, from http://www.agsdus.org/html/typeivongierke.htm